Abstract
Background
In an attempt to improve the treatment of patients with acute coronary syndromes (ACS), a network of certified chest pain units (CPUs) has been recently established in Germany.
Methods
Data from patients admitted between December 2008 and September 2011 for ACS in 40 certified CPUs participating in the registry were prospectively collected.
Results
A total of 5,457 patients was admitted for ACS; 798 patients (14.6 %) were diagnosed with an ST-elevation myocardial infarction (STEMI), 2,244 (41.1 %) with a non-ST-elevation myocardial infarction (NSTEMI), and 2,415 (44.3 %) with unstable angina. The mean time to first medical contact was 2:08 h for STEMI patients. A pre-hospital ECG was available in 23.8 % of all ACS patients. Importantly, evidence of ST-segment elevation was present in 79.7 % of the STEMI patients already in this pre-hospital ECG. As many as 76.6 % of the patients, independently of their symptoms and final diagnosis, received an ECG within 10 min of reaching the CPU. 98.2 % of STEMI patients underwent invasive diagnostics, with an in-hospital delay as little as 31 (11–75) min.
Conclusion
The establishment of a nation-wide network of certified CPUs optimizes the medical treatment of patients with ACS while providing an ideal infrastructure to evaluate and improve, both on a nation-wide and a single center scale, the adherence to guidelines. The median delay between symptom onset and first medical contact remains high. Although performed relatively rarely, a pre-hospital ECG facilitates earlier diagnosis of a STEMI in a large majority of patients. The introduction of CPUs minimizes in-hospital delays and exploits the benefit of invasive diagnostics and treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute chest pain is one the most frequent complaints of patients contacting emergency services [1]. Although the differential diagnosis of chest pain may be complex, timeliness and accuracy are of paramount importance in this setting; in ST-segment elevation myocardial infarction (STEMI) patients, it has been consistently demonstrated that early reperfusion is an important determinant of patient outcome, and current guidelines emphasize the need “to make every effort to minimize all time delays, especially within the first 2 h after onset of symptoms, by the implementation of a system of care network” [2]. Conversely, inappropriate discharge of patients with acute coronary syndromes (ACS) is associated with increased mortality and morbidity [3, 4].
Despite significant improvements in diagnostic and therapeutic strategies, the outcome of patients with suspected ACS remains suboptimal. Registry studies of patients with presumed myocardial infarction or ACS report 1-month overall mortality rates as high as 50 %, and about one half of these deaths occur within the first 2 h [5]. For patients admitted to traditional emergency departments, the incidence of death and recurrent myocardial infarction within the hospital stay following a diagnosis of non-ST-elevation myocardial infarction (NSTEMI) has been reported to be in the range of 10 %, and the 1-year mortality is comprised between 15 and 25 % despite the implementation of guidelines and the systematic use of invasive strategies [6, 7]. Importantly, technological and pharmacological developments have lead to a significant decrease in in-hospital mortality, whereas pre-hospital mortality has changed little over the last years [8].
In order to address this problem, the concept of a unit dedicated to the diagnosis and treatment of acute chest pain has been introduced in countries such as the United States and United Kingdom. The mission of these specialized emergency units is to allow a more systematic approach to differential diagnosis of chest pain, thus optimizing the treatment of patients with ACS [9]. Chest pain units (CPUs) have been rapidly introduced in many centers in the US and the UK, although some argue that this process has occurred at times “in a disorganized way” [10]. Several studies comparing the outcome of patients treated in a traditional emergency ward versus settings where a CPU was available revealed that the existence of a CPU is associated with a more effective diagnosis and a improved clinical outcomes [9, 11]. In particular, the establishment of CPUs in the US reduced the percentage of patients who were discharged before receiving appropriate treatment and was also cost saving, mostly due to the prevention of complications and unnecessary admissions in this subset of patients [12].
Based on these findings, the German Cardiac Society implemented a certification process aimed at maintaining elevated and uniform standards of care in the rapidly enlarging CPU network. Between September 2008 and October 2011, a total of 132 CPUs were certified [13, 14]. Beyond improved patient care, this network provides a platform for the collection of real-world data on the diagnosis and treatment of ACS in Germany.
Materials and methods
The German CPU network
The German CPU network consists of CPUs across the country which meet or exceed quality-of-care measures defined by the German Cardiac Society [14]. Certification is awarded to those CPUs which fulfill a set of minimum requirements and successfully complete the certification process by an expert committee of the German Society of Cardiology. Within this framework, CPUs plan and organize the delivery of care in a systematic manner. The introduction of additional “best practice” recommendations (for instance, the introduction of 17-lead ECG) furthers development and innovation while guaranteeing a minimum standard throughout the network. More details on the nature of the CPU network and on the procedures followed are described in [15].
Definitions
Consecutive patients admitted for chest pain to one of the CPUs throughout Germany were prospectively enrolled. The criteria for German CPUs include a minimum requirement of biomarkers assays at admission and 6–9 h thereafter; an additional ECG + biomarker assessment 3 h after admission is considered an additional recommendation. ACS were classified as STEMI, NSTEMI, or unstable angina (UA). STEMI was diagnosed if the electrocardiogram at admission or by the emergency physician showed an ST-elevation above 0.1 mV in at least two contiguous leads or (previously unknown) left bundle branch block and typical clinic. The diagnosis of NSTEMI was made in the absence of ST elevations when at least one cTn assay exceeded the 99th percentile with a rise and or fall on subsequent samples. UA was diagnosed in the absence of a cTn elevation in a patient with suspected ACS due to clinical presentation (rest angina, severe angina, new onset or crescendo angina) with ECG evidence of myocardial ischemia (ST-segment depression >1 mm in ≥2 ECG leads without elevated troponin or CK-MB) at rest, abnormal exercise testing or in the presence of a significant coronary stenosis on coronary angiography.
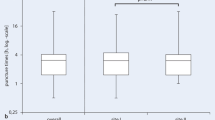
Statistical analysis
The median, with lower and upper quartiles (in brackets), is used as measures of location and dispersion for metrical variables. Categorical variables are described by absolute frequencies and percentages (Tables 1, 2).
Statistical tests were performed in addition to descriptive comparisons between three subgroups of patients with the diagnosis STEMI, NSTEMI, or UA. The classical (Pearson’s) Chi-square test for dichotomous variables and a Kruskal–Wallis rank test for metrically scaled variables were used. Differences were considered significant if the test for one variable rejected the null hypothesis (of no difference between the three subgroup distributions) on a significance level of 0.05. This level applies to each hypothesis (i.e., variable) individually, without adjustment for multiple testing. Resulting empirical significance levels (P values) are added to the descriptive statistics (Tables 1, 2).
All statistical computations were done using SAS®, version 9.2 (SAS Institute Inc., Cary, NC, USA.).
Results
Baseline characteristics
A total of 5,457 patients were admitted to one of the CPUs from December 2008 to September 2011 with a diagnosis of ACS. Table 1 shows the baseline characteristics of these patients. 1,832 (33.6 %) were females, median age was 68.7 (57.4–76.4) years and median body mass index was 27.2 (24.7–30.2) kg/m2.
798 patients (14.6 %) received a final diagnosis of STEMI, 2,244 (41.1 %) were diagnosed with NSTEMI, and 2,415 (44.3 %) with UA. The prevalence of diabetes mellitus, chronic kidney failure, hyperlipidemia, arterial hypertension, and of a positive family history for coronary artery disease was significantly higher in NSTEMI and UA patients than for STEMI patients (P < 0.0001 for the comparison across groups; Table 1), while active smoking was significantly more prevalent in patients presenting with a STEMI (P < 0.0001; Table 1). Similarly, patients with NSTEMI and UA were older, more frequently female, and had a higher prevalence of prior myocardial infarction (all P < 0.0001), stroke or peripheral arterial disease (both P < 0.05). This difference in the previous cardiovascular history was also reflected in a larger prior use of aspirin in NSTEMI and UA patients (P < 0.0001) although only 20 % were taking aspirin versus ~60 % with history of cardiovascular disease.
Clinical presentation
Chest pain was the most frequent symptom (92.2 % of all patients), followed by dyspnea (26.3 %). Chest pain was the predominant clinical manifestation in STEMI patients (95.5 %), and it was slightly less frequent in NSTEMI and UA patients (respectively, 87.8 and 95.1 %, P < 0.0001). In contrast, dyspnea was more frequent in NSTEMI and UA patients (27.7 and 26.5 %) than in STEMI patients (22.0 %, P < 0.01). The first medical contact was the family physician in as many as 17.4 % of the patients with STEMI, and even more frequently in NSTEMI (21.2 %) and UA patients (22.5 %, P < 0.01). 14.1, 19.2 and 31.1 %, respectively, of the patients reached the CPU on their own (P < 0.01) and only 55.2, 37.6 and 42.6 % (P < 0.0001) of the patients called the emergency services.
Pre-hospital and in-hospital diagnosis (Table 2)
Given the importance of early diagnosis and treatment, a pre-hospital ECG is recommended by STEMI guidelines [2]. A pre-hospital ECG (whether performed by a family physician or emergency staff) was available in 23.8 % of the overall ACS population, and in 42.9 % of STEMI patients. Confirming the (unexploited) importance of pre-hospital ECG in shortening the time delay to diagnosis and treatment, as many as 79.7 % STEMI patients showed ST-elevation in this ECG and an additional 3.1 % showed a left bundle branch pattern, while only 10.9 % showed ST-depression or T-wave inversion. Thus, ECG was diagnostic for ischemia from the very early phase in the large majority of STEMI patients. In contrast, ECGs (both pre- and in-hospital) were not diagnostic for ischemia in a large percentage of patients with NSTEMI and UA (65.0 and 77.7 %, respectively).
Upon reaching the CPU, the median time to first ECG was 5 (3–10) min, and 76.6 % of the ECGs were performed and read within 10 min of admission. A cardiac ultrasound was available in 78.8 %, and as many as 84.5 % (98.2 % of those with STEMI) underwent cardiac catheterization.
Troponin (T, I or high-sensitive troponin T) were assayed in 4,759 patients (87.2 %). Blood was collected in 642 STEMI patients (80.5 %). Importantly, this value was negative in as many as 38.5 % of the cases.
Pre-hospital and in-hospital time delays in STEMI patients
The time to first medical contact after symptom onset was 128 (48–720) min in STEMI patients. Only 8.9 % of these patients contacted a physician within 60 min of symptom onset.
The median time between medical contact and admission to the hospital was 58 (35–118) min, and the median time between admission to the hospital and invasive diagnosis (door to needle) was 31 (11–75) min, i.e., a total “first medical contact to needle” time of 95 (60–195) min. As many as 47.8 and 61.7 %, respectively, of the patients reached a catheterization laboratory within 90 and 120 min, respectively, of symptom onset. Overall, the median time interval between symptom onset and arrival in the catheterization laboratory was 322 (149–1,338) min. STEMI were classified as “emergency” (immediate access to catheterization laboratory) in 93 % of the cases, and as “urgent” (catheterization on the next working day) in a remaining 5.7 %.
Therapy of STEMI patients
The large majority of patients received aspirin (91.4 %), heparin (82.5 % unfractionated heparin, 13.7 % low-molecular weight) and clopidogrel or prasugrel, with a larger use of these drugs in STEMI than in NSTEMI and UA patients. Since the data were collected prior to the publication of the most recent NSTEMI-ACS guidelines, clopidogrel was more frequently used than prasugrel, and ticagrelor was not yet available. The use of GpIIb/IIIa inhibitors in the CPU was relatively less common (26.7 %). Fibrinolytic therapy was administered to only 2.5 % of all STEMI patients. PCI was performed in 90 % of the patients with STEMI, 60 % of those with NSTEMI, and 33 % of those with unstable angina (Fig. 1).
Discussion
While only 10–15 % of the patients presenting to the hospital with chest pain have an ACS [3], a rapid and accurate differential diagnosis in this setting has a profound impact on their prognosis. Data from single center experiences demonstrate that the establishment of CPUs specifically dedicated to this subset of patients is associated with improved health care [11, 16]. However, it remains less well explored how this strategy performs on a nation-wide scale. In order to provide a structured approach to this problem, the German Society of Cardiology developed in 2008 a standardized certification system for CPUs [13, 14]. Specific aims of this CPU network are to reduce pre- and in-hospital delays, limit inappropriate discharge of ACS patients and avoid unnecessary hospitalizations for non-ACS patients while reducing unnecessary costs [17]. Within the framework of this initiative, a “nation-wide German CPU Registry” was established.
The first results of the CPU registry
Clinical presentation, diagnostic and therapeutic procedures
In contrast with earlier publications reporting a larger proportion of ST-elevation infarctions [18–21], NSTEMI and UA were by far the most frequent diagnoses in our population. This might in part be explained by the fact that reference values for troponin levels have been progressively lowered within the last years (resulting in a higher number of patients being classified as NSTEMI). Further, many STEMI patients by-pass the CPU and are transported to the catheterization laboratory resulting in the underreporting of these patients in a CPU registry. A third explanation should, however, be considered. Patients diagnosed with NSTEMI and UA presented significantly more often with atypical symptoms (dyspnea rather than angina), and had a non-diagnostic ECG in more than two-thirds of the cases. In contrast to STEMI, repeated ECGs and systematic laboratory investigations are thus necessary for these diagnoses, and without a structured diagnostic algorithm (comprehensive of stress ECG, cardiac ultrasound, laboratory markers and, when indicated, coronary angiography), a significant proportion of NSTEMI and UA patients is systematically missed, with negative prognostic implications [22, 23]. Thus, the difference in the distributions of STEMI, NSTEMI and UA as compared to previous reports might partially reflect the diagnostic accuracy of the CPU model, in which ECG (within 10 min of admission), cardiac ultrasound and cardiac catheterization were performed in >75 % of the patients. Finally, the systematic inclusion of 17-lead ECGs might further change these relationships. 17-lead ECGs have been introduced in the CPU certification as “additional recommendations” since recently. It is possible that the systematic implementation of this method might increase the proportion of STEMIs otherwise undiagnosed.
Early availability of an ECG accelerates decision-making, limits in-hospital delays and increases the success rate of reperfusion therapies [24–27]. Only 23.8 % of our patients received a pre-hospital ECG. These data emphasize the importance of pre-hospital diagnosis and transfer strategies and identifies a weakness in our system, and an issue to be addressed in the future. In contrast, demonstrating the efficacy of the CPU as a tool to implement guidelines, an ECG was available within 10 min of admission to the CPU in as many as 76.6 % of the patients, regardless of their final diagnosis and clinical presentation. This figure represents a significant improvement compared to “standard” emergency room treatment [28]. The advantage of early ECG recordings is evident when one considers the proportion of patients who can be diagnosed in this early stage. Notably, as many as 80 % of the patients with STEMI showed evidence of ST-elevation in the ECG recorded by ambulance staff: while being performed in less than a quarter of all ACS patients, a pre-hospital ECG allows early diagnosis in the large majority of the cases. The present data also confirm the concept that “one should not wait for the results (of cardiac blood markers) to initiate reperfusion treatment” [2]. Indeed, as many as 38.5 % of the patients with STEMI had normal troponin levels at admission. While markers of necrosis may be helpful in deciding between an early invasive or a more conservative strategy in selected cases, reliance on these biomarkers in the early diagnosis of ACS carries a substantial risk of false negative results (and causes an unnecessary time delay).
Our data also confirm the concept that the availability of a CPU allows early and effective treatment of ACS and the exploitation of invasive strategies. Overall, the median time from first medical contact to catheterization was 95 min in STEMI patients, which is in line with guidelines for optimal treatment [2] and well below the maximum acceptable percutaneous revascularization-related time delay as compared to fibrinolytic therapy [29–32]; the timeliness of first in-hospital ECG and the availability of PCI facilities thus partially compensated for the low rate of pre-hospital ECGs. Several other reasons explain the very low use of fibrinolytic therapy in the German CPU network [33, 34]. First, since the major time delay was between symptom onset and first medical contact, given the availability of 24-h PCI facilities, a more systematic use of fibrinolysis would have not shortened the time to effective reperfusion. Further, as described above, patients with STEMI generally by-pass the CPU and are directed to the catheterization laboratory. Therefore, STEMI patients included in the present registry generally received a first diagnosis while already in-hospital (e.g., no pre-hospital ECG available, false negative diagnosis by the emergency physician, new ST-elevation, self referrals to the CPU, etc.) and could therefore be directly transferred to the catheterization laboratory with no extra delay.
Similar to large registries [18, 21, 35–38], the use of aspirin and heparins was in the range of 90 %, while that of clopidogrel and IIb/IIIa inhibitors remained low [39]. The introduction of new medications and new lines of evidence regarding the importance of antiplatelet therapy will probably lead to a broader use of these drugs in the future [40].
Time delay in STEMI
The time between symptom onset and reperfusion is a central determinant of patients’ prognosis in the setting of STEMI [29, 41, 42]. In the present dataset, the median time between symptom onset and admission to the CPU in STEMI patients was approximately 4 h. Notably, the largest component of this delay was the interval between symptom onset and first medical contact, data that is in line with recent reports showing a worryingly trend towards an increase, rather than decrease, in this time interval [17]. In contrast, in-hospital time delays demonstrate the efficiency of the CPU system and compare favorably with those of other studies such as the EHS-ACS-I and II registry (angiography rate of 56.3 and 70.2 % respectively, door-to-balloon time of 93 and 70 min, respectively) [18, 35].
While in-hospital protocols appear to be effective, more efforts have to be invested in reducing the time interval between symptom onset and hospital admission. Recent data from regional and supra-regional networks demonstrate that this can partially be addressed by establishing a formalized data feedback on the treatment times and patient outcome between hospitals and emergency services [43].
Conclusions
The present data provide a nationwide perspective on the current treatment of ACS in Germany. Our data reinforce the importance of structured and time-efficient strategies for the early (pre-hospital) diagnosis of STEMI and to avoid under-reporting of NSTEMI and UA. Further, they emphasize the existence of significant issues, principally a time delay between symptom onset and first medical contact. Taken together, the data on the performance of medical procedures in the CPU are encouraging and demonstrate, along with the introduction of more sensitive markers [44–46], the effectiveness of CPUs as a strategy to achieve several crucially important goals; early diagnosis of STEMI, thorough evaluation of NSTEMI and UA, facilitated access to interventional therapy, and identification of weaknesses to be addressed.
References
Barish RA, Doherty RJ, Browne BJ (1997) Reengineering the emergency evaluation of chest pain. J Healthc Qual 19:6–12 (quiz 60)
Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, Filippatos G, Fox K, Huber K, Kastrati A, Rosengren A, Steg PG, Tubaro M, Verheugt F, Weidinger F, Weis M (2008) Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the task force on the management of st-segment elevation acute myocardial infarction of the European Society of Cardiology. Eur Heart J 29:2909–2945
Pope JH, Aufderheide TP, Ruthazer R, Woolard RH, Feldman JA, Beshansky JR, Griffith JL, Selker HP (2000) Missed diagnoses of acute cardiac ischemia in the emergency department. N Engl J Med 342:1163–1170
Zobel C, Dörpinghaus M, Reuter H, Erdmann E (2012) Mortality in a cardiac intensive care unit. Clin Res Cardiol 101(7):521–524
Tunstall-Pedoe H, Kuulasmaa K, Mahonen M, Tolonen H, Ruokokoski E, Amouyel P (1999) Contribution of trends in survival and coronary-event rates to changes in coronary heart disease mortality: 10-year results from 37 WHO MONICA project populations. Monitoring trends and determinants in cardiovascular disease. Lancet 353:1547–1557
Bauer T, Koeth O, Junger C, Heer T, Wienbergen H, Gitt A, Zahn R, Senges J, Zeymer U (2007) Effect of an invasive strategy on in-hospital outcome in elderly patients with non-ST-elevation myocardial infarction. Eur Heart J 28:2873–2878
Vogel B, Hahne S, Kozanli I, Kalla K, Jarai R, Freynhofer M, Smetana P, Nürnberg M, Geppert A, Unger G, Huber K (2011) Influence of updated guidelines on short- and long-term mortality in patients with non-ST-segment elevation acute coronary syndrome (NSTE-ACS). Int J Cardiol [Epub ahead of print]
Goldberg RJ, Glatfelter K, Burbank-Schmidt E, Lessard D, Gore JM (2006) Trends in community mortality due to coronary heart disease. Am Heart J 151:501–507
Bahr RD (2002) The chest pain center strategy for delivering community heart attack care by shifting the paradigm of heart attack care to earlier detection and treatment. Prev Cardiol 5:16–22
Cross E, How S, Goodacre S (2007) Development of acute chest pain services in the UK. Emerg Med J 24:100–102
Keller T, Post F, Tzikas S, Schneider A, Arnolds S, Scheiba O, Blankenberg S, Munzel T, Genth-Zotz S (2010) Improved outcome in acute coronary syndrome by establishing a chest pain unit. Clin Res Cardiol 99:149–155
Goodacre S, Dixon S (2005) Is a chest pain observation unit likely to be cost effective at my hospital? Extrapolation of data from a randomised controlled trial. Emerg Med J 22:418–422
Breuckmann F, Post F, Giannitsis E, Darius H, Erbel R, Görge G, Heusch G, Jung W, Katus H, Perings S, Senges J, Smetak N, Münzel T (2008) Unit FdTFCP. Kriterien der deutschen gesellschaft für kardiologie—herz- und kreislaufforschung für “chest-pain-units”. Der Kardiologe 2:389–394
Breuckmann F, Post F, Erbel R, Munzel T (2009) Acute thoracic pain: chest pain unit—the certification campaign of the German Society of Cardiology. Herz 34:218–223
Post F, Gori T, Senges J, Giannitsis E, Katus H, Munzel T (2012) Establishment and progress of the chest pain unit certification process in Germany and the local experiences of Mainz. Eur Heart J 33:682–686
Tzikas S, Keller T, Post F, Blankenberg S, Genth-Zotz S, Munzel T (2010) Patient satisfaction in acute coronary syndrome. Improvement through the establishment of a chest pain unit. Herz 35:403–409
Senges J, Schiele R (2004) Prehospital delay-not just a question of patient knowledge. Z Kardiol 93(Suppl 1):I16–I18
Hasdai D, Behar S, Wallentin L, Danchin N, Gitt AK, Boersma E, Fioretti PM, Simoons ML, Battler A (2002) A prospective survey of the characteristics, treatments and outcomes of patients with acute coronary syndromes in Europe and the Mediterranean basin; the Euro Heart Survey of acute coronary syndromes (Euro Heart Survey ACS). Eur Heart J 23:1190–1201
Allen LA, O’Donnell CJ, Camargo CA Jr, Giugliano RP, Lloyd-Jones DM (2006) Comparison of long-term mortality across the spectrum of acute coronary syndromes. Am Heart J 151:1065–1071
Dougan JP, Mathew TP, Riddell JW, Spence MS, McGlinchey PG, Nesbitt GS, Smye M, Menown IB, Adgey AA (2001) Suspected angina pectoris: a rapid-access chest pain clinic. QJM 94:679–686
Fox KA, Goodman SG, Klein W, Brieger D, Steg PG, Dabbous O, Avezum A (2002) Management of acute coronary syndromes. Variations in practice and outcome; findings from the Global Registry of Acute Coronary Events (GRACE). Eur Heart J 23:1177–1189
Maddox TM, Reid KJ, Rumsfeld JS, Spertus JA (2007) One-year health status outcomes of unstable angina versus myocardial infarction: a prospective, observational cohort study of ACS survivors. BMC Cardiovasc Disord 7:28
Armstrong PW, Fu Y, Chang WC, Topol EJ, Granger CB, Betriu A, Van de Werf F, Lee KL, Califf RM (1998) Acute coronary syndromes in the GUSTO-IIb trial: prognostic insights and impact of recurrent ischemia. The GUSTO-IIb investigators. Circulation 98:1860–1868
Brown JP, Mahmud E, Dunford JV, Ben-Yehuda O (2008) Effect of prehospital 12-lead electrocardiogram on activation of the cardiac catheterization laboratory and door-to-balloon time in ST-segment elevation acute myocardial infarction. Am J Cardiol 101:158–161
Ferguson JD, Brady WJ, Perron AD, Kielar ND, Benner JP, Currance SB, Braithwaite S, Aufderheide TP (2003) The prehospital 12-lead electrocardiogram: impact on management of the out-of-hospital acute coronary syndrome patient. Am J Emerg Med 21:136–142
Kudenchuk PJ, Maynard C, Cobb LA, Wirkus M, Martin JS, Kennedy JW, Weaver WD (1998) Utility of the prehospital electrocardiogram in diagnosing acute coronary syndromes: the myocardial infarction triage and intervention (MITI) project. J Am Coll Cardiol 32:17–27
Myers RB (1998) Prehospital management of acute myocardial infarction: electrocardiogram acquisition and interpretation, and thrombolysis by prehospital care providers. Can J Cardiol 14:1231–1240
Diercks DB, Peacock WF, Hiestand BC, Chen AY, Pollack CV Jr, Kirk JD, Smith SC Jr, Gibler WB, Ohman EM, Blomkalns AL, Newby LK, Hochman JS, Peterson ED, Roe MT (2006) Frequency and consequences of recording an electrocardiogram >10 minutes after arrival in an emergency room in non-ST-segment elevation acute coronary syndromes (from the crusade initiative). Am J Cardiol 97:437–442
Zahn R, Schiele R, Gitt AK, Schneider S, Seidl K, Voigtlander T, Gottwik M, Altmann E, Gieseler U, Rosahl W, Wagner S, Senges J (2001) Impact of prehospital delay on mortality in patients with acute myocardial infarction treated with primary angioplasty and intravenous thrombolysis. Am Heart J 142:105–111
Nallamothu BK, Bates ER (2003) Percutaneous coronary intervention versus fibrinolytic therapy in acute myocardial infarction: is timing (almost) everything? Am J Cardiol 92:824–826
Betriu A, Masotti M (2005) Comparison of mortality rates in acute myocardial infarction treated by percutaneous coronary intervention versus fibrinolysis. Am J Cardiol 95:100–101
Pinto DS, Kirtane AJ, Nallamothu BK, Murphy SA, Cohen DJ, Laham RJ, Cutlip DE, Bates ER, Frederick PD, Miller DP, Carrozza JP Jr, Antman EM, Cannon CP, Gibson CM (2006) Hospital delays in reperfusion for st-elevation myocardial infarction: implications when selecting a reperfusion strategy. Circulation 114:2019–2025
Schachinger V, Herdeg C, Scheller B (2010) Best way to revascularize patients with main stem and three vessel lesions: patients should undergo PCI! Clin Res Cardiol Off J German Cardiac Soc 99:531–539
Birkemeyer R, Rillig A, Koch A, Miljak T, Kunze M, Meyerfeldt U, Steffen W, Soballa M, Ranke C, Prassler R, Benzing A, Jung W (2010) Primary angioplasty for any patient with ST-elevation myocardial infarction? Guideline-adherent feasibility and impact on mortality in a rural infarction network. Clin Res Cardiol Off J German Cardiac Soc 99:833–840
Mandelzweig L, Battler A, Boyko V, Bueno H, Danchin N, Filippatos G, Gitt A, Hasdai D, Hasin Y, Marrugat J, Van de Werf F, Wallentin L, Behar S (2006) The second euro heart survey on acute coronary syndromes: characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean basin in 2004. Eur Heart J 27:2285–2293
Mehta RH, Roe MT, Chen AY, Lytle BL, Pollack CV Jr, Brindis RG, Smith SC Jr, Harrington RA, Fintel D, Fraulo ES, Califf RM, Gibler WB, Ohman EM, Peterson ED (2006) Recent trends in the care of patients with non-ST-segment elevation acute coronary syndromes: insights from the crusade initiative. Arch Intern Med 166:2027–2034
Scirica BM, Moliterno DJ, Every NR, Anderson HV, Aguirre FV, Granger CB, Lambrew CT, Rabbani LE, Arnold A, Sapp SK, Booth JE, Ferguson JJ, Cannon CP (1999) Differences between men and women in the management of unstable angina pectoris (The GUARANTEE Registry). The GUARANTEE investigators. Am J Cardiol 84:1145–1150
Stone PH, Thompson B, Anderson HV, Kronenberg MW, Gibson RS, Rogers WJ, Diver DJ, Theroux P, Warnica JW, Nasmith JB, Kells C, Kleiman N, McCabe CH, Schactman M, Knatterud GL, Braunwald E (1996) Influence of race, sex, and age on management of unstable angina and non-q-wave myocardial infarction: the TIMI III registry. JAMA 275:1104–1112
Borja J, Garcia O, Donado E, Izquierdo I (2006) Clopidogrel and metoprolol in myocardial infarction. Lancet 367:811–812
Schulz S, Mehilli J, Ndrepepa G, Dotzer F, Dommasch M, Kufner S, Birkmeier KA, Tiroch K, Byrne RA, Schomig A, Kastrati A (2011) Influence of abciximab on evolution of left ventricular function in patients with non-ST-segment elevation acute coronary syndromes undergoing PCI after clopidogrel pretreatment: lessons from the ISAR-REACT 2 trial. Clin Res Cardiol Off J German Cardiac Soc 100:691–699
De Luca G, van ‘t Hof AW, de Boer MJ, Ottervanger JP, Hoorntje JC, Gosselink AT, Dambrink JH, Zijlstra F, De Suryapranata H (2004) Time-to-treatment significantly affects the extent of ST-segment resolution and myocardial blush in patients with acute myocardial infarction treated by primary angioplasty. Eur Heart J 25:1009–1013
Nallamothu B, Fox KA, Kennelly BM, Van de Werf F, Gore JM, Steg PG, Granger CB, Dabbous OH, Kline-Rogers E, Eagle KA (2007) Relationship of treatment delays and mortality in patients undergoing fibrinolysis and primary percutaneous coronary intervention. The Global Registry of acute coronary events. Heart 93:1552–1555
Nallamothu B, Fox KA, Kennelly BM, Van de Werf F, Gore JM, Steg PG, Granger CB, Dabbous OH, Kline-Rogers E, Eagle KA, GRACE Investigators (2007) Relationship of treatment delays and mortality in patients undergoing fibrinolysis and primary percutaneous coronary intervention. The global registry of acute coronary events. Heart 93(12):1552–1555
Kurz K, Giannitsis E, Becker M, Hess G, Zdunek D, Katus HA (2011) Comparison of the new high sensitive cardiac troponin T with myoglobin, h-FABP and cTnT for early identification of myocardial necrosis in the acute coronary syndrome. Clin Res Cardiol Off J German Cardiac Soc 100:209–215
Celik S, Giannitsis E, Wollert KC, Schwobel K, Lossnitzer D, Hilbel T, Lehrke S, Zdunek D, Hess A, Januzzi JL, Katus HA (2011) Cardiac troponin T concentrations above the 99th percentile value as measured by a new high-sensitivity assay predict long-term prognosis in patients with acute coronary syndromes undergoing routine early invasive strategy. Clin Res Cardiol Off J German Cardiac Soc 100:1077–1085
Zha Y, Chen Y, Xu F, Zhang J, Li T, Zhao C, Cui L (2010) Elevated level of ADAMTS4 in plasma and peripheral monocytes from patients with acute coronary syndrome. Clin Res Cardiol Off J German Cardiac Soc 99:781–786
Acknowledgments
This work was supported by the German Cardiac Society.
Author information
Authors and Affiliations
Corresponding author
Additional information
J. Senges, T. Gori and T. Münzel contributed equally and should be considered as joint senior authors.
Appendix: Participants of the CPU registry
Appendix: Participants of the CPU registry
Institution | Town |
|---|---|
Ostalb Klinikum Aalen | Aalen |
St. Elisabeth Krankenhaus GmbH | Bad Kissingen |
Kerckhoff-Klinik | Bad Nauheim |
Herz- und Gefäßklinik GmbH | Bad Neustadt |
Vivantes Klinikum Neukölln | Berlin |
Charité Campus Virchow | Berlin |
Charité Campus Mitte | Berlin |
Vivantes Klinikum Am Urban | Berlin |
Herzzentrum Brandenburg in Bernau | Bernau |
Städtisches Klinikum Brandenburg GmbH | Brandenburg an der Havel |
MVZ am Küchwald | Chemnitz |
Klinikum Lippe- Detmold | Detmold |
Universitätsklinikum Erlangen | Erlangen |
Universitätsklinikum Essen | Essen |
Philippusstift Essen | Essen |
Elisabethkrankenhaus | Essen |
Elisabethkrankenhaus | Essen |
Klinikum Frankfurt-Höchst | Frankfurt am Main |
Markus Krankenhaus | Frankfurt am Main |
Bethanien Krankenhaus | Frankfurt am Main |
Helios Kreiskrankenhaus Gotha GmbH | Gotha |
Universitätsmedizin Göttingen | Göttingen |
Krankenhaus Neu Bethlehem | Göttingen |
Vinzenzkrankenhaus Hannover | Hannover |
Ev. KH Hamm | Hamm |
Universitätsklinikum Heidelberg | Heidelberg |
Kliniken Heilbronn GmbH | Heilbronn |
Westpfalz Klinikum | Kaiserslautern |
St. Vincentius Krankenhaus | Karlsruhe |
Städt. Klinikum | Karlsruhe |
Asklepios Kliniken Langen-Seligenstadt | Langen |
Klinikum Ludwigsburg | Ludwigsburg |
Klinikum der Johannes Gutenberg Universität | Mainz |
Kliniken Maria-Hilf | Mönchengladbach |
Klinikum Neuperlach | Munich |
Städt. Klinikum München Klinik Bogenhausen | Munich |
Klinik Augustinum München | Munich |
Lukaskrankenhaus | Neuss |
Christliches KH | Quakenbrück |
Klinikum Saarbrücken gGmbH | Saarbrücken |
Herzklinik Ulm | Ulm |
Katharinenhospital Unna | Unna |
Rights and permissions
About this article
Cite this article
Post, F., Giannitsis, E., Riemer, T. et al. Pre- and early in-hospital procedures in patients with acute coronary syndromes: first results of the “German chest pain unit registry”. Clin Res Cardiol 101, 983–991 (2012). https://doi.org/10.1007/s00392-012-0487-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-012-0487-4