Abstract
Purpose
Because there are few comparative studies of open, laparoscopy-assisted (LA), and robot-assisted (RA) total mesorectal excision (TME) for rectal cancer, we aimed to compare these three procedures in terms of sphincter-saving operation (SSO) achievement, surgical complications, and early oncological outcomes.
Methods
The short-term outcomes of 2114 patients with rectal cancer consecutively enrolled between July 2010 and February 2015 at Asan Medical Center (Seoul, Korea) were retrospectively evaluated. Patients underwent either open, LA, or RA TME (n = 1095, 486, and 533, respectively) performed by experienced surgeons.
Results
RA TME was a significant determinant of SSO in multivariate analysis that included potential variables such as tumor location and T4 category (odds ratio, 2.458; 95 % confidence interval, 1.497–4.036; p < 0.001). The cumulative rates of 3-year local recurrence, overall survival, and disease-free survival did not differ among the three groups: 2.5–3.4, 91.9–94.6, and 82.2–83.1 % (p = 0.85, 0.352, and 0.944, respectively). Early general surgical complications occurred more frequently in the open group than in the LA and RA groups (19.3 versus 13.0 versus 12.2 %, p < 0.001), specifically ileus and wound infection.
Conclusions
There were no significant differences in 3-year survival outcomes and local recurrence among open, LA, and RA TME. RA TME is useful for SSO achievement, regardless of advanced stage and location of rectal cancer. The open procedure had a slightly but significantly higher incidence of postoperative complications than LA and RA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Treatment of rectal cancer patients has been focused on reducing local recurrence and increasing the use of sphincter-saving operation (SSO). Total mesorectal excision (TME), which involves complete removal of the mesorectal envelope en bloc with the rectum, is considered a prerequisite procedure because it decreases local recurrence to as low as 4–6 % [1–3]. On the other hand, multimodal treatment that includes preoperative chemoradiotherapy (CRT) clearly improves local tumor control, even in patients who undergo TME3. Tumor downstaging after concurrent preoperative CRT additionally enables SSO to include ultra-low anterior resection (ULAR) with coloanal anastomosis in a large number of patients [4]. Along with these treatment advances, the use of minimally invasive laparoscopy- and robot-assisted (LA and RA) procedures continues to grow due to their mechanical benefits, chiefly, a magnified field and increased accessibility in rectal cancer operations performed at the restrictive pelvis and delicate fascia.
Compared with open TME, LA TME showed similar disease-free survival (DFS) and overall survival (OS) outcomes in several randomized trials, as well as similar recurrence rates from 3 to 10 years of follow-up [5–7]. LA TME tends to achieve less intraoperative hemorrhage, shorter hospitalization, and faster bowel recovery than open TME, but has mixed results regarding SSO achievement, completeness of mesorectal excision, and circumferential resection margin positivity (CRM+) [8, 9]. However, these trials could be partly imprecise due to an innate bias of patient selection. For example, in the COLOR II trial [6], LA TME was not recommended in T4 or T3 rectal cancer patients with threatened circumferential margins. In addition, LA TME remains technically demanding, mainly due to awkward instrumental handling due to the levering effect. The success of robot platforms has gradually increased in the last decade, and they now achieve equivalent oncological and functional outcomes in terms of TME, SSO, and survival [10, 11]. Although these results are mostly based on studies of retrospective case series, the RA procedure seems to facilitate safe and efficient rectal cancer surgery by offering excellent pelvic visualization and instrumental dexterity. However, a longer operative time and higher cost compared with open and LA TME are the limitations.
Unfortunately, the relatively well-designed ROLARR trial (https://clinicaltrials.gov/ct2/show/NCT01736072) did not suggest any remarkable differences between RA and LA rectal cancer surgery in its early report, noting the heterogeneity of technical skills among participating surgeons (minimal requirement of ten LA and ten RA cases). Few integrative studies have compared the open, LA, and RA approaches. Accordingly, the aim of our study, conducted in a high-volume institution and involving experienced surgeons, was to compare SSO achievement, surgical complications, and early oncological outcomes among these three approaches.
Methods
Patient enrolment and preparation
A consecutive cohort of 2114 patients with rectal cancer was enrolled in the present study between July 2010 and February 2015 at Asan Medical Center, Seoul, Korea, and retrospectively reviewed to be analyzed. Eligibility criteria were curatively resected adenocarcinoma of the rectum (≤stage III), an Eastern Cooperative Oncology Group performance status of 0–3, and an age ≤75 years. Patients were excluded if they had a previous history of any cancer, hereditary colorectal cancer, or inflammatory bowel disease. Patients were provided with full information on the three procedures (open, LA, and RA approaches) and chose one (n = 1095, 486, and 533, respectively). The disease extent was assessed by clinical examination, colonoscopy, chest radiography, chest and abdominopelvic computed tomography, pelvic magnetic resonance imaging, endorectal ultrasonography, and computed tomography/positron emission tomography. Preoperative CRT was principally indicated for patients with clinical stage III or T4 cancers but was ultimately determined by the surgeon. Postoperative CRT was administered in pathologic stage III patients without preoperative CRT. Patients with preoperative or postoperative CRT received a total of 45–50.4 Gy with FL (5-FU + leucovorin) or capecitabine. All patients provided written informed consent, and the study protocol was approved by the Institutional Review Board of Asan Medical Center (registration number: 2015-0973) in accordance with the Declaration of Helsinki.
Operative procedures
All three procedures included TME with at least unilateral pelvic autonomic nerve preservation. Briefly, the open procedure was similar to the LA or RA procedures except for two points: the abdominal procedure was performed via a lateral approach and the pelvic procedure involved spiral dissection, as described previously [12]. Meanwhile, the LA and RA procedures were performed with full LA and RA colorectal mobilization via a medial approach, and the pelvic procedure involved alternative right and left dissections. The SSO was maximized by ULAR with or without intersphincteric resection (ISR), reducing abdominoperineal resection (APR) [13]. The double-stapling technique was mostly used for anorectal excision and anastomosis, except for hand-sewn anastomosis in the case of total or subtotal ISR. Finally, any cross or weak stapling points could be safely reinforced using manual sutures to prevent anastomotic leakage. The current procedures were not accompanied by a colonic J-pouch or coloplasty, and a diverting stoma was created at the surgeon’s discretion. The open procedure was performed by six qualified surgeons with 5–30 years of experience and 100–250 rectal cancer operations, whereas the LA and RA procedures were performed by six and three surgeons, respectively, with experience of at least 100 LA and 30 RA approaches, in addition to previous open experience.
Follow-up and outcome evaluations
All patients were regularly evaluated in a follow-up examination every 6 months for the first 3 years and annually thereafter until five postoperative years. Recurrence was confirmed either by imaging studies or histologic examinations. Local recurrence was defined by tumor relapse confined to the pelvis medial to the external iliac artery, whereas systemic recurrence was defined by any other relapses. The occurrence and grade [14] of general surgical complications were identified and divided into two periods of ≤1 postoperative month and thereafter. The completeness of TME was primarily examined by the respective surgeon and confirmed by the two pathologists. Distal resection margins (DRMs) and CRMs were determined as positive involvement if the distance between the deepest extent of the tumor cells and the closest margins were ≤5 and ≤1 mm on microscopic examination, respectively. Male sexual dysfunction was assessed at two postoperative years in 598 patients (61.8 %) who were ≤65 years old (open/LA/RA groups: 235/125/141 patients) by evaluating both erectile firmness and ejaculatory frequency using a visual analogue scale: none–mild dysfunction (0–1), moderate dysfunction (2–3), or severe dysfunction (4–5). Anorectal manometry was performed with the patients’ consent (open/LA/RA groups: 182/51/251 patients) at baseline and at 6–12 postoperative months (2 months after restoration of intestinal continuity).
Statistical analysis
Physical and clinicopathological variables in the three groups were compared by cross-table analysis using Pearson’s χ 2 test and Fisher’s exact test with two-sided verification or an unpaired Student’s t test and an analysis of variance (ANOVA) test, as appropriate. Potential variables were verified by multivariate analysis using binary logistic regression. Survival outcomes and recurrences were compared using the Kaplan–Meier method with the log-rank test. Statistical significance was set at p < 0.05. All analyses were carried out using the SPSS software (version 21; SPSS Inc., Chicago, IL, USA).
Results
Physical status and tumor characteristics
Physical and tumor characteristics are presented in Table 1. The mean age and comorbidity rate were somewhat lower in the RA group than those in the open and LA groups, whereas ASA status and the prior abdominal operation rate were lower in the LA group than those in the open and RA groups. Rates of preoperative or postoperative CRT and stage III tumor were significantly lower in the LA group than in the open and RA groups (p < 0.001). Lower rectal cancer was most frequent in the RA group, followed by the open group and then the LA group (p < 0.001). A similar pattern was also found for the mean tumor distance from the anal verge, which was lowest in the RA group (p < 0.001).
Surgery-related outcomes
Procedure-associated results are shown in the first half of Table 2. SSO was accomplished in more than 95 % of patients in the LA and RA groups (p < 0.001). Specifically in lower rectal cancers, APR was >2.5-fold more frequently performed in the open group than in the LA and RA groups (open versus LA versus RA: 27.5 versus 10.5 versus 10.1 %; p < 0.001). Tumor location was a significant determining factor for SSO achievement (lower versus middle and upper rectal cancers: 80.2 versus 99.8 %; p < 0.001). RA was one of the significant parameters determining SSO in multivariate analysis (odds ratio [OR], 2.458; 95 % confidence interval [CI], 1.497–4.036; p < 0.001) (Tables 3 and S1). ISR was also more frequently performed in the RA group than in the open and LA groups (p < 0.001). The mean anastomosis level was thus shorter from the anal verge in the RA group than in the open and LA groups (p < 0.001). Conversion to open surgery was significantly more frequent in the LA group than in the RA group (7.2 versus 0.2 %; p < 0.001). The causes of conversion were advanced cancer (40 %), difficult mobilization (28 %), dense adhesion (24 %), and others (one case each of marginal artery injury and anastomotic failure). The mean operative time was approximately 1 h longer in the RA group than in the open and LA groups (p < 0.001), but the mean console time in the RA group was only 66 min. Diverting ileostomy was also performed in approximately one third of patients in the open and RA groups, more frequently than the LA group, which included fewer patients with lower rectal cancer and preoperative CRT. Controllable intraoperative bleeding occurred in less than 5 % of patients without a significant difference among the three groups.
Pathological features
The pathological features are summarized in the second half of Table 2. Pathologic stage I tumor was significantly more common in the LA group than in the other two groups (p < 0.001). The mean number of retrieved lymph nodes did not differ between the open and RA groups (>20). The mean lymph node harvest was higher, and the numbers of expanding tumors and lymphovascular invasion-positive patients were greater in the LA group than in the open and RA groups. The CRM involvement rate (<2.5 %) did not differ among the three groups. The mean DRM was longer than 20 mm in the three groups, and it was a little longer in the LA group than in the open and RA groups (p = 0.019).
Postoperative outcomes
Postoperative outcomes, including surgical complications, are shown in Table 4. Operative mortality (i.e., within ≤1 month of surgery) did not occur in any patient. The pain score at postoperative day 1 was lower in the LA and RA groups than that in the open group (p < 0.001). The mean hospital stay was approximately 1 day longer in the open group than that in the LA and RA groups (p < 0.001). Early general surgical complications (i.e., within ≤1 month of surgery) occurred more frequently in the open group than in the LA and RA groups (19.3 versus 13.0 versus 12.2 %; p < 0.001), and ileus and wound infection was remarkable in the open group (p = 0.001 and 0.003, respectively). Anastomotic leakage occurred in <5 % of patients in the three groups and was slightly more frequent in the LA group than in the RA group (4.3 versus 2.1 %; p = 0.047). On the other hand, the incidence of delayed general surgical complications (i.e., within >1 month of surgery) did not differ among the three groups, except for incisional hernia, which was exclusively identified in the open group (p = 0.038). The grades of surgical complications did not differ among the three groups, regardless of the postoperative period. Postoperative ileus was significantly associated with concurrent ileal diversion (OR, 2.603; 95 % CI, 1.478–4.584; p = 0.001) and male patients in multivariate analysis (OR, 1.775; 95 % CI, 1.092–2.887; p = 0.021) (the first half of Table S2). Anastomotic complications, including leakage, abscess, fistula, and stricture, were significantly associated with male patients in multivariate analysis (OR, 1.85; 95 % CI, 1.049–3.263; p = 0.034) (the second half of Table S2). Stoma reversion was not possible during the entire follow-up period in 26 patients with temporary ileal diversion (3.9 %) or with anastomotic complications (48.1 %), without a difference among the three groups.
Bowel function was recovered earlier in the LA and RA groups than that in the open group (p < 0.001). Basic manometry factors, including maximal resting pressure (MRP), maximal squeezing pressure, urge to defecate volume, and maximal tolerance volume, were recovered to up to 81.7–99.1 % of the preoperative level between 6 and 12 months postoperatively in the 485 patients (<70 years) who consented to the manometry (Fig. S1). The MRP resumption was greatest in the LA group (p = 0.016), but the recoveries of the other three factors did not differ significantly among the three groups. Moderate-to-severe sexual dysfunction occurred more frequently in the open group than in the RA group (32.5 versus 19.1 %; p = 0.004) in male patients ≤65 years. However, male sexual dysfunction was not associated with preoperative CRT.
Recurrences and survival outcomes
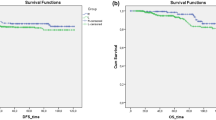
The cumulative rates of 3-year local recurrence did not differ among the three groups and were situated at 2.7, 3.4, and 2.5 % in the open, LA, and RA groups, respectively (p = 0.85) (Fig. 1a). The 3-year local recurrence rate was closely related to postoperative hemorrhage (OR, 14.02; 95 % CI, 2.592–75.84; p = 0.002), DRM+ (OR, 13.4; 95 % CI, 2.319–77.439; p = 0.004), anastomotic complications (OR, 5.514; 95 % CI, 1.416–21.475; p = 0.014), and tumor location (OR, 0.364; 95 % CI, 0.134–0.989; p = 0.047) in multivariate analysis (Table S3). The cumulative rates of the 3-year systemic recurrence did not differ among the three groups and were 16.7, 13.6, and 17.8 % in the open, LA, and RA groups, respectively (p = 0.5) (Fig. 1b). Among 161 patients with systemic recurrence, the lung (10.5 %) was the most frequent site of metastasis, followed by the liver (6.2 %), systemic lymph nodes (3.1 %), peritoneal seeding (0.8 %), bone (0.7 %), and brain (0.3 %).
Cumulative local recurrence (a), systemic recurrence (b), overall survival (c), and disease-free survival rates (d) of open, LA, and RA groups. Survival outcomes and recurrences were compared using the Kaplan–Meier method with the log-rank test. LA laparoscopy-assisted, RA robot-assisted, LR local recurrence, SR systemic recurrence, OS overall survival, DFS disease-free survival
The 3-year OS and DFS rates did not differ among the three groups (open versus LA versus RA: 3-year OS, 91.9 versus 94.4 versus 94.6 %, p = 0.352; 3-year DFS, 82.2 versus 83.1 versus 82.2 %, p = 0.944) (Fig. 1c, d). No survival differences were identified among the three groups according to the respective pathologic stage (0–I/II/III, p = 0.145–0.9) (Fig. S2).
Discussion
In our current study, the LA group included lesser patients with advanced and lower rectal cancer and, consequently, lesser patients who received preoperative and postoperative CRT, compared with open and RA groups. The LA procedure tends to be preferred for upper rectal cancers and lesser advanced tumors, irrespective of the surgeon’s competence with the LA procedure. Because the RA group was significantly correlated with SSO achievement in multivariate analysis that included tumor location and T4 category, the RA procedure was probably chosen to overcome surgical complexity in patients with locally advanced and lower rectal cancers. In addition, the rate of ISR was highest and the anastomotic level was lowest in the RA group. Conventionally, the TME procedure with SSO involves dissection of the lower rectum via an abdominal approach and is associated with technical difficulty and oncologic risk during open and LA procedures [15].
Our rate of conversion to open surgery was much lower in the RA group than in the LA group (0.2 versus 5.1 %). A recent study also showed lower conversion in RA than LA procedures (9.5 versus 16.4 %) in 2868 propensity-matched patients [16]. Laparoscopic TME, particularly in the case of bulky low rectal cancer, is technically challenging [15]. Similarly, advanced cancer and anatomical limitations were the most common causes of conversion. The RA procedure time was longer than that of the open and LA procedures, in accordance with a tendency reported in a meta-analysis [11]. The extra time for the RA procedure was mostly due to the initial installation, a shift setup for laparoscopic anastomosis, and the accompanying ileal diversion. Injury at the presacral venous plexus was the main cause of intraoperative hemorrhage. This complication was mostly controlled with compression and local application of fibrin sealants. We experienced no cases of operative mortality (within 1 month of surgery).
Early general complications, specifically ileus and wound infection, occurred more frequently in the open group than in the LA and RA groups, as previously reported [10]. In accordance with our previous study [17], we found postoperative ileus to be related to temporary ileal diversion and male sex. Additional maneuvers during ileal diversion may compromise bowel movement. Male sex was also associated with anastomotic complications, as in a recent meta-analysis [18]. This association may be partly explained by the causal relationship between postoperative ileus and male sex. The anastomotic leakage rate was <5 % in the three groups, although it tended to be more frequent in the LA group than in the RA group. The current anastomotic leakage rates seem to be lower than those of other studies (range, 3–17 %) [10, 11, 19]. One study suggested that the higher incidence of anastomotic leakage in LA surgery patients might be due to technical limitations, namely, oblique transection and repeated linear stapler use [19]. Notably, anastomotic leakage led to a permanent stoma in a half of our patients with an anastomotic complication, which was also reported as the highest risk factor in a previous study [20]. Incisional hernia was exclusively identified in patients who underwent the open procedure, which inevitably involved a longer incision than minimally invasive procedures.
The LA and RA procedures showed some benefits regarding postoperative pain, bowel recovery, and hospitalization, as shown in an intervention review [1]. We evaluated anorectal dysfunction by manometry at 6 to 12 postoperative months, and a <20 % reduction was identified in all patients of the three groups. The earlier recovery of MRP in the LA group than in the open and RA groups may be partly due to more patients with higher level of anastomosis from the anal verge. Male sexual dysfunction (≤65 years) was 1.7 times more frequent in the open group than in the RA group. This result is consistent with our previous comparative study of open and RA ISRs [13]. Another study reported an earlier recovery (3 months postoperatively) of erectile function in patients treated with RA TME than in those treated with LA TME [21]. Another analysis that included seven studies found no difference in male sexual dysfunction between open and LA procedures [22]. Interestingly, voiding difficulty did not differ among the three groups. Taken together, damage to the susceptible cavernosal fibers can be reduced at the level of the prostate and may benefit from the magnified view and fine dissection with efficient traction permitted by the RA procedure.
The mean number of retrieved lymph nodes was >20 in our three groups, which was slightly higher than that of other studies [10, 11, 19]. The three procedures in our study did not differ in terms of DRM+ and CRM+, in accordance with the results of review studies [10, 11]. DRM+ was arbitrarily defined as a ≤5-mm margin according to a systematic analysis of patients with perioperative CRT [23]. The LA group showed slightly more lymph node yields than the open and RA groups, probably due to fewer patients with preoperative CRT. Lymph node yield is significantly lower in patients with preoperative CRT than in those without it [24].
The cumulative rates of 3-year local recurrence, DFS, and OS did not differ among the three groups: 2.5–3.4, 91.9–94.6, and 82.2–83.1 %, respectively. Recent randomized controlled trials comparing local recurrence rate and survival outcomes did not show any differences between open and LA TME, although each trial was slightly different in terms of tumor stage and location [5–7]. One large-scale review also found a similar rate of local recurrence and survival outcomes between open and LA procedures [9]. Few data on survival outcomes are currently available for RA procedures, mainly due to the insufficient follow-up period since RA was introduced. We found the 3-year local recurrence closely correlated with DRM+, postoperative hemorrhage, and anastomotic complications in multivariate analysis. However, DRM may be a controversial issue due to its association with local recurrence, and approximately three times more local recurrence was reported in patients with DRM <2 cm than in those with DRM >2 cm in one study [25]. Postoperative hemorrhage tends to be related to operation complexity, physical grounding, and transfusion. One review that included 36 studies showed a moderate association between colorectal cancer recurrence and perioperative transfusions, with an OR of 1.42 (95 % CI, 1.20–1.67) [26]. We defined anastomotic complications as all pathologic processes accompanied by severe peri-anastomotic inflammation, including abscess, stricture, and fistula, in addition to anastomotic leakage. One meta-analysis including 10,953 rectal cancer patients suggested that anastomotic leakage was associated with local recurrence. Research-based evidence implicates inflammatory factors in tumor proliferation, resistance to apoptosis, metastasis, and chemoresistance [27]. Otherwise, failure or delay in postoperative CRT due to anastomotic leakage may increase local recurrence. Our study did not assess the prognostic factors of systemic recurrence and survival outcomes due to the limited observation period.
The present study is inevitably subject to several limitations. First, it is a retrospective analysis that includes heterogeneous populations of the respective groups regarding tumor stage, location, and preoperative CRT. The other main concern might be the reproducibility of outcomes due to the surgeon’s preference for each procedure. Lastly, long-term results could not be attained due to the limited follow-up period.
Despite these shortcomings, we did not find any significant differences in 3-year survival outcomes and local recurrence among open, LA, and RA TME. The RA procedure is useful in SSO achievement, regardless of rectal cancer stage and location, and possibly benefits from its magnified view and improved dexterity. The open procedure may possess a slightly higher incidence of postoperative complications than LA and RA, specifically, the ileus, wound-related complications, and incisional hernia. However, a longer follow-up is needed to validate the outcome results of the current study, as well as confirm the economic efficiency of the LA and RA approaches.
References
Vennix S, Pelzers L, Bouvy N et al (2014) Laparoscopic versus open total mesorectal excision for rectal cancer. Cochrane Database Syst Rev 4, CD005200
Martling AL, Holm T, Rutqvist LE, Moran BJ, Heald RJ, Cedemark B (2000) Effect of a surgical training programme on outcome of rectal cancer in the County of Stockholm. Stockholm Colorectal Cancer Study Group, Basingstoke Bowel Cancer Research Project. Lancet 356:93–96
Peeters KC, Marijnen CA, Nagtegaal ID et al (2007) The TME trial after a median follow-up of 6 years: increased local control but no survival benefit in irradiated patients with resectable rectal carcinoma. Ann Surg 246:693–701
Lange MM, Rutten HJ, van de Velde CJ (2009) One hundred years of curative surgery for rectal cancer: 1908–2008. Eur J Surg Oncol 35:456–463
Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ (2010) Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg 97:1638–1645
Bonjer HJ, Deijen CL, Abis GA et al (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372:1324–1332
Jeong SY, Park JW, Nam BH et al (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15:767–774
Smith JJ, Garcia-Aguilar J (2015) Advances and challenges in treatment of locally advanced rectal cancer. J Clin Oncol 33:1797–1808
Miskovic D, Foster J, Agha A et al (2015) Standardization of laparoscopic total mesorectal excision for rectal cancer: a structured international expert consensus. Ann Surg 261:716–722
Kim CW, Kim CH, Baik SH (2014) Outcomes of robotic-assisted colorectal surgery compared with laparoscopic and open surgery: a systematic review. J Gastrointest Surg 18:816–830
Araujo SE, Seid VD, Klajner S (2014) Robotic surgery for rectal cancer: current immediate clinical and oncological outcomes. World J Gastroenterol 20:14359–14370
Kim JC, Yang SS, Jang TY, Kwak JY, Yun MJ, Lim SB (2012) Open versus robot-assisted sphincter-saving operations in rectal cancer patients: techniques and comparison of outcomes between groups of 100 matched patients. Int J Med Robot 8:468–475
Kim JC, Lim SB, Yoon YS, Park IJ, Kim CW, Kim CN (2014) Completely abdominal intersphincteric resection for lower rectal cancer: feasibility and comparison of robot-assisted and open surgery. Surg Endosc 28:2734–2744
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Denost Q, Adam JP, Rullier A, Buscail E, Laurent C, Rullier E (2014) Perineal transanal approach: a new standard for laparoscopic sphincter-saving resection in low rectal cancer, a randomized trial. Ann Surg 260:993–999
Speicher PJ, Englum BR, Ganapathi AM, Nussbaum DP, Mantyh CR, Migaly J (2015) Robotic low anterior resection for rectal cancer: a national perspective on short-term oncologic outcomes. Ann Surg 262:1040–1045
Kim JC, Yu CS, Lim SB, Kim CW, Park IJ, Yoon YS (2015) Outcomes of ultra-low anterior resection combined with or without intersphincteric resection in lower rectal cancer patients. Int J Colorectal Dis 30:1311–1321
Qu H, Liu Y, Bi DS (2015) Clinical risk factors for anastomotic leakage after laparoscopic anterior resection for rectal cancer: a systematic review and meta-analysis. Surg Endosc 29:3608–3617
Park EJ, Cho MS, Baek SJ et al (2015) Long-term oncologic outcomes of robotic low anterior resection for rectal cancer: a comparative study with laparoscopic surgery. Ann Surg 261:129–137
Dinnewitzer A, Jäger T, Nawara C, Buchner S, Wolfgang H, Öfner D (2013) Cumulative incidence of permanent stoma after sphincter preserving low anterior resection of mid and low rectal cancer. Dis Colon Rectum 56:1134–1142
Kim JY, Kim NK, Lee KY, Hur H, Min BS, Kim JH (2012) A comparative study of voiding and sexual function after total mesorectal excision with autonomic nerve preservation for rectal cancer: laparoscopic versus robotic surgery. Ann Surg Oncol 19:2485–2493
Lim RS, Yang TX, Chua TC (2014) Postoperative bladder and sexual function in patients undergoing surgery for rectal cancer: a systematic review and meta-analysis of laparoscopic versus open resection of rectal cancer. Technol Coloproctol 18:993–1002
Pahlman L, Bujko K, Rutkowski A, Michalski W (2013) Altering the therapeutic paradigm towards a distal bowel margin of <1 cm in patients with low-lying rectal cancer: a systematic review and commentary. Colorectal Dis 15:e166–e174
Lykke J, Roikjaer O, Jess P, Danish Colorectal Cancer Group (2014) Tumour stage and preoperative chemoradiotherapy influence the lymph node yield in stages I-III rectal cancer: results from a prospective nationwide cohort study. Colorectal Dis 16:O144–O149
Law WL, Chu KW (2004) Anterior resection for rectal cancer with mesorectal excision: a prospective evaluation of 622 patients. Ann Surg 240:260–268
Amato A, Pescatori M (2006) Perioperative blood transfusions for the recurrence of colorectal cancer. Cochrane Database Syst Rev 1, CD005033
Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P (2011) Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg 253:890–899
Acknowledgments
This study was supported by grants (to J.C. Kim) from the Korea Research Foundation (2013R1A2A1A03070986), Ministry of Science, ICT, and Future Planning, and the Korea Health 21 R&D Project (HI06C0868 and HI13C1750), Ministry of Health, Welfare, and Family Affairs, Republic of Korea. We gratefully acknowledge the expert assistance of Dr. J. Y. Lee, Mr. Y. J. Yoon, Ms. J. R. Kim, and H. J. Jung.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All patients provided written informed consent, and the study protocol was approved by the Institutional Review Board of Asan Medical Center (registration number: 2015-0973) in accordance with the Declaration of Helsinki.
Conflict of interest
The authors declare that they have no conflict of interest.
Role of the funding source
None
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Fig. 1
Mean fold ratios of basic manometric parameters of evaluable patients (open/LA/RA groups: n = 182/52/251 patients). The data represent the ratios of the values obtained at 6–12 postoperative months to the preoperative values and were compared using an analysis or variance (ANOVA) test. MRP, maximal resting pressure; MSP, maximal squeezing pressure; UDV, urge to defecate volume; MTV, maximal tolerance volume. (GIF 37 kb)
Supplementary Fig. 2
Overall survival (a–c) and disease-free survival (d–f) of the open, LA, and RA groups according to the respective stage. Survival outcomes were compared using the Kaplan–Meier method with the log-rank test. LA, laparoscopy-assisted; RA, robot-assisted; OS, overall survival; DFS, disease-free survival. (GIF 57 kb)
Table S1
Parameters associated with SSO achievementa (DOCX 27 kb)
Table S2
Parameters associated postoperative ileus and anastomotic complicationsa (DOCX 25 kb)
Table S3
Parameters associated 3-year local recurrence (DOCX 24 kb)
Rights and permissions
About this article
Cite this article
Kim, J.C., Yu, C.S., Lim, SB. et al. Comparative analysis focusing on surgical and early oncological outcomes of open, laparoscopy-assisted, and robot-assisted approaches in rectal cancer patients. Int J Colorectal Dis 31, 1179–1187 (2016). https://doi.org/10.1007/s00384-016-2586-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-016-2586-6