Abstract
Background
There is concern that transanal total mesorectal excision (TaTME) may result in poorer functional outcomes as compared to laparoscopic TME (LaTME). These concerns arise from the fact that TaTME entails both a low anastomosis and prolonged dilatation of the anal sphincter from the transanal platform.
Objectives
This paper aimed to assess the comparative functional outcomes following TaTME and LaTME, with a focus on anorectal and genitourinary outcomes.
Data sources
A meta-analysis and systematic review was performed on available literature between 2000 and 2020 from the PubMed, EMBASE, Medline, and Cochrane Library databases.
Study selection
All comparative studies assessing the functional outcomes following taTME versus LaTME in adults were included.
Main outcome measure
Functional anorectal and genitourinary outcomes were evaluated using validated scoring systems.
Results
A total of seven studies were included, consisting of one randomised controlled trial and six non-randomised studies. There were 242 (52.0%) and 233 (48.0%) patients in the TaTME and LaTME groups respectively. Anorectal functional outcomes were similar in both groups with regard to LARS scores (30.6 in the TaTME group and 28.3 in the LaTME group), Jorge-Wexner incontinence scores, and EORTC QLQ C30/29 scores. Genitourinary function was similar in both groups with IPSS scores of 5.5 to 8.0 in the TaTME group, and 3.5 to 10.1 in the LaTME group. (p = 0.835).
Conclusion
This review corroborates findings from previous studies in showing that the transanal approach is not associated with increased anal sphincter damage. Further prospective clinical trials are needed in this field of research.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The quality of life following rectal surgery is often overlooked in the provision of surgical care. Total mesorectal excision (TME) has become the standard of care in the surgical treatment of rectal cancer with excellent long-term local recurrence-free and overall survival rates [1]. With technological advances in surgery, there has been a gradual shift over time from an open approach to laparoscopic and robotic approaches, and more recently, to a transanal approach with transanal total mesorectal excision (TaTME) [2]. First described by Sylla in 2010, TaTME was developed as a novel technique to overcome difficulties encountered in distal pelvic dissection in other approaches to TME, especially when operating on patients with a high BMI, on men with a narrow android pelvis, and on low-lying tumours [3].
While there is an ongoing debate regarding the long-term oncological safety of TaTME, little has been reported about functional sequelae post-TaTME and their impact on patients’ quality of life (QoL). Patients often report disordered bowel function following rectal resection, which can have a significant impact on their QoL, and is termed as low anterior resection syndrome (LARS). In addition to anorectal dysfunction, urethral injuries following TME have also been reported, given the proximity of the dissection planes to pelvic nerves and urogenitary structures. The burden of urogenital dysfunction following TME has been increasingly acknowledged in recent years, from both laparoscopic and transanal approaches [5, 6].
This paper therefore aimed to assess the comparative functional outcomes following TaTME and LaTME, with a focus on anorectal and genitourinary outcomes, while accounting for previously reported confounders [7].
Methods
Search strategy
All relevant published studies were identified through a computer-assisted search of PubMed, EMBASE, Medline, and Cochrane Library databases between 2000 and 2020. The following medical subject heading (MeSH) terms and text words were used for the search in all possible combinations: “(rectal neoplasm OR cancer)” AND “(transanal TME OR laparoscopic TME)” AND “function” OR “functional outcomes”. The cited references in each retrieved paper were also checked for relevance. The last date for this search was 31 August 2020.
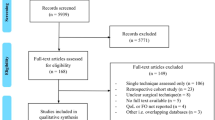
Selection of studies
The retrieved titles and abstracts of all studies were evaluated for their eligibility for inclusion according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines. All articles comparing afunctional outcomes following TaTME and LaTME in adult populations were included. All non-English studies, letters, perspectives, conference abstracts, or studies focusing on paediatric patients were excluded.
Definitions
The functional outcome assessments encountered in this meta-analysis included the low anterior resection syndrome (LARS) score, the Jorge-Wexner scale, the international prostate syndrome score (IPSS), and the European Organisation for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire (QLQ C-29/30).
Low anterior resection syndrome score
The LARS score is a symptom-based scoring system which measures bowel dysfunction following low anterior resection for rectal cancer. Major markers of incontinence include incontinence for flatus or liquid stools, frequency of bowel motions, stool clustering, and urgency. Overall scores are broken down into three groups corresponding to the severity of LARS: no LARS (0–20), minor LARS (21–29), and major LARS (30–42).
Jorge-Wexner scale
The Jorge-Wexner scale is a five-item scoring system which aims to measure the severity of faecal incontinence. Patients allocate a score between 0 (never) and 4 (always) to five symptoms (solid incontinence, liquid incontinence, flatus incontinence, pad wearing, and lifestyle alteration) to a maximum of 20.
International prostate syndrome score
The IPSS measures the quality of urinary function in male patients. It is based on seven symptoms related to urinary function—incomplete emptying, frequency, intermittency, urgency, weak stream, straining, and nocturia. Patients allocate a score of 0 (none) to 5 (almost always) to each symptom, to a maximum score of 35.
European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire (QLQ-C30 and QLQ-C29)
The QLQ-C30 questionnaire measures the QoL of cancer patients by asking a total of 30 questions with regard to five functional aspects (physical, role, emotional, cognitive, and social), eight symptoms (fatigue, nausea, pain, dyspnoea, loss of appetite, insomnia, constipation, and diarrhoea), financial strain, and global health status. The complementary QLQ-29 assesses QoL especially in colorectal cancer patients, with a total of 29 questions asked in four scales (body image, urinary frequency, blood and mucus in stool, and stool frequency).
Data extraction
Two reviewers (KTC and TWWY) independently extracted the data from the included studies using a standard data extraction form. Any discrepancies were resolved by consensus and discussion between the two reviewers and the supervising author (JCK).
Statistical analysis
All categorical data was collected as absolute numbers. Any data which reported zero events was replaced with 0.5 to allow for the computation of statistical calculations. A pooled odds ratio (OR) was calculated based on the Cochran-Mantel-Haenszel test. When reported as a median value with an associated range, this was converted to mean and SD. I2 statistics were performed to assess for inter-study heterogeneity. The Newcastle-Ottawa and Jadad scales were used to assess the quality of non-randomised studies and randomised controlled trials (RCTs) respectively. Egger’s test was performed to assess for publication bias. A p value of < 0.05 was considered significant. All data analysis was performed in R Studio Team (2015). RStudio: Integrated Development for R Studio, Inc., Boston, MA, using the metaphor package for meta-analysis.
Results
Search results and included studies
There were a total of 303 citations identified in the initial search. After removing duplicates and screening with full-text reviews, a total of seven studies were included in the study (Table 1) [8,9,10,11,12,13,14]. There were a total of 465 patients, with 242 (52.0%) patients in the TaTME group and 223 (48.0%) patients in the LaTME group.
Study design and quality
There were RCT [14] and six non-randomised studies, with three retrospective [8, 11, 13] and three prospective observational studies [9, 10, 12]. All non-randomised studies scored 6 or more on the Newcastle-Ottawa scale, and the RCT scored 3 points in the Jadad scoring system. All studies were therefore deemed to be good quality studies.
Patient characteristics and functional outcome assessments tools
The mean age for patients ranged between 57.5 and 68 years in the TaTME group and 59.9 and 68 years in the LaTME group. There were more male patients in both groups, accounting for 67.9% and 62.2% of the TaTME and LaTME groups respectively. All studies included patients who underwent neoadjuvant chemoradiotherapy (CRTx), with a slightly lower proportion of 44.2% (107 patients) in the TaTME group as compared to 50.2% (112 patients) in the LaTME group. Four studies reported on tumour staging [9, 10, 12, 14]. There were 46 (36.5%) patients in the TaTME group and 58 (53.7%) patients in the LaTME group, who had at least stage IIIa or Dukes C colorectal cancer. There were various functional outcome assessment tools utilised across the seven studies, with all studies including LARS scores. Three studies utilised the Jorge-Wexner scale [8, 10, 14], three studies used IPSS [9, 13, 14], and three studies utilised EORTC QLQ-C29 and QLC-C30 scores [9, 12, 13].
Functional outcome assessments
LARS
Five studies reported on LARS score [8,9,10, 13, 14], with a mean LARS score of 30.6 in the TaTME group and 28.3 in the LaTME group. One hundred twenty-nine (53.3%) patients in the TaTME group and 107 (47.9%) patients in the LaTME group had major or severe LARS (OR: 1.28, 95% CI: 0.88–1.87, p = 0.235) (Table 2, Fig. 1). No significant difference was identified between the two groups, with the standard mean difference (SMD) favouring the TaTME group (SMD: 0.42, 95% CI: − 0.10–0.93, p = 0.115) (Fig. 2).
Jorge-Wexner scale
Three studies reported on Jorge-Wexner scores. These scores ranged from 7 to 9 in the TaTME group and 7 to 10 in the LaTME group [8, 10, 14]. There was no significant difference identified between the two groups with the SMD favouring the TaTME group (SMD: 0.09, 95% CI: − 0.26–0.43, p = 0.623) (Fig. 3).
IPSS
Three studies reported IPSS, with scores ranging from 5.5 to 8.0 in the TaTME group and 3.5 to 10.1 in the LaTME group [9, 13, 14]. No significant differences were identified between the two groups with the SMD favouring the TaTME group (SMD: 0.07, 95% CI: − 0.56–0.69, p = 0.835) (Fig. 4). Thirty-two (28.1%) patients in the TaTME group and 25 (25.8%) patients in the LaTME group had moderate or severe IPSS symptoms (OR: 1.11, 95% CI: 0.60–2.06, p = 0.851) (Table 3, Fig. 5).
EORTC QLQ-C29
The QLQ-C29 assessment found that buttock pain, changes to taste, hair loss, faecal incontinence, and sore skin were significantly more common in the TaTME group (p = 0.011, 0.047, 0.010, 0.032, and 0.023 respectively) (Table 4). Conversely, abdominal pain and bloating symptoms were significantly more common in the LaTME group (p = 0.044 and 0.042 respectively) (Table 4). No statistically significant differences were identified with regard to any of the functional scales [9, 12, 13].
EORTC QLQ-C30
When comparing functional outcomes using the QLQ-C30 questionnaire (Table 5), diarrhoea, fatigue, and financial difficulties were significantly more likely to occur in the LaTME group (p = 0.009, 0.021, and 0.032 respectively) [9, 12, 13]. Role functioning was found to be significantly affected in favour of the LaTME group (p = 0.042) [13]. Two contradictorily significant differences were identified in two studies with regard to emotional function, with Bjoern et al. favouring LaTME (p = 0.041) and Mora et al. favouring taTME (p = 0.031) [9, 12]. There were no statistically significant differences in global health status scores across all studies.
Complications requiring surgery
Three studies reported on complication rates, with 9 (10.2%) and 14 (16.7%) patients affected in the TaTME and LaTME groups respectively. No statistically significant differences were identified between the two groups (OR: 0.58, 95% CI: 0.23–1.42, p = 0.332) (Fig. 6) [10, 13, 14].
Discussion
This systematic review and meta-analysis compared functional outcomes following LaTME and TaTME, finding that overall functional outcomes are similar with both surgical techniques.
TaTME was developed as a novel surgical technique to facilitate dissection of the lower third mesorectum, and transection of rectal cancers, particularly in the narrow android pelvis [15]. Apart from improved accessibility, TaTME allows for the construction of a low anastomosis in patients who would have otherwise required an abdominoperineal resection [16]. However, ongoing concerns persist about poor post-operative functional outcomes due to the low anastomosis, and prolonged stretch/dilatation of anal sphincter from the transanal platform intra-operatively [16, 17]. This issue is especially pertinent given the already significant prevalence of low anterior resection syndrome (LARS) following rectal surgery [4].
From our review, TaTME and LaTME have been shown to have similar anorectal functional outcomes across three different scoring modalities. The LARS score, a widely validated scoring system [4, 18] for anorectal dysfunction following rectal surgery, was utilised by all studies in this review. The mean LARS score following TaTME was 30.6, correlating to severe LARS, but no significant difference was found between the incidence of major LARS in the TaTME and LaTME groups. Both the TaTME and LaTME groups performed poorly on the Jorge-Wexner scale, the most widely applied faecal incontinence instrument to date [19]. Patients in both groups had scores ranging from 7 to 10, with no significant differences identified between the two groups. Despite the severity of faecal incontinence exhibited by patients in both groups, it was reassuring to note that only a few patients required complete disconnection of the anastomosis and construction of a colostomy due to persisting faecal incontinence [20].
Similarly, functional outcomes were again comparable between the two groups when utilising the QoL-related questionnaires EORTC QLQ-C30 and EORTC QLQ-C29 designed specifically for colorectal cancer patients. Both cohorts had higher functional burden for specific symptoms such as hair loss and abdominal pain, but contradictory findings were noted with regard to emotional function, and its incidence in the TaTME and LaTME groups. Such findings suggest that there is significant difficulty inherent in the interpretation of results of these QoL questionnaires.
The quality of functional outcome assessment lies primarily in the questionnaire used [4]. Being extensively validated, these three scoring systems provide insight into symptoms of anorectal and urogenital dysfunction following surgery. Expectedly, these scoring systems are not without their individual criticisms. The recent Delphi consensus suggested that the linear LARS score may significantly underestimate the impact of evacuatory dysfunction and may overestimate the impact on an individual patient’s quality of life in some patients [21]. The inclusion of functional QoL instruments allows for crucial assessment of the impact of these symptoms on a patient’s life [22]. The inclusion of three different scoring systems in this review is a strength that allows for careful and comprehensive evaluation of both symptoms, and their impact on the quality of life, with regard to anorectal dysfunction [4].
No significant differences between the TaTME and LaTME groups were identified with regard to urogenital function, in comparing the results from the IPSS questionnaire. While there was no considerable data on sexual function, a study by Pontallier et al. [14] found that erectile function was better in patients who underwent TaTME as compared to those who underwent LaTME, and was associated with a higher rate of sexual activity. It has therefore been hypothesised that TaTME allows for better preservation of pelvic nerves intra-operatively.
The main limitation of this review is the lack of data from RCTs. Most of the studies were heterogeneous comparative studies. Furthermore, while the use of subjective questionnaires is promising, the results should be further corroborated with objective measurements such as electromyography or sphincter manometry, which could aid in the detection of sphincter insufficiency. However, the patient’s own subjective rating should always be considered the gold standard measurement, as only they can truly perceive the implications of their anorectal or urogenital dysfunction within the context of their own life [19].
Conclusion
In this non-randomised review of current evidence, no functional differences in outcomes were identified between LaTME and TaTME. This finding supports those from previous studies showing that the transanal approach is not associated with increased anal sphincter damage. Looking ahead, further large-scale prospective clinical trials corroborating subjective functional outcomes with objective measurements are required to further support this finding.

References
Brouwer NP, Bos AC, Lemmens VE, Tanis PJ, Hugen N, Nagtegaal ID et al (2018) An overview of 25 years of incidence, treatment and outcome of colorectal cancer patients. Int J Cancer 143(11):2758–2766
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, Van Der Pas MH, De Lange-De Klerk ES et al (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372(14):1324–1332
Sylla P, Rattner DW, Delgado S, Lacy AM (2010) NOTES transanal rectal cancer resection using transanal endoscopic microsurgery and laparoscopic assistance. Surg Endosc 24(5):1205–1210
Keane C, Fearnhead NS, Bordeianou L, Christensen P, Espin Basany E, Laurberg S, Mellgren A, Messick C, Orangio GR, Verjee A, Wing K, Bissett I, the LARS International Collaborative Group, An V, Bryant A, Byrne C, Chen T, Clark D, Croft S, Dinning P, Gladman M, Heriot A, Kariappa S, Keck J, Lubowski D, Khera A, Kirkwood K, Petersen D, Sloots K, Totten B, Weston M, Andersen P, Bachmann C, Barht H, Emmertsen K, Faaborg P, Gögenur I, Ingerslev P, Isaksen D, Iversen H, Iversen L, Jacobsen K, Jansen T, Jocobsen I, Juul T, Kjær D, Krogh K, Majgaard M, Mynster A, Neuenschwander A, Nielsen C, Nielsen M, Nielsen R, Nielsen T, Olsen J, Poulsen B, Rahr H, Snedker B, Sørensen G, Stolzenburg T, Vaabengaard P, Acheson A, Andreyev J, Bach S, Battersby N, Bradbury J, Brown S, Cecil T, Chapman M, Chapman S, Chave H, Cook T, Cuffy L, Davies J, Dawson C, Dixon J, Duff S, Edwards C, Geh I, Hamilton C, Hancock L, Harji D, Hill J, Holtham S, Jenkins J, Johnston R, Kapur S, Maxwell-Armstrong C, McArthur D, Moran B, Norton C, Nugent K, Pateman L, Perston Y, Rockall T, Sagar P, Saunders M, Sebag-Montefiore D, Senapati A, Singh B, Skaife P, Smart N, Sykes H, Taylor C, Thorpe G, Tierney G, Voyce S, Walsh C, Warren O, Wheeler J, Woodward A, Winter D, Abbott S, Beban V, Bennett M, Chadwick T, Collinson R, Corbett S, Dennett E, Eglinton T, Fraser A, Glue J, Hohaia D, Menzi E, O’Connor M, Stevenson D, Wells C, Wolyncewicz S, Woodfield J, Bence K, Boutros M, Brueseke M, DeKorte J, Floruta C, Francone T, Frederick F, Grasso J, Gurland B, Higgins K, Hull T, Keller D, Laffan A, Lovett S, Marlatt J, McAdams D, McCarthy C, Milch H, Natale S, Pappou E, Paquette I, Pulskamp S, Rich M, Savitt L, Shafi M, Steele S, Stein S, Tolbert M, Varma M, Vogler S, Vuong T, Wells K, Wexner S, Wo J, Wright J, Wunderlich C, Campbell K, Lim M, Moug S, Oliphant R, Araujo-Ferreiro M, Ballester C, Belen-Bueno A, Blanco-Colino R, Carrillo-Moreno J, Castillo J, Codina-Cazador A, Enriquez-Navascuez JM, Gallego-García M, Jerez J, Jimenez LM, Labaka-Aretaga I, Martin-Fernández M, Martinez-Sanchez C, Muñoz A, Paniagua-Cayetano G, Pascual-Damieta M, de la Portilla F, Ramirez L, Sanchez-García C, Vaquer-Casas G, Vico-García E, Vigorita V, Adams R, Cornish J, Davies M, Evans M, Torkington J, Turner J (2020) International consensus definition of low anterior resection syndrome. Color Dis 22(3):331–341
Koedam T, Van Ramshorst G, Deijen C, Elfrink A, Meijerink W, Bonjer H et al (2017) Transanal total mesorectal excision (TaTME) for rectal cancer: effects on patient-reported quality of life and functional outcome. Techniques in coloproctology 21(1):25–33
Andersson J, Abis G, Gellerstedt M, Angenete E, Angerås U, Cuesta M et al (2014) Patient-reported genitourinary dysfunction after laparoscopic and open rectal cancer surgery in a randomized trial (COLOR II). Br J Surg 101(10):1272–1279
Roodbeen SX, Penna M, Mackenzie H, Kusters M, Slater A, Jones OM, Lindsey I, Guy RJ, Cunningham C, Hompes R (2019) Transanal total mesorectal excision (TaTME) versus laparoscopic TME for MRI-defined low rectal cancer: a propensity score-matched analysis of oncological outcomes. Surg Endosc 33(8):2459–2467
Foo CC, Kin Ng K, Tsang JS, Siu-hung Lo O, Wei R, Yip J, Lun Law W (2020) Low anterior resection syndrome after transanal total mesorectal excision: a comparison with the conventional top-to-bottom approach. Dis Colon Rectum 63(4):497–503
Bjoern MX, Nielsen S, Perdawood SK (2019) Quality of life after surgery for rectal Cancer: a comparison of functional outcomes after Transanal and laparoscopic approaches. J Gastrointest Surg 23(8):1623–1630
Rubinkiewicz M, Zarzycki P, Witowski J, Pisarska M, Gajewska N, Torbicz G, Nowakowski M, Major P, Budzyński A, Pędziwiatr M (2019) Functional outcomes after resections for low rectal tumors: comparison of Transanal with laparoscopic Total Mesorectal excision. BMC Surg 19(1):79
Dou R (2019) SunW, Luo S, Hou Y, Zhang C, Kang L. comparison of postoperative bowel function between patients undergoing transanal and laparoscopic total mesorectal excision. Zhonghua Wei Chang Wai Ke Za Zhi 22:246–254
Mora L, Zarate A, Serra-Aracil X, Pallisera A, Serra S, Navarro-Soto S (2018) Afectación funcional y calidad de vida tras cirugía de cáncer rectal [Functional impairment and quality of life after rectal cancer surgery]. Cir Cir 86(2):140–147
Veltcamp Helbach M, Koedam TWA, Knol JJ, Velthuis S, Bonjer HJ, Tuynman JB, Sietses C (2019) Quality of life after rectal cancer surgery: differences between laparoscopic and transanal total mesorectal excision. Surg Endosc 33(1):79–87
Pontallier A, Denost Q, Van Geluwe B, Adam JP, Celerier B, Rullier E (2016) Potential sexual function improvement by using transanal mesorectal approach for laparoscopic low rectal cancer excision. Surg Endosc 30(11):4924–4933
Rouanet P, Mourregot A, Azar CC, Carrere S, Gutowski M, Quenet F, Saint-Aubert B, Colombo PE (2013) Transanal endoscopic proctectomy: an innovative procedure for difficult resection of rectal tumors in men with narrow pelvis. Dis Colon Rectum 56(4):408–415
Kang L, Sylla P, Atallah S, Ito M, Wexner SD, Wang J-P. taTME: boom or bust? : Oxford University Press; 2020
Van der Heijden J, Koëter T, Smits L, Sietses C, Tuynman J, Maaskant-Braat A et al (2020) Functional complaints and quality of life after transanal total mesorectal excision: a meta-analysis. Br J Surg 107(5):489–498
Juul T, Ahlberg M, Biondo S, Emmertsen KJ, Espin E, Jimenez LM, Matzel KE, Palmer G, Sauermann A, Trenti L, Zhang W, Laurberg S, Christensen P (2014) International validation of the low anterior resection syndrome score. Ann Surg 259(4):728–734
Chen TY-T, Emmertsen KJ, Laurberg S (2015) What are the best questionnaires to capture anorectal function after surgery in rectal cancer? Current colorectal cancer reports 11(1):37–43
Tuech J-J, Karoui M, Lelong B, De Chaisemartin C, Bridoux V, Manceau G et al (2015) A step toward NOTES total mesorectal excision for rectal cancer: endoscopic transanal proctectomy. Ann Surg 261(2):228–233
Ribas Y, Aguilar F, Jovell-Fernández E, Cayetano L, Navarro-Luna A, Muñoz-Duyos A (2017) Clinical application of the LARS score: results from a pilot study. Int J Color Dis 32(3):409–418
O'Connor R (2004) Measuring quality of life in health. Measuring quality of life in health. p. xvi, 264-xvi,
Author information
Authors and Affiliations
Contributions
Substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data: All authors
Drafting and revising the article: All authors
Final approval of the version to be published: All authors
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Kay T. Choy and Tze Wei Wilson Yang are co-first authors and have contributed to this study equally.
Rights and permissions
About this article
Cite this article
Choy, K.T., Yang, T.W.W., Prabhakaran, S. et al. Comparing functional outcomes between transanal total mesorectal excision (TaTME) and laparoscopic total mesorectal excision (LaTME) for rectal cancer: a systematic review and meta-analysis. Int J Colorectal Dis 36, 1163–1174 (2021). https://doi.org/10.1007/s00384-021-03849-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-021-03849-2