Abstract
Purpose
Increased physiological stress from laparoscopic surgery and the lower physiological reserves in the elderly are causes for concern. This study aims to compare the outcomes between laparoscopic and open colorectal surgery in octogenarians.
Methods
Octogenarians who underwent elective colorectal resections from 2000 to 2011 were reviewed. Patients who underwent laparoscopic surgery were matched for comorbidities, T-staging and type of resection performed to patients with open surgery.
Results
Each group had 36 patients. Both groups were comparable for median age (85 vs 83, p = 0.43), gender (21 vs 18 males, p = 0.64) and the American Society of Anaesthesiologists (ASA) score (p = 0.486).
Both groups had comparable median maximal tumour dimensions (4.75 vs 4.25 cm, p = 0.38) and median number of lymph nodes harvested (15 vs 14, p = 0.94). The laparoscopic group had, however, a longer median operative time (167.5 vs 124.5 min, p < 0.001).
Both groups had comparable median length of hospitalisation (8 vs 7, p = 0.83), number of complications with a grade of complication (GOC) of ≥3 (5 vs 7, p = 0.75) and 30-day mortality rates (8.3 vs 5.6 %, p = 1.00). One-year survival rate for the open group was lower (75.0 vs 94.4 %, p = 0.09).
Conclusions
Despite a longer operating time, laparoscopic surgery had comparable short-term outcomes and might have a long-term survival benefit.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The elderly population in Singapore and the world is increasing, and with it, the incidence of colorectal cancer in this age group [1, 2].
Since the emergence of minimally invasive surgery, laparoscopic procedures have gained popularity in colorectal surgery. Benefits include less post-operative pain and shorter hospital stay, with comparable complication rates and oncological outcomes when compared to open surgery.
There has been concern over the safety of laparoscopic surgery for older patients, given their lower physiological reserves compared to younger patients and the increased stresses laparoscopic surgery places on the elderly [3, 4]. It is postulated that older patients have a higher risk of complications due to their frailty and higher number of comorbid conditions, which could result in poorer overall and disease-free survival [1]. There are few studies that analyse the mortality and morbidity of laparoscopic surgery specifically in the older population.
In view of the above, our study aims to compare the short-term outcomes of octogenarian patients who underwent laparoscopic to those who had open colorectal resections for colorectal cancers.
Methodology
A retrospective review of all consecutive octogenarian patients, who underwent laparoscopic colorectal resections from 2000 to 2011, was performed. Octogenarian patients were assigned to undergo open surgery by default; however, suitability for laparoscopic surgery was decided upon by the attending consultant surgeons, all of whom attained colorectal fellowship training and had performed more than 50 elective laparoscopic colonic resections during their training and prior to attaining consultant grade.
Patients were included if they were above 80 years of age and had primary colorectal cancer, elective surgical resection of their cancer with curative intent and histological evidence of malignancy, as confirmed by biopsy via colonoscopy pre-operatively.
Patients were excluded if their tumour was benign or had distant metastases as evident from pre-operative staging computed tomography (CT) of the abdomen and pelvis. All cancers were staged according to the American Joint Commission for Cancer (AJCC). Curative resection was defined as the complete excision of the primary tumour and its locoregional lymph nodes with microscopically negative margins for stages I to III disease. Conversion was defined as the termination of the laparoscopic procedure at any point of surgery, at the surgeon’s discretion.
Data collected included patient’s demographics and premorbid status, including the American Society of Anaesthesiologists score and the Charlson’s comorbidity index [5]. Pre-operative investigations, intra-operative details and post-operative details were collected. Post-operative morbidity was classified using the Clavien classification [6]. All patients who had open resections for colorectal malignancies within the time period were also reviewed. Open cases selected for the study were chosen after matching them for Charlson’s comorbidity index, T-stage of the tumour and the type of operation performed with the patients who underwent laparoscopic surgery.
Statistical tests were performed using SPSS 17 (Chicago, IL). Categorical variables were analysed using Fisher’s exact two-sided test whilst continuous variables were analysed using Mann-Whitney U test. p value <0.05 was considered to be significant. Patients were analysed on an intention-to-treat basis. Institutional Review Board approval for the study was obtained.
Results
Thirty-six patients satisfied the recruitment criteria for the laparoscopic group (laparoscopic colorectal resection octogenarian patients, LCROP) during the study period. The patients had a median age of 83 (80–94), including 18 males (50.0 %), and 94.4 % (n = 34) of them had an American Society of Anaesthesiologists (ASA) score of II–III. Twenty-six (72.2 %) patients had a Charlson’s comorbidity index of ≤3 (Table 1).
The most common procedures these patients underwent were anterior resections (n = 12, 33 %) and right hemicolectomies (n = 18, 50 %). Median operative time for the laparoscopic group of patients was 167.5 min (96–397 min). There were three (8.3 %) conversions to open procedures. Seven (19.4 %) patients had a stoma created (Table 2).
Thirty-two (88.9 %) of the tumours had a T-stage ≥3, with a median maximal tumour dimension of 4.25 cm (1.0–16.0 cm). Median number of lymph nodes harvested was 14 (11–31). One patient who had undergone an ultralow anterior resection (ULAR) had distal resection margins involved by tumour after microscopic examination by the histopathologist. The patient subsequently underwent a course of adjuvant chemoradiotherapy (Table 3).
Median length of hospitalisation was 7 days (3–23). Seven patients (19.4 %) had complications with a grade of complication (GOC) of ≥3. We encountered one anastomotic leak and one post-operative bleeding, both of which required a re-operation (Table 4).
Thirty-day mortality rate was 5.6 % (n = 2). One of the mortalities was attributed to a cardiovascular collapse post-operatively. This patient had a strong history of ischemic heart disease. The second mortality occurred on the second post-operative day and after a coroner’s examination; cause of death was likely due to severe aspiration pneumonia. There were no further mortalities at 1-year follow-up for the laparoscopic group of patients (Table 4).
Fifty-seven octogenarian patients had an open procedure during the study period, with data available for matching. After matching for T-stage and type of resection performed, the open patient group (open colorectal resection octogenarian patients, OCROP) were comparable to LCROP in terms of median age (85 vs 83, p = 0.43), gender distribution (21 vs 18 males, p = 0.64), ASA score (p = 0.49) and Charlson’s comorbidity index (p = 1.00) (Table 1).
Both groups of patients had comparable median maximal tumour dimensions (4.75 vs 4.25 cm, p = 0.38) and median lymph nodes harvested (15 vs 14, p = 0.94). None of the patients who underwent an open procedure had margin involvement (Table 3). The OCROP had a shorter median operative duration compared to LCROP (124.5 vs 167.5 min, p < 0.001) (Table 2).
Both groups, however, had comparable median length of stay (8 vs 7, p = 0.83), stoma formation rate (19.4 vs 19.4 %, p = 1.00) and number of complications with GOC ≥3 (5 vs 7, p = 0.75) (Table 4). OCROP had one (2.8 %) case of anastomotic leak, requiring a re-operation, and three patients (8.3 %) developed post-operative bleeding, of whom one required re-operation (Table 4). Both groups had comparable 30-day mortality rates (8.3 vs 5.6 %, p = 1.00).
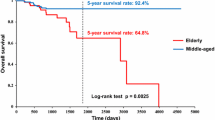
Interestingly, 1-year survival rate for OCROP was lower than for LCROP (75.0 vs 94.4 %, p = 0.090), and these additional mortalities after 30 post-operative days (n = 5, 13.9 %) were not related to the surgery or cancer. There were no further mortalities encountered in LCROP in the first year after the initial 30 post-operative days.
Discussion
With an increasing life expectancy of the world’s population, there is also an increased incidence of colorectal cancer worldwide, especially so in the older age group. The management of these older patients poses a challenge, as their lower physiological reserves and poorer premorbid status translates to an increased incidence of morbidity and mortality following surgery [7, 8]. However, several studies have shown that the long-term outcomes following colorectal resections are still favourable in octogenarians [7]. Survival of this group of patients has also been shown to be similar to the age-matched “normal” population [9]. Studies have shown that surgical intervention for malignancy is beneficial, in terms of symptom control and quality of life, in the older population group compared to conservative, non-surgical management [10].
Recent studies have not shown a significant difference in oncological outcomes between laparoscopic and open surgical colorectal cancer resections [11–15]. Large multicenter randomised trials have also supported the use of laparoscopic surgery. The Barcelona trial [15] showed that laparoscopic surgery had a better 5-year survival rate in stage III patients and comparable survival rates for the other stages, whilst the CLASICC [15] and COST [16] trials showed comparable 3-year survival and recurrence rates. A Singapore case series showed favourable oncological outcomes in an octogenarian population following resection of their tumour, with an overall survival for stage I, II, III and IV diseases of 62.3, 60.4, 51.6 and 19.3 months, respectively [1]. Furthermore, other studies suggest that the disease-specific survival rate between the elderly and younger patients is similar, and curative intent should be considered regardless of age [17, 18].
Despite the numerous advantages in surgical and oncological outcomes, the disadvantages of the laparoscopic approach include a longer operating time and being technically more challenging to master, both of which could affect its efficacy in patients who are older [13]. The necessity to establish and maintain pneumoperitoneum adds to the physiological stress experienced by the patient during laparoscopic surgery, especially in individuals with a suboptimal pulmonary function [4, 10, 19], and there have been cases of cardiopulmonary complications because of this [19]. With the increasing number of elderly patients undergoing resection of colorectal cancer, it was therefore necessary to examine the surgical outcomes specifically for the older population [9].
Laparoscopic surgery has been shown to have comparable if not superior short-term surgical outcomes when compared to open surgery. The benefits include less blood loss, less post-operative pain, faster recovery of function, less post-operative complications and shorter duration of hospitalisation [8, 9, 12, 16, 18, 20–24]. In our series, we demonstrated no significant differences in short- and long-term surgical outcomes between the laparoscopic and open surgery groups other than the operative duration. Duration of hospitalisation was shorter for LCROP compared to OCROP, although not statistically significant.
The conversion rate in our series compares favourably to those published in the literature (8.3 % vs 0–33 %) [2, 8–10, 16, 21–23]. All patients who had conversions from laparoscopic to open surgery in our series recovered from the hospital stay and were discharged well. This suggests that the employment of laparoscopic surgery still has a role in cases which are technically more challenging.
Whilst evidence for long-term survival for octogenarian patients has not been abundant in the literature, it is not unexpected that the limited evidence shows that the long-term survival for octogenarians who have undergone cancer resection surgery is poor [25, 26]. Therefore, any small improvement that laparoscopic surgery is associated with in terms of long-term survival should be regarded as noteworthy. Our series shows that patients who have undergone laparoscopic surgery are associated with a better 1-year survival rate compared to those who have undergone open surgery. This is an interesting point as many believe that laparoscopic surgery places more physiological stress onto the patient during surgery. These stressors may however be short lived, thus leading to better survival in the long term. The deaths in the open group were due to causes unrelated to surgery, which poses the question whether open surgery has a longer lasting effect on the physiological reserve in these patients, leading to their demise.
We acknowledge that there are limitations to our study. This is a retrospective review, and the allocation of cases was not randomly assigned, which may result in a selection bias. An attempt to reduce this bias was made by matching cases from both groups over the same time period and for characteristics which were considered potential confounders, such as comorbidities, tumour stage and the type of resection performed. We acknowledge that due to the retrospective nature of the study, we were unable to match for a more extensive list of factors, such as number of cycles and chemotherapy agents used during adjuvant chemotherapy.
In addition, even though the study population is small, we have found that the percentage and number of octogenarians requiring surgery for colorectal malignancies have been steadily increasing annually during the study period, which emphasises the need to better understand the outcomes of surgery in this patient group.
Conclusion
In conclusion, the short-term surgical and oncological outcomes between laparoscopic and open surgery for octogenarian patients with colorectal cancer are comparable. In addition, although it takes longer to perform, there is a suggestion that laparoscopic surgery may be associated with a better 1-year survival rate in this group of patients. Thus, laparoscopic surgery is safe and should be considered in octogenarians.
References
Tan KK, Koh FH, Tan YY, Liu JZ, Sim R (2012) Long-term outcome following surgery for colorectal cancers in octogenarians: a single institution’s experience of 204 patients. J Gastrointest Surg 16(5):1029–1036
Cheung HY, Chung CC, Fung JT, Wong JC, Yau KK, Li MK (2007) Laparoscopic resection for colorectal cancer in octogenarians: results in a decade. Dis Colon Rectum 50(11):1905–1910
Tan WS, Chew MH, Lim IA, Ng KH, Tang CL, Eu KW (2012) Evaluation of laparoscopic versus open colorectal surgery in elderly patients more than 70 years old: an evaluation of 727 patients. Int J Colorectal Dis 27(6):773–780
Gerges FJ, Kanazi GE, Jabbour-Khoury SI (2006) Anesthesia for laparoscopy: a review. J Clin Anesth 18(1):67–78
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Al-Refaie WB, Parsons HM, Habermann EB, Kwaan M, Spencer MP, Henderson WG, Rothenberger DA (2011) Operative outcomes beyond 30-day mortality: colorectal cancer surgery in oldest old. Ann Surg 253(5):947–952
Lian L, Kalady M, Geisler D, Kiran RP (2010) Laparoscopic colectomy is safe and leads to a significantly shorter hospital stay for octogenarians. Surg Endosc 24(8):2039–2043
Allardyce RA, Bagshaw PF, Frampton CM, Frizelle FA, Hewett PJ, Rieger NA, Smith JS, Solomon MJ, Stevenson AR, Australasian Laparoscopic Colon Cancer Study Group (2010) Australasian Laparoscopic Colon Cancer Study shows that elderly patients may benefit from lower postoperative complication rates following laparoscopic versus open resection. Br J Surg 97(1):86–91
Simmonds PD, Best L, George S, Baughan C, Buchanan R, Davis C, Fentiman I, Gosney M, Northover J, WIlliams C, Colorectal Cancer Collaborative Group (2000) Surgery for colorectal cancer in elderly patients: a systematic review. Lancet 356(9234):968–974
Boller AM, Nelson H (2007) Colon and rectal cancer: laparoscopic or open? Clin Cancer Res 13(22 Pt 2):6894–6896
Breukink S, Pierie J, Wiggers T (2008) Laparoscopic versus open total mesorectal excision for rectal cancer. The Cochrane Library (4)
Sambasivan CN, Deveney KE, Morris KT (2010) Oncologic outcomes after resection of rectal cancer: laparoscopic versus open approach. Am J Surg 199(5):599–603
Kuhry E, Schwenk WF, Gaupset R, Romild U, Bonjer HJ (2012) Long-term results of laparoscopic colorectal cancer resection. The Cochrane Library (5)
Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, Heath RM, Brown JM, UK MRC CLASICC Trial Group (2007) Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC trial group. J Clin Oncol 25(21):3061–3068
Clinical Outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Puig-La Calle J Jr, Quayle J, Thaler HT, Shi W, Paty PB, Quan SH, Cohen AM, Guillem JG (2000) Favorable short-term and long-term outcome after elective radical rectal cancer resection in patients 75 years of age or older. Dis Colon Rectum 43(12):1704–1709
Issa N, Grassi C, Melki Y, Powsner E, Dreznik Z (2011) Laparoscopic colectomy for carcinoma of the colon in octogenarians. J Gastrointest Surg 15(11):2011–2015
Lehmann L, Lewis MC, Goldman H, Marshall JR (1995) Cardiopulmonary complications during laparoscopy: two case reports. South Med J 88(10):1072–1075
Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, Visa J (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet 359(9325):2224–2229
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M, Lacy AM, COlon cancer Laparoscopic or Open Resection Study Group (COLOR) (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6(7):477–484
Kurian AA, Suryadevara S, Vaughn D, Zebley DM, Hofmann M, Kim S, Fassler SA (2010) Laparoscopic colectomy in octogenarians and nonagenarians: a preferable option to open surgery? J Surg Educ 67(3):161–166
Prakash K, Varma D, Rajan M, Kamlesh NP, Zacharias P, Ganesh Narayanan R, Philip M (2010) Laparoscopic colonic resection for rectosigmoid colonic tumours: a retrospective analysis and comparison with open resection. Indian J Surg 72(4):318–322
She WH, Poon JT, Fan JK, Lo OS, Law WL (2013) Outcome of laparoscopic colectomy for cancer in elderly patients. Surg Endosc 27(1):308–312
Ohigashi S (2014) Present state and problems of the surgical treatment for colorectal cancer in elderly patients. Nihon Rinsho 72(1):134–138
Steele SR, Park GE, Johnson EK, Martin MJ, Stojadinovic A, Maykel JA, Causey MW (2014) The impact of age on colorectal cancer incidence, treatment, and outcomes in an equal-access health care system. Dis Colon Rectum 57(3):303–310
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koh, F.H., Wong, J., Tan, J.K. et al. Laparoscopic colorectal surgery is safe and benefits octogenarian patients with malignant disease: a matched case-control study comparing laparoscopic and open colorectal surgery. Int J Colorectal Dis 30, 963–968 (2015). https://doi.org/10.1007/s00384-015-2252-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-015-2252-4