Abstract
Purpose
Some recent studies have suggested that fluorescence angiography with indocyanine green (ICG) might be useful for preventing anastomotic leakage (AL) after laparoscopic colorectal surgery. However, its efficacy has not been proven. We evaluated whether intraoperative ICG fluorescence angiography could decrease the AL rate with laparoscopic colorectal cancer surgery.
Methods
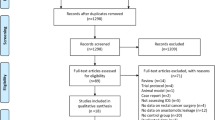
This retrospective study included patients with colorectal cancer who underwent laparoscopic surgery at our institution between March 2014 and December 2018. Patients were divided into two groups: with or without ICG fluorescence angiography. The primary outcome was the rate of AL.
Results
A total of 488 patients were included: 223 patients in the ICG group and 265 patients in the no-ICG group. In the ICG group, the transection line was changed to a more proximal location in seven patients (3.1%), including one patient with transverse colon surgery and six with rectal surgery. None of these seven patients developed AL. There were 18 ALs (3.7%) overall. The AL rate was 1.8% in the ICG group and 5.3% in the no-ICG group. For colon cancer, there were no significant differences in the AL rate between the groups (p = 0.278). In rectal cancer, the AL rate was significantly lower in the ICG group than in the no-ICG group (3.5% vs. 10.5%, p = 0.041). After propensity score matching, the AL rate was also significantly lower in the ICG group for rectal cancer (p = 0.044).
Conclusion
ICG fluorescence angiography can potentially reduce the AL rate with laparoscopic rectal cancer surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Laparoscopic surgery for colorectal cancer has become widespread in last two decades. Compared to open surgery, better short-term outcomes and reasonable long-term oncological results have been confirmed with laparoscopic surgery [1,2,3,4,5,6,7]. Although laparoscopic surgery is regarded as a feasible approach, it is more technically demanding than open surgery, and inadequate procedures could lead to complications. Colorectal cancer surgery is associated with various complications, of which anastomotic leakage (AL) is among the most detrimental. AL can increase postoperative morbidity and mortality rates, as well as the risk of local recurrence in rectal cancer resection [8,9,10]. For the purpose of improving laparoscopic colorectal cancer treatment, it is crucial to prevent the occurrence of AL.
Many factors are associated with AL occurrence. One of the most important factors is blood flow to the intestinal stump used in the anastomosis. Although sufficient blood blow is required to make a stable anastomosis, it is not always easy to evaluate blood flow precisely. Recently, indocyanine green (ICG) fluorescence angiography with near-infrared (NIR) light has been introduced in the field of laparoscopic surgery. We can utilize this method for real-time intraoperative assessment of intestinal blood flow in a way that differs from conventional methods [11,12,13]. Although ICG fluorescence angiography might be an efficient method to prevent AL after laparoscopic colorectal surgery, whether ICG fluorescence angiography can decrease the rate of AL has not been demonstrated. Given this context, we aimed to clarify whether the use of intraoperative ICG fluorescence angiography could decrease the rate of AL.
Methods
Patients
This retrospective cohort study included 488 consecutive patients with colorectal cancer who underwent laparoscopic colorectal resection with creation of an anastomosis between March 2014 and December 2018 at our institution. Patients with a previous history of colorectal resection, allergic hypersensitivity to ICG or iodine, multiorgan resection, preoperative intestinal obstruction, more than two anastomoses due to multiple sites of colorectal cancer, intra-abdominal infection, or severe comorbidities were excluded. We began to use ICG fluorescence angiography to assess intestinal perfusion at anastomotic sites in June 2017 when a laparoscopic system equipped with NIR was introduced. Since then, it has been performed in all cases except when the patient has an allergic hypersensitivity to ICG or iodine.
Analysis
Patients were classified into two groups. Patients who did not receive ICG fluorescence angiography were defined as the no-ICG group. Patients who underwent ICG fluorescence angiography were defined as the ICG group. The following patient and tumor-related characteristics were assessed: age, sex, American Society of Anesthesiologists (ASA) score, body mass index (BMI), tumor size, histopathology details, tumor location, and distance between the distal side of the tumor and the anal verge (AV distance) in patients with rectal cancer. The primary outcome was the rate of AL within 30 days of the initial operation. The effect of ICG fluorescence angiography on the rate of AL was analyzed by comparing the rate of AL in the two groups. In this study, we assessed symptomatic AL, which was defined as discharge of feces or gas from the drain or wound, discharge of pus per rectum, or rectovaginal fistula [14]. When AL was clinically suspected, one or more of the following imaging examinations were performed: (i) contrast enema radiography, (ii) contrast radiography through the drain, (iii) computerized tomography (CT), or (iv) rectoscopy. Intrapelvic abscesses with no dehiscence in the anastomosis were not defined as AL. Postoperative complications were categorized according to the Clavien-Dindo classification. Complications of Clavien-Dindo classification grade II or higher were recorded.
Surgical procedure
We performed standard laparoscopic procedures for colorectal cancer resection and robotic procedures for rectal cancer resection established in our institution. Briefly, after inserting an initial port into the umbilicus, pneumoperitoneum was established with carbon dioxide insufflation at 10 mmHg. Four to five additional ports were then inserted. The operation continued with the multi-port technique. For colon cancer resection, the colon and mesocolon were sufficiently mobilized to extract the cancer specimen. For sigmoid and rectal cancer resection, the distal rectum was transected intracorporeally using a laparoscopic linear stapler. After resecting the cancer specimen, the anastomosis was completed with the end-to-end double stapling technique for sigmoid colon cancer or rectal cancer or with the functional end-to-end anastomosis technique for other types of colon cancer. When performing an intersphincteric resection (ISR), a hand-sewn anastomosis was performed from the anal side.
ICG fluorescence angiography
Before creating the anastomosis, we performed fluorescence angiography with a 5-mg intravenous ICG injection, to assess the perfusion of the proximal colon (Figs. 1 and 2). The camera was fixed 15 cm away from the extracted specimen. If blood flow at the anastomotic site was not confirmed by 60 s after injection, we selected a more proximal site where a demarcation line was clearly observed.
Statistical analysis
Patient demographic and surgical variables were summarized as numbers (%) or medians (range). Comparisons between two groups were performed with Fisher’s exact test or the Mann–Whitney U test, as appropriate. To adjust for different distributions of covariates in the two groups that might lead to selection bias, propensity score matching was used. For each patient, a propensity score was calculated based on age, sex, tumor size, and cStage for colon cancer surgery. In addition to these variables, AV distance, neoadjuvant treatment, and whether or not a diverting stoma was created were included in the propensity score for rectal cancer surgery; all of these variables are well-known risk factors for AL [15]. One-to-one matching was performed using the nearest-neighbor matching method. The size of the caliper was set to 0.20 of the standard deviation of the logit of the estimated propensity score. All calculations were performed using EZR, a statistical software package based on R (Easy R, Version 2.13.0; Jichi Medical University, Saitama, Japan) [16]. All results were expressed as medians (range). Values of p < 0.05 were considered significant.
Results
Patients
A total of 223 patients were included in the ICG group, and 265 patients were included in the no-ICG group. Patient, tumor, and surgical characteristics are summarized in Tables 1 and 2. There was a higher proportion of male patients in the ICG group, and median age was higher in the no-ICG group, but these differences were not statistically significant (p = 0.275 and p = 0.065, respectively). Regarding tumor location, there were 116 patients with rectal cancer (52.0%) in the ICG group and 104 (39.2%) in the no-ICG group (p = 0.028). Among patients with rectal cancer, the median AV distance was 4.0 cm in the ICG group, which was similar to the median AV distance of 4.5 cm in the no-ICG group (p = 0.058). Preoperative chemotherapy was more frequently administered in the ICG group (p = 0.037). There were no significant differences in tumor size, tumor location, stage, BMI, diverting stoma status, or neoadjuvant treatment between the two groups. Regarding the type of rectal cancer surgery, the robotic approach was performed for 31.8% of patients in the ICG group, which was significantly higher than the 21.2% in the no-ICG group (p = 0.001). In addition, ISR was more frequently performed in the ICG group (28.4% in the ICG group and 14.4% in the no-ICG group, p = 0.014).
Surgical results
In the ICG group, 7 of 223 patients (3.1%) had the transection line changed to a more proximal location because perfusion in the initially planned site for anastomosis was judged to be insufficient based on ICG fluorescence angiography. One patient underwent transverse colon surgery and six patients underwent rectal surgery. None of these seven patients developed AL postoperatively.
Details about postoperative complications are shown in Table 3. A total of 18 ALs were observed. The overall AL rate was 3.7%. The AL rate in the ICG group was 1.8%, which was significantly lower than the AL rate of 5.3% in the no-ICG group (p = 0.033). Complications considered to be related to ICG fluorescence angiography were not observed. There were no significant differences between the two groups in the frequency of other kinds of complications such as ileus, surgical site infection, pneumonia, or urinary dysfunction.
Effect of ICG fluorescence angiography
We analyzed the rate of AL for colon cancer and rectal cancer surgery separately (Table 2). For colon cancer surgery, the AL rate was 0% in the ICG group and 1.8% in the no-ICG group (p = 0.278). For rectal cancer surgery, the AL rate was 3.5% in the ICG group, which was significantly lower than the rate of 10.5% in the no-ICG group (p = 0.041).
Although the AL rate for rectal cancer surgery was significantly lower in the ICG group than in the no-ICG group, bias between the groups can distort the results in the entire cohort. Propensity score matching analysis was used to minimize this bias. After propensity score matching, the two groups were nearly balanced; details on 87 matched pairs for rectal cancer are shown in Table 4. There were no significant differences in sex, age, ASA score, BMI, AV distance, tumor size, tumor location, stage, or diverting stoma status. Regarding surgical approach, robotic surgery was more frequently performed in the ICG group (p = 0.016). After propensity score matching, the AL rate in the ICG group was 3.4%, which was significantly lower than the 11.5% in the no-ICG group (p = 0.044). In addition, propensity score matching was performed for colon cancer resection to minimize bias. No cases of AL were extracted in either group because few ALs occurred with colon cancer surgery (Supplemental Table 1).
Discussion
In this study, we found that ICG fluorescence angiography is an efficient method for preventing the occurrence of AL with laparoscopic rectal cancer resection. Our results suggest that routine use of this method could potentially improve the results of laparoscopic rectal cancer surgery. By contrast, an obvious effect of ICG fluorescence angiography in colon cancer resection could not be confirmed.
Previous studies have reported that many factors could be associated with AL, including male sex, higher age, advanced stage, low anastomosis, large tumor diameter, comorbidities, malnutrition, obesity, smoking, preoperative radiotherapy, advanced tumor stage, prolonged operative time, blood loss, more than three uses of the stapler, diverting ileostomy, and inadequate blood supply to the anastomosis [15, 17,18,19]. Although it is difficult to preoperatively control most of these risk factors with medical interventions, it might be possible to identify parts of the intestines with sufficient perfusion if an appropriate method to assess blood flow is available. Conventionally, intestinal perfusion has been evaluated by surgeons based on several clinical signs, including the color of the bowel serosa, palpable pulsation, peristaltic movement, and active bleeding from marginal arteries [20]. These signs might be problematic because assessments are surgeon-dependent and tend to be inconsistent. Moreover, a definite demarcation line cannot always be recognized, as demonstrated by Karliczek et al. [21]. Thus, technical advances are needed to solve this problem.
To date, several techniques have been developed to evaluate intestinal perfusion, such as Doppler ultrasound, laser Doppler flowmetry, angiography, and oxygen spectroscopy. These techniques, however, were not widely adopted due to reasons including high initial costs, technical complexities, and inconsistent results [22]. The NIR system was introduced to perform intraoperative angiography more easily; it allows for real-time intraoperative evaluation of bowel perfusion [11, 13]. ICG fluorescence angiography could potentially be used to identify parts of the intestines with sufficient perfusion easily and objectively. It has been previously reported that ICG use in colorectal surgery might decrease the incidence of AL by assessing blood flow [23,24,25]. Most previous studies were based on the studies with small sample sizes or the lack of a historical control group. Regarding methods for evaluating ICG fluorescence, the distance from the scope to the area seemed to be inconsistent, which might influence the intensity of the fluorescence. In addition, ICG fluorescence angiography was performed before intestinal transection, resulting in the possibility that blood flow in the anastomotic portion might be impacted by additional manipulation. Based on these factors, we conducted this study to overcome limitations of prior studies.
The rate of AL after laparoscopic colon cancer resection has been reported to be 1–8% [15, 26, 27], whereas the rate after rectal cancer resection is higher, ranging from 5% to 19% [8, 15, 26, 28]. In this study, the rate of AL for colon cancer resection was 0% and 1.8% in the ICG and no-ICG groups, respectively, which are likely to be better than in previous reports. In the entire rectal cancer resection cohort, the AL rate of 10.5% in the no-ICG group was significantly higher than the 3.5% in the ICG group, suggesting that a difference of approximately seven percentage points in the rate of AL could be prevented by the use of ICG fluorescence angiography. Intriguingly, we changed the transection line to a more proximal location after ICG fluorescence angiography in 5.2% of rectal cancer surgeries; none of these patients developed AL. The prevention of AL was also confirmed by propensity score matching. Although we cannot draw definite conclusions, the rate of change in the transection line based on the findings of ICG fluorescence angiography nearly corresponds to the decrease in the AL rate after introducing ICG fluorescence angiography. It is quite possible that some patients could benefit from ICG fluorescence angiography.
The multicenter PILLAR II study is the largest published prospective case series to date (n = 139) [13]. It includes patients who underwent left colon resection for both benign and malignant disease, with anastomoses 5–15 cm from the AV. AL occurred in 1.4% of patients. The AL rate in the PILLAR II study was much lower than that of our study, but our study included patients with rectal cancer very close to the anus, and all patients had malignant disease. When taking these differences into consideration, we believe that the AL rate of 3.5% in our study is sufficiently acceptable.
There are some study limitations. First, this study was performed in a single institution, and it was a retrospective cohort study. Second, the patients were not randomly assigned. Lastly, radiological AL might have gone undetected because contrast enema was not routinely performed at our institution. Therefore, a multicenter prospective randomized study with a larger sample size that also assesses radiological leakage should be performed.
In conclusion, ICG fluorescence angiography has the potential to reduce the rate of AL in laparoscopic rectal resection. Further prospective studies are needed to confirm the usefulness of intraoperative ICG fluorescence angiography for reducing the rate of AL.
References
(2004) The clinical outcomes of surgical therapy study group A comparison of laparoscopically assisted and open colectomy for colon. N Engl J Med 350:2050–9 2
Lacy AM, Delgado S, Castells A, Prins HA, Arroyo V, Ibarzabal A, Pique JM (2008) The long-term results of a randomized clinical trial of laparoscopy-assisted versus open surgery for colon cancer. Ann Surg 248:1–7
Jayne DG, Guillou PJ, Thorpe H et al (2007) Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC trial group. J Clin Oncol 25:3061–3068
Kang S-B, Park JW, Jeong S-Y, Nam BH, Choi HS, Kim DW, Lim SB, Lee TG, Kim DY, Kim JS, Chang HJ, Lee HS, Kim SY, Jung KH, Hong YS, Kim JH, Sohn DK, Kim DH, Oh JH (2010) Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol 11:637–645
van der Pas MHGM, Haglind E, Cuesta MA et al (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14:210–218
Stevenson AR, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ, Davies L, Wilson K, Hague W, Simes J, ALaCaRT Investigators (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal Cancer: the ALaCaRT randomized clinical trial. JAMA 314:1356–1363
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M, Peters WR Jr, Maun D, Chang G, Herline A, Fichera A, Mutch M, Wexner S, Whiteford M, Marks J, Birnbaum E, Margolin D, Larson D, Marcello P, Posner M, Read T, Monson J, Wren SM, Pisters PW, Nelson H (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal Cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314:1346–1355
Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P (2011) Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg 253:890–899
Krarup PM, Nordholm-Carstensen A, Jorgensen LN, Harling H (2014) Anastomotic leak increases distant recurrence and long-term mortality after curative resection for colonic cancer: a nationwide cohort study. Ann Surg 259:930–938
Kang J, Choi GS, Oh JH et al (2015) Multicenter analysis of long-term oncologic impact of anastomotic leakage after laparoscopic total mesorectal excision: the Korean laparoscopic colorectal surgery study group. Medicine (Baltimore) 94:e1202
Watanabe J, Ota M, Suwa Y, Suzuki S, Suwa H, Momiyama M, Ishibe A, Watanabe K, Masui H, Nagahori K, Ichikawa Y, Endo I (2015) Evaluation of the intestinal blood flow near the rectosigmoid junction using the indocyanine green fluorescence method in a colorectal cancer surgery. Int J Color Dis 30:329–335
Wada T, Kawada K, Takahashi R, Yoshitomi M, Hida K, Hasegawa S, Sakai Y (2017) ICG fluorescence imaging for quantitative evaluation of colonic perfusion in laparoscopic colorectal surgery. Surg Endosc 31:4184–4193
Jafari MD, Wexner SD, Martz JE et al (2015) Perfusion assessment in laparoscopic left-sided/anterior resection (PILLAR II): a multi-institutional study. J Am Coll Surg 220(82–92):e81
Hamabe A, Ito M, Nishigori H, Nishizawa Y, Sasaki T (2018) Preventive effect of diverting stoma on anastomotic leakage after laparoscopic low anterior resection with double stapling technique reconstruction applied based on risk stratification. Asian J Endosc Surg 11:220–226
McDermott FD, Heeney A, Kelly ME, Steele RJ, Carlson GL, Winter DC (2015) Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. Br J Surg 102:462–479
Kanda Y (2013) Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant 48:452–458
Chadi SA, Fingerhut A, Berho M, DeMeester S, Fleshman JW, Hyman NH, Margolin DA, Martz JE, McLemore E, Molena D, Newman MI, Rafferty JF, Safar B, Senagore AJ, Zmora O, Wexner SD (2016) Emerging trends in the etiology, prevention, and treatment of gastrointestinal anastomotic leakage. J Gastrointest Surg 20:2035–2051
Kologlu M, Yorganci K, Renda N, Sayek I (2000) Effect of local and remote ischemia-reperfusion injury on healing of colonic anastomoses. Surgery 128:99–104
Yasui M, Takemasa I, Miyake Y et al (2017) Tumor size as an independent risk factor for postoperative complications in laparoscopic low anterior resection for advanced rectal Cancer: a multicenter Japanese study. Surg Laparosc Endosc Percutan Techn 27:98–103
Kawada K, Hasegawa S, Wada T, Takahashi R, Hisamori S, Hida K, Sakai Y (2017) Evaluation of intestinal perfusion by ICG fluorescence imaging in laparoscopic colorectal surgery with DST anastomosis. Surg Endosc 31:1061–1069
Karliczek A, Harlaar NJ, Zeebregts CJ, Wiggers T, Baas PC, van Dam G (2009) Surgeons lack predictive accuracy for anastomotic leakage in gastrointestinal surgery. Int J Color Dis 24:569–576
Son GM, Kwon MS, Kim Y et al (2018) Quantitative analysis of colon perfusion pattern using indocyanine green (ICG) angiography in laparoscopic colorectal surgery. Surg Endosc
Shen R, Zhang Y, Wang T (2018) Indocyanine green fluorescence angiography and the incidence of anastomotic leak after colorectal resection for colorectal cancer: a meta-analysis. Dis Colon Rectum 61:1228–1234
Boni L, Fingerhut A, Marzorati A et al (2017) Indocyanine green fluorescence angiography during laparoscopic low anterior resection: results of a case-matched study. Surg Endosc 31:1836–1840
Boni L, David G, Dionigi G, Rausei S, Cassinotti E, Fingerhut A (2016) Indocyanine green-enhanced fluorescence to assess bowel perfusion during laparoscopic colorectal resection. Surg Endosc 30:2736–2742
Pommergaard HC, Gessler B, Burcharth J, Angenete E, Haglind E, Rosenberg J (2014) Preoperative risk factors for anastomotic leakage after resection for colorectal cancer: a systematic review and meta-analysis. Color Dis 16:662–671
Frasson M (2015) Flor-LorenteB, Rodríguez JL et al. risk factors for anastomotic leak after colon resection for cancer: multivariate analysis and nomogram from a multicentric, prospective, National Study with 3193 patients. Ann Surg 262(2):321–330
Hashiguchi Y, Muro K, Saito Y et al (2019) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol in press
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The protocol for this study was approved by the institutional review board of Sapporo Medical University Hospital.
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM1
(PDF 147 kb)
Rights and permissions
About this article
Cite this article
Ishii, M., Hamabe, A., Okita, K. et al. Efficacy of indocyanine green fluorescence angiography in preventing anastomotic leakage after laparoscopic colorectal cancer surgery. Int J Colorectal Dis 35, 269–275 (2020). https://doi.org/10.1007/s00384-019-03482-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-019-03482-0