Abstract
Background
Transapical aortic valve replacement (TAVR) is increasingly being applied in conventionally inoperable patients with aortic stenosis. The utility of the cardiac marker NT-pro-BNP has yet not been assessed in this setting.
Methods
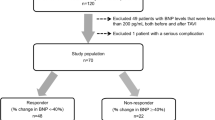
NT-pro-BNP was assessed preoperatively, postoperatively (day 1, 3, 5 and 8) and 2 months after the intervention in 31 consecutive patients (13 men, 18 women; median age 84) undergoing TAVR and the association with baseline characteristics and outcome was analysed.
Results
Baseline NT-pro-BNP was associated with baseline creatinine, left-ventricular mass index and NYHA class and predicted regression of LV-mass after 2 months. There was no correlation of NT-pro-BNP with measures of the aortic valve function before or after replacement. The increase of NT-pro-BNP 3 days after TAVR was inversely associated with a functional improvement of ≥1 NYHA class at 2 months. Baseline NT-pro-BNP was not associated with 2-month mortality and major adverse events (death/neurological deficit), whereas the postoperative increase of NT-pro-BNP after TAVR showed a slightly significant inverse and the EuroSCORE a significant correlation.
Conclusions
In multimorbid patients undergoing TAVR, NT-pro-BNP independently predicted regression of LV-mass after 2 months and early decrease of NT-pro-BNP postoperatively indicated improvement of functional capacity at 2 months. There was no association of NT-pro-BNP with 2-month mortality.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Due to the demographic development the number of old patients with aortic stenosis introduced for valve replacement is growing [8]. Hence, as these patients frequently show high comorbidity, minimally invasive procedure techniques like the transapical aortic valve replacement (TAVR) are increasingly in the focus of interest [20]. However, even with minimally invasive techniques, the risk for this patient clientele remains high [4, 23]. In addition, the nature of peri-procedural complications and risk predictors may differ from conventional surgical valve replacement, and established risk scores like the EuroSCORE may be insufficient. Therefore, the main scope must be to evaluate predictors of procedural risk and short-term benefit resulting from TAVR to clearly define the target population as evidence is lacking in this field [20].
B-type natriuretic peptides (NP) are excellent markers of cardiac function including prognostic information on cardiovascular mortality and morbidity [10, 17, 18]. As previously shown, the amino-terminal part of proBNP (NT-pro-BNP) was the strongest prognostic parameter in a multimorbid cohort of cardiac patients [18]. In patients with aortic stenosis, NPs correlate with severity of stenosis, indicate worse prognosis and can help define the optimal time point for valve replacement [1, 7, 12, 14]. Furthermore, in patients undergoing conventional aortic valve replacement, BNP was accurate and superior to the EuroSCORE in predicting peri-operative and long-term mortality [3, 11, 15]. Up to now, there are no data on NP kinetics during TAVR and the impact on prognostic and functional outcome. Results from previous studies on conventional aortic valve replacement cannot be transferred to TAVR as the patient population as well as the surgical method strongly differ.
Aim of this pilot study was to evaluate the predictive impact of NT-pro-BNP in patients undergoing TAVR. Therefore, we assessed NT-pro-BNP levels during and after the procedure and analysed associations with clinical and echocardiographic parameters and short-term outcome in 31 consecutive patients.
Subjects and methods
Patients and data acquisition
Patients undergoing TAVR (Edwards SAPIEN THV, Edwards Lifesciences) in the department of Cardiothoracic Surgery of the University of Cologne were consecutively included for this prospective observational study from March 2008 until February 2009. All patients underwent clinical examination and standard transthoracic echocardiography preoperative, pre-discharge and 2 months after TAVR. In addition, NT-pro-BNP was analysed from routinely assessed blood samples preoperatively, postoperatively on day 1, 3, 5 and 8 and 2 months after TAVR as previously described [16]. The prospectively defined outcome parameters were death, changes in echocardiographic parameters and in NYHA class.
The study was approved by the local ethics committee of the University Hospital of Cologne.
Statistics
Continuous variables appeared to be distributed non-gaussian and, thus, were summarized using medians and interquartile range (IQR) unless indicated otherwise. Comparisons between groups with respect to continuous variables were performed by non-parametric rank tests (Mann–Whitney U for independent groups and Wilcoxon for dependent groups). Qualitative variables were summarized using percentage. Group comparisons were performed by the Chi-square test. As the distribution of NT-pro-BNP was highly skewed, log transformation was carried out. Association of NT-pro-BNP with variables was analysed with linear regression analysis.
p values below 0.05 were considered statistically significant. Statistical analysis was performed using the software PASW Statistics version 17.0 for windows.
Results
Baseline parameters
Baseline characteristics of the 31 study patients are shown in Table 1. 75% of the patients were aged 80 years or older. The three patients under the age of 75 were selected because of a porcelain aorta, a severe limitation in pulmonary function and severe comorbidities (liver cirrhosis, terminal renal insufficiency, pulmonary hypertension and previous coronary bypass operation), respectively. 21 (68%) patients were in NYHA class III or IV. 24 (77.4%) patients had relevant cardiac and 25 (80.6%) patients had relevant extracardiac comorbidity. All patients had severe aortic stenosis (aortic valve area index, AVAI < 0.6 cm2/m2) and all patients were symptomatic for aortic stenosis. One patient had a re-stenosis of a biological valve implanted 2 years ago.
In linear regression analysis including all parameters of Table 1, only creatinine (standardized β 0.71, p < 0.0001), baseline left-ventricular mass index (standardized β 0.42, p = 0.02) and NYHA class (standardized β 0.40, p = 0.025) were significantly associated with NT-pro-BNP levels.
Parameters after valve replacement
TAVR with a 23-mm-diameter valve prosthesis was performed in 8 patients and TAVR with a 26-mm-diameter valve prosthesis in 21 patients. In two patients, the intervention was switched to conventional valve replacement during the procedure because of dislocation of the implanted prosthesis.
The kinetic of NT-pro-BNP and clinical parameters is shown in Table 2 and Fig. 1. Peak pressure gradient and mean pressure gradient decreased and AVA-index increased significantly after intervention and did not change significantly at the 2-month examination. NYHA class and LV-mass index significantly decreased at 2 months compared to baseline.
NT-pro-BNP showed no significant change 24 h after the intervention but showed a significant increase at 3, 5 and 8 days after intervention with a peak on day 3. After 2 months, NT-pro-BNP levels were still elevated compared with baseline, which was not statistically significant.
In linear regression analysis, baseline NT-pro-BNP levels were significantly associated with the regression of the LV-mass index at 2 months (standardized β −0.69, p = 0.002, Fig. 2). Each increase in 1 SD of baseline NT-pro-BNP was associated with a decrease of 21 g/m2 LV-mass index 2 months after valve implantation. Importantly, the association with the regression of LV-mass index remained significantly after adjustment for baseline LV-mass index (standardized β −0.56, p = 0.002).
Postinterventional NT-pro-BNP (day 3) was significantly but weakly associated with the postinterventional peak pressure gradient (standardized β 0.48, p = 0.02), but there was no association with mean pressure gradient or AVA-index. NT-pro-BNP levels at 2 months were not related to peak pressure gradient, mean pressure gradient, AVA-index, LV-myocardial mass index or NYHA class.
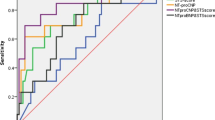
Outcome
Three (10.7%) patients died within the first 30 days after the intervention and five (16.1%) patients died within the second month after intervention (one of the eight deaths was due to malignancy). Baseline NT-pro-BNP levels were not significantly associated with 2-month mortality (p = 0.47, Fig. 3). Patients with an inframedian NT-pro-BNP increase 3 days after intervention had a lower mortality (6.7%) compared with patients with a supramedian NT-pro-BNP increase (35.7%, p = 0.05). Correspondingly, patients who died had a significantly higher increase in NT-pro-BNP on day 3 after intervention (factor 7.2, IQR 2.1–8.6) than patients who survived (factor 1.4, IQR 0.8–2.7, p = 0.03). In addition, patients with inframedian EuroSCORE/Log EuroSCORE had a significantly lower mortality (10%/6.3%) compared with patients with supramedian EuroSCORE/Log EuroSCORE (54.5%, p = 0.007/46.7%, p = 0.01). One patient developed a stroke after the intervention (with minor neurological deficit at 2 months) and one patient had a severe neurological deficit after resuscitation during the intervention. The association of major adverse events (MAE) composed of death and neurological deficit at 2 months was significant with the EuroSCORE (15% in inframedian vs. 63.6% in supramedian, p = 0.006) and the Log EuroSCORE (12.5% in inframedian vs. 53.3% in supramedian, p = 0.015) and was of borderline significance with the change of NT-pro-BNP on day 3 after intervention (13.3% in inframedian vs. 42.9% in supramedian, p = 0.08). There was no association of MAE with baseline NT-pro-BNP. Next to NT-pro-BNP and EuroSCORE, none of the variables of Table 1 was associated with mortality or MAE.
10 (45.5%) of 22 surviving patients (one of the 23 patients was excluded due to switch to conventional valve replacement) had an improvement of at least 1 NYHA class. Neither baseline NT-pro-BNP, baseline NYHA class nor the baseline degree of aortic stenosis was related to changes in NYHA class after intervention. However, patients with an inframedian increase in NT-pro-BNP 3 days after intervention showed an improvement of ≥1 NYHA class in 69.2% compared with 11.1% in patients with a supramedian NT-pro-BNP increase (p = 0.01, Fig. 4).
Discussion
This is the first study to evaluate the utility of NT-pro-BNP as a prognostic marker in patients undergoing TAVR. Baseline NT-pro-BNP was associated with NYHA class but not with parameters of cardiac or aortic valve performance. Postintervention and 2 months after valve replacement, NT-pro-BNP was not reflecting the improvement in valve function and functional capacity. However, baseline NT-pro-BNP was strongly associated with the regression of LV-mass at 2 months. Furthermore, an early decrease of NT-pro-BNP after valve replacement was associated with an improved functional capacity at 2 months. In contrast to the EuroSCORE, baseline NT-pro-BNP and the early NT-pro-BNP decrease after valve replacement were not or only weakly predictive for 2-month mortality and MAE.
Several studies describe a correlation of NP levels with morphological and functional cardiac changes reflecting the severity of aortic stenosis [5, 11, 22, 24]. However, the tightness of these correlations differs notably in previous reports. Except for NYHA class and left-ventricular mass index we did not observe any significant associations in our cohort, though previous studies included younger patients with less comorbidity making associations more obvious due to less influencing factors. Furthermore, previous studies often examined a wide range in severity of aortic stenosis including healthy controls. All our patients had symptomatic severe aortic stenosis. In this narrow range of advanced disease, correlations are more difficult to detect and probably a larger sample size is needed. The correlations of NT-pro-BNP with parameters of cardiac and valve performance were even weaker after the intervention. This is not unexpected as NP levels unspecifically increase after any type of cardiosurgical intervention [6]. Even at the 2-month examination the NT-pro-BNP values did not return to the baseline levels. Neverdal and coworkers described a normalization of NP levels 6–12 months after valve replacement and Weber found a significant correlation between changes of BNP and pressure gradient only 12 months after valve replacement [13, 25]. Thus, in concordance with these data NPs seem to be not suitable for monitoring the short-term success of reducing the valve gradient.
A very important finding of our study is that baseline NT-pro-BNP was strongly associated with the regression of LV-mass after 2 months. It is already known that NP may better reflect diastolic load and myocardial hypertrophy than systolic strain in aortic stenosis [5, 22]. Correspondingly, we also found a significant correlation of NT-pro-BNP with baseline LV-mass index. However, to our knowledge this is the first study to show that high NT-pro-BNP predicts regression of myocardial hypertrophy in aortic stenosis after valve replacement even after adjustment for baseline hypertrophy. Notably, by predicting the regression of LV-mass and in consequence the improvement in diastolic function, NT-pro-BNP could also predict the symptomatic relief which is of high clinical interest to individually select patients most benefiting from valve replacement. We did not yet find an association between baseline NT-pro-BNP and symptomatic improvement at 2 months. However, the main effect of reverse remodelling occurs 6–12 months after valve replacement [9]. Further long-term observations are needed to evaluate the predictive value of NT-pro-BNP for symptomatic improvement.
In contrast to previous reports on conventional aortic valve replacement [2, 11, 15], we found only EuroSCORE and not baseline NT-pro-BNP associated with 2-month mortality and MAE. However, as already stated, the cited studies included significantly younger patients with lower comorbidity. Additionally, in contrast to our results previous studies found also NYHA class, cardiac and functional performance to be prognostically relevant, all of which are strongly related to NP levels. Taken together, this suggests that in a “conventional replacement population” the degree of cardiac dysfunction and thereby NP levels plays a leading role for prognosis. In the “transapical population” comorbidity is higher and, hence, has a dominant influence on outcome. Although baseline NT-pro-BNP was not predictive for mortality, an early decrease in NT-pro-BNP after valve replacement was borderline significant. This may be attributed to the large inter-individual variation of NT-pro-BNP levels which is notably pronounced in old and comorbid patients [19] and underlines the importance of serial NP measurements in individuals. Accordingly, impaired renal function as one example also detected in our study is known to strongly influence NP levels due to the reduced hormone clearance [21]. Nevertheless, our data indicate that NT-pro-BNP may not be useful for a prospective risk assessment of mortality in patients introduced for TAVR. Furthermore, the discrepancy between the log EuroSCORE (median 12%) and the observed 2-months mortality of 25%—although still significantly associated—underscores the limitation of this score in a TAVR patient cohort.
A limitation on this study is the small patient cohort. Results have to be confirmed by larger registries. However, the coherence of NT-pro-BNP and EuroSCORE with mortality and reverse remodelling which is the main finding of our examination is strongly evident even in this sample size.
In conclusion, in patients undergoing TAVR serial NT-pro-BNP measurement and the EuroSCORE show complementary prognostic value with NT-pro-BNP being predictive for reverse remodelling and symptomatic benefit and the EuroSCORE being predictive for mortality. Further studies are needed to evaluate the combination of both markers to optimize the selection of patients suitable for TAVR.
References
Antonini-Canterin F, Popescu BA, Popescu AC, Beladan CC, Korcova R, Piazza R, Cappelletti P, Rubin D, Cassin M, Faggiano P, Nicolosi GL (2008) Heart failure in patients with aortic stenosis: clinical and prognostic significance of carbohydrate antigen 125 and brain natriuretic peptide measurement. Int J Cardiol 128:406–412
Bergler-Klein J, Klaar U, Heger M, Rosenhek R, Mundigler G, Gabriel H, Binder T, Pacher R, Maurer G, Baumgartner H (2004) Natriuretic peptides predict symptom-free survival and postoperative outcome in severe aortic stenosis. Circulation 109:2302–2308
Bergler-Klein J, Mundigler G, Pibarot P, Burwash IG, Dumesnil JG, Blais C, Fuchs C, Mohty D, Beanlands RS, Hachicha Z, Walter-Publig N, Rader F, Baumgartner H (2007) B-type natriuretic peptide in low-flow, low-gradient aortic stenosis: relationship to hemodynamics and clinical outcome: results from the Multicenter Truly or Pseudo-Severe Aortic Stenosis (TOPAS) study. Circulation 115:2848–2855
Bleiziffer S, Ruge H, Mazzitelli D, Schreiber C, Hutter A, Laborde JC, Bauernschmitt R, Lange R (2009) Results of percutaneous and transapical transcatheter aortic valve implantation performed by a surgical team. Eur J Cardiothorac Surg 35:615–620
Cemri M, Arslan U, Kocaman SA, Cengel A (2008) Relationship between N-terminal pro-B type natriuretic peptide and extensive echocardiographic parameters in mild to moderate aortic stenosis. J Postgrad Med 54:12–16
Georges A, Forestier F, Valli N, Plogin A, Janvier G, Bordenave L (2004) Changes in type B natriuretic peptide (BNP) concentrations during cardiac valve replacement. Eur J Cardiothorac Surg 25:941–945
Gerber IL, Legget ME, West TM, Richards AM, Stewart RA (2005) Usefulness of serial measurement of N-terminal pro-brain natriuretic peptide plasma levels in asymptomatic patients with aortic stenosis to predict symptomatic deterioration. Am J Cardiol 95:898–901
Iung B, Baron G, Butchart EG, Delahaye F, Gohlke-Barwolf C, Levang OW, Tornos P, Vanoverschelde JL, Vermeer F, Boersma E, Ravaud P, Vahanian A (2003) A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J 24:1231–1243
Krayenbuehl HP, Hess OM, Monrad ES, Schneider J, Mall G, Turina M (1989) Left ventricular myocardial structure in aortic valve disease before, intermediate, and late after aortic valve replacement. Circulation 79:744–755
Kurz K, Voelker R, Zdunek D, Wergeland R, Hess G, Ivandic B, Katus H, Giannitsis E (2007) Effect of stress-induced reversible ischemia on serum concentrations of ischemia-modified albumin, natriuretic peptides and placental growth factor. Clin Res Cardiol 96:152–159
Lim P, Monin JL, Monchi M, Garot J, Pasquet A, Hittinger L, Vanoverschelde JL, Carayon A, Gueret P (2004) Predictors of outcome in patients with severe aortic stenosis and normal left ventricular function: role of B-type natriuretic peptide. Eur Heart J 25:2048–2053
Nessmith MG, Fukuta H, Brucks S, Little WC (2005) Usefulness of an elevated B-type natriuretic peptide in predicting survival in patients with aortic stenosis treated without surgery. Am J Cardiol 96:1445–1448
Neverdal NO, Knudsen CW, Husebye T, Vengen OA, Pepper J, Lie M, Tonnessen T (2006) The effect of aortic valve replacement on plasma B-type natriuretic peptide in patients with severe aortic stenosis—1-year follow-up. Eur J Heart Fail 8:257–262
Orlowska-Baranowska E, Baranowski R, Greszata L, Stepinska J (2008) Brain natriuretic peptide as a marker of left ventricular hypertrophy in patients with aortic stenosis. J Heart Valve Dis 17:598–605
Pedrazzini GB, Masson S, Latini R, Klersy C, Rossi MG, Pasotti E, Faletra FF, Siclari F, Minervini F, Moccetti T, Auricchio A (2008) Comparison of brain natriuretic peptide plasma levels versus logistic EuroSCORE in predicting in-hospital and late postoperative mortality in patients undergoing aortic valve replacement for symptomatic aortic stenosis. Am J Cardiol 102:749–754
Pfister R, Scholz M, Wielckens K, Erdmann E, Schneider CA (2004) Use of NT-proBNP in routine testing and comparison to BNP. Eur J Heart Fail 6:289–293
Pfister R, Tan D, Thekkanal J, Hellmich M, Erdmann E, Schneider CA (2007) NT-pro-BNP measured at discharge predicts outcome in multimorbid diabetic inpatients with a broad spectrum of cardiovascular disease. Acta Diabetol 44:91–97
Pfister R, Tan D, Thekkanal J, Hellmich M, Schneider CA (2007) NT-pro-BNP is associated with long-term outcome in a heterogeneous sample of cardiac inpatients. Eur J Intern Med 18:215–220
Scharhag J, Herrmann M, Weissinger M, Herrmann W, Kindermann W (2007) N-terminal B-type natriuretic peptide concentrations are similarly increased by 30 minutes of moderate and brisk walking in patients with coronary artery disease. Clin Res Cardiol 96:218–226
Vahanian A, Alfieri O, Al-Attar N, Antunes M, Bax J, Cormier B, Cribier A, De Jaegere P, Fournial G, Kappetein AP, Kovac J, Ludgate S, Maisano F, Moat N, Mohr F, Nataf P, Pierard L, Pomar JL, Schofer J, Tornos P, Tuzcu M, van Hout HB, Von Segesser LK, Walther T (2008) Transcatheter valve implantation for patients with aortic stenosis: a position statement from the European Association of Cardio-Thoracic Surgery (EACTS) and the European Society of Cardiology (ESC), in collaboration with the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 29:1463–1470
van Kimmenade RR, Januzzi JL Jr, Bakker JA, Houben AJ, Rennenberg R, Kroon AA, Crijns HJ, van Dieijen-Visser MP, de Leeuw PW, Pinto YM (2009) Renal clearance of B-type natriuretic peptide and amino terminal pro-B-type natriuretic peptide a mechanistic study in hypertensive subjects. J Am Coll Cardiol 53:884–890
Vanderheyden M, Goethals M, Verstreken S, DeBruyne B, Muller K, VanSchuerbeeck E, Bartunek J (2004) Wall stress modulates brain natriuretic peptide production in pressure overload cardiomyopathy. J Am Coll Cardiol 44:2349–2354
Walther T, Simon P, Dewey T, Wimmer-Greinecker G, Falk V, Kasimir MT, Doss M, Borger MA, Schuler G, Glogar D, Fehske W, Wolner E, Mohr FW, Mack M (2007) Transapical minimally invasive aortic valve implantation: multicenter experience. Circulation 116:I240–I245
Weber M, Arnold R, Rau M, Brandt R, Berkovitsch A, Mitrovic V, Hamm C (2004) Relation of N-terminal pro-B-type natriuretic peptide to severity of valvular aortic stenosis. Am J Cardiol 94:740–745
Weber M, Arnold R, Rau M, Elsaesser A, Brandt R, Mitrovic V, Hamm C (2005) Relation of N-terminal pro B-type natriuretic peptide to progression of aortic valve disease. Eur Heart J 26:1023–1030
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pfister, R., Wahlers, T., Baer, F.M. et al. Utility of NT-pro-BNP in patients undergoing transapical aortic valve replacement. Clin Res Cardiol 99, 301–307 (2010). https://doi.org/10.1007/s00392-010-0118-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-010-0118-x