Abstract
Purpose
Clinical data indicate that laparoscopic surgery has a beneficial effect on intestinal wound healing and is associated with a lower incidence of anastomotic leakage. This observation is based on weak evidence, and little is known about the impact of intraoperative parameters during laparoscopic surgery, e.g., temperature and humidity.
Methods
A small-bowel anastomosis was formed in rats inside an incubator, in an environment of stable humidity and temperature. Three groups of ten Wistar rats were operated: a control group (G1) in an open surgical environment and two groups (G2 and G3) in the incubator at a humidity of 60 % and a temperature of 30 and 37 °C (G2 and G3, respectively). After 4 days, bursting pressure and hydroxyproline concentration of the anastomosis were analyzed. The tissue was histologically examined. Serum levels of C-reactive-protein (CRP) were measured.
Results
No significant changes were seen in the evaluation of anastomotic stability. Bursting pressure was very similar among the groups. Hydroxyproline concentration in G3 (36.3 μg/g) was lower by trend (p = 0.072) than in G1 (51.7 μg/g) and G2 (46.4 μg/g). The histological evaluation showed similar results regarding necrosis, inflammatory cells, edema, and epithelization for all groups. G3 (2.56) showed a distinctly worse score for submucosal bridging (p = 0.061) than G1 (1.68). A highly significant increase (p = 0.008) in CRP was detected in G3 (598.96 ng/ml) compared to G1 (439.49 ng/ml) and G2 (460 ng/ml).
Conclusion
A combination of high temperature and humidity during surgery induces an increased systemic inflammatory response and seems to be attenuating the early regeneration process in the anastomotic tissue.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Impaired intestinal wound healing and subsequent anastomotic leak remains a devastating event in gastrointestinal surgery and leads to increased patient morbidity and mortality [1]. Little is known about the mechanism of anastomotic healing in general; less evidence even exists concerning the effects of laparoscopic surgery on anastomotic healing.
Today, minimally invasive bowel resection has been established as a standard procedure in most hospitals. Retrospective analyses indicate a beneficial effect of laparoscopically performed surgery on the occurrence of anastomotic leak, other serious complications, and patient recovery [2, 3]. An attenuated systemic inflammatory response after laparoscopic surgery was even shown [4, 5]. However, this observation is based on very weak evidence and whether the improved outcome can be attributed to an improved tissue regeneration process or is biased remains unclear. Clinical analyses are compromised by several factors, like comorbidities of the selected patients, technical aspects, perioperative management and the level of experience of surgical staff [6, 7], creating an inevitable bias of any clinical investigation regarding safety and benefit of laparoscopically fashioned anastomoses [8, 9].
Anastomotic healing is a complex process that relies on countless mediator-cell interactions [10], which are prone to be affected by changes in perioperative conditions such as temperature and humidity.
When trying to understand the process of tissue regeneration, the altered intraoperative situation of laparoscopic surgery can only be reviewed systematically in an experimental animal model. Laparoscopic models have been established in large mammals, but experiments are difficult to perform for technical and ethical reasons. Rodent models for laparoscopic approaches have been described [11]. Neither setting allows for sophisticated analysis of perioperative factors like intra-abdominal pressure, temperature, humidity, and core temperature of the animal; hence, those factors remain difficult to control.
In our new approach, we used an incubator designed for neonatal care to create an environment of stable humidity and temperature, mimicking conditions found in a laparoscopic setting [12].
This model allows analysis of individual parameters such as temperature and humidity on tissue regeneration. This study is set out to determine the effects of changes in perioperative temperature and humidity on early-stage tissue regeneration after small-bowel resection.
Materials and methods
Incubator
To create conditions comparable to a laparoscopic environment, we employed an incubator originally designed for neonatal intensive care. Our device was a full-functioning Dräger 8000 IC Isolette, capable of creating and maintaining temperature between 0 and 60 °C and humidity of 15 to 95 % [12].
Experimental design
Thirty male Wistar rats (Charles River, Sulzfeld, Germany) weighing 250 to 420 g were randomised into three groups of ten rats. Small-bowel anastomosis was performed 15 cm proximal of Bauhin’s valve after resection of 1-cm ileum [13]. The animals assigned to the control group (G1) were operated under standard conditions on an operating table, while the rats in groups 2 (G2) and 3 (G3) underwent the same surgery performed by the same surgeon, but inside the incubator. G2 was operated at a temperature of 30 °C and a humidity of 60 %, G3 at an increased temperature of 37 °C, with humidity at a constant 60 %.
Operative procedure and adhesions
The rats fasted 12 h before operation with free access to water and were anaesthetised for the operation with 1.5–3 % isofluran in oxygen. All procedures were performed by the same non-blinded surgeon. After laparotomy, small-bowel resection and enteroanastomosis with single sutures (Prolene 8/0) were performed. The rats were kept in a controlled environment for 4 days with limited access to food and water. Rectal temperature and weight were taken daily. The anastomosis was assessed on the fourth post-operative day. Previous studies in rats have shown the anastomosis to be weakest at this point in time [13].
On the fourth day, a blood sample was taken from each rat for measurement of serum C-reactive-protein (CRP). Afterwards, the animals were euthanised with KCl. The abdomen was reopened, and intra-abdominal adhesions were evaluated employing the score established by van der Ham et al. in 1992 [14]. A score of zero point represents no adhesions, one point is accredited for adhesions towards the anastomosis line from the omentum, two points for adhesion of bowel and omentum towards the anastomosis line and three points for extensive adhesions towards the anastomosis line and concurrent presence of abscess. The anastomosis was resected and harvested for further investigation.
Bursting pressure, hydroxyproline concentration, and serum CRP
The evaluation of bursting pressure was performed by the surgeon not blinded toward the group the rat was assigned to. Bursting pressure as an indicator of anastomotic stability was measured by fixing one lumen of the intestinal segment to an infusion pump filled with sterile isoosmolar saline by a 14-G silicone catheter and the other end to a digital pressure transducer. Pressure was increased with an infusion rate of 60 ml/h and digitally monitored until rupturing of the anastomosis occurred. The last measured pressure was recorded as the bursting pressure [13].
Tissue hydroxyproline concentration as a direct indicator of the collagen content in the anastomotic tissue was measured in a blinded manner employing chloramine-T spectrophotometry [15]. The specimens used for hydroxyproline concentration measurement were desiccated in an oven (Heraeus Electronic UT5042EK, Germany) until a constant dry weight was achieved. The tissue was decomposed by alkaline hydrolysis, and chloramine-T was used to oxidise the free hydroxyproline in pyrrole. Adding Ehrlich’s reagent resulted in a chromophore that could be recorded at 550 nm. Data finally were calculated to express the results as micrograms of hydroxyproline per gram dry weight of tissue.
Serum CRP was measured by standard ELISA using the Rat CRP ELISA Kit by eBioscience (Santa Clara, USA) by a blinded examiner.
Histological evaluation
A strip of the anastomotic tissue was immediately spread out in a cassette for paraffin-embedding and fixed in 4 % phosphate-buffered formaldehyde. The tissue was sliced in 2-μm slices after 24 h and stained with haematoxylin-eosin. The anastomosis was reviewed by two independent blinded examiners (one pathologist) with an Olympus™ BX51 microscope. We used the criteria first described by Verhofstad et al. in 2001 for the quantification of anastomotic healing (Table 1) [16]. The number of cells was evaluated in the proximity of the anastomosis in comparison with healthy intestinal wall and is therefore semiquantitative [17].
Statistical analysis
The data are expressed as mean ± standard error of the mean (SEM). The primary outcome parameter was bursting pressure, and the secondary outcome measures were adhesions, hydroxyproline concentration, serum CRP values, and histological wound-healing score.
A Kruskal-Wallis test was used to assess overall differences in the parameters between the three groups, and a Mann-Whitney U test was added to compare groups. SPSS for Windows™ was used for statistical analysis (SPSS, Chicago, IL, USA).
Results
General
To secure comparable groups, perioperative data were taken. Surgery time (44 min) was almost identical among the groups. The temperature of the rats was monitored during the operation. The animals being operated in the incubator showed an intraoperative increase of up to 1 °C. The temperature dropped rapidly to normal levels after the end of the procedure. The core temperature post-operative showed no difference among the groups, constantly staying at an average of 36 to 37 °C. Fever did not occur in any of the animals. The rats started at an approximate weight of 300 g. All rats lost a significant amount of weight after the procedure at an average level of 10 % of their original weight. There was no significant difference among the groups.
There was one fatality due to anastomotic leak each in G1 and G2 during the 4 days of post-operative monitoring. One rat in G3 died of unknown cause, most likely urosepsis. These three rats were excluded from further analyses.
Adhesions
After reopening the abdomen, adhesions were evaluated and dissected. The degree of adhesions varied among the animals from almost none to severe. Severe adhesions with the abdominal wall were found twice in the control group and once in the group operated at 37 °C, while no severe adhesions could be detected in the group operated at 30 °C. The mean adhesion score was 2.00 in G1 and lower in G2 and G3 (1.78). The difference was not significant (p = 0.834) (Fig. 1).
Degree of adhesions. Quantification of adhesions at time of reoperation as described by van der Han et al. [14]. There are no significant changes among the groups (p = 0.834). All results are mean ± SEM
Bursting pressure and hydroxyproline concentration
The evaluation of anastomotic structure and quality was performed after removal of the anastomosis. Two parameters were measured as indication of anastomotic stability: the bursting pressure and the hydroxyproline concentration, representing the collagen level of the anastomotic tissue (Fig. 2).
Evaluation of the intestinal anstomosis. The anastomisis was harvested on the fourth day after operation for further investigation. Bursting pressure and hydroxyproline as an indicator of collagen concentration in the tissue are measured. There are no significant changes among the groups in bursting pressure (p = 0.505) or hydroxyproline concentration (p = 0.072). Bursting pressure could not be evaluated in two animals in each group due to partial change during harvesting of the anastomosis. All resulsts are mean ± SEM
Bursting pressure could not be evaluated in two animals in each group due to partial damage during harvesting of the anastomosis. All other parameters were regularly obtained.
G2 and G3 showed a lower mean bursting pressure (81.4 and 84 mmHg) than the control group (91.9 mmHg). G3 featured three anastomoses with a bursting pressure of 60 mmHg or lower—the lowest value in G1 being 79 mmHg and G2 being 68 mmHg. Overall, the difference between the groups was not significant (p = 0.505).
The mean hydroxyproline concentration increased slightly in G2 (51.7 μg/g dry weight) compared to the control (46.4 μg/g dry weight) group only to show a strong decline in group 3 (36.3 μg/g dry weight). Even though a distinct trend is visible, the difference is not significant (p = 0.072).
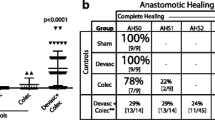
Histological evaluation
The established score for anastomotic healing (Table 1) was employed for histological review analysing the anastomotic region (Fig. 3). A low score represents a well-healed and sound anastomosis. The findings were concordant with an early regeneration process (Table 2). Most specimens showed a high degree of necrosis at the edge of the joint tissue, mostly massive necrosis was seen (52 %). The majority of the specimens showed a slight increase of polymorphonuclear cells (59 %) and lymphocytes (67 %) and marked infiltration with macrophages (78 %).
Edema was measured as the thickness of the intestinal wall. Severe edema occurred in 56 % of all specimens, while 37 % showed marked edema. In G2, a distinct increase in edema (0.32 score points) can be observed, while edema decreased again in G3, even below the level of the control group (0.34 score points). The difference was not significant (p = 0.136).
Mucosal epithelization and submucosal bridging of the anastomosis were poor in all groups; 37 % showed no epithelization at all, and none showed a normal glandular epithelium. In 77 %, no bridging or poor bridging was seen. G2 and G3 showed a slightly worse score for mucosal epithelization (p = 0.449) and a distinctly worse score for the submucosal muscular layer (p = 0.061). Particularly G3 showed very poor bridging.
The groups were very similar regarding the amount of necrotic tissue (p = 0.809). G2 and G3 showed fewer lymphocytes and more macrophages than the control group. An increase in polymorphonuclear cells compared to the control group could only be detected in G3. Overall, there was no significant difference between the groups in the number of polymorphonuclear cells (p = 0.369), lymphocytes (p = 0.491) and macrophages (p = 0.491).
Serum CRP values
Serum CRP was measured on the fourth post-operative day just before reoperation as a parameter of systemic inflammatory response. The standard range of serum CRP concentration in rats has been described from 300 to 600 ng/ml [18].
G3 operated at 37 °C and 60 % humidity showed a clearly increased CRP level of 598.96 ng/ml compared to G1 (439.49 ng/ml) and G2 (460 ng/ml). The difference was highly significant (p = 0.008). G2 operated at a temperature of only 30 °C and humidity of 60 % showed no difference to the control group (Fig. 4).
Discussion
Temperature and humidity are two relevant variables during laparoscopic surgery. Since knowledge regarding the impact of these conditions on anastomotic healing is scarce, we developed a new rodent model [12] and now present experimental data on the process of functional and structural anastomotic healing.
The laparoscopic approach changes three major factors in the patient’s physiology: The amount of trauma inflicted on the patient is reduced, causing less systematic inflammation. During surgery, there is a constant overload pressure inside the abdomen, built up by 100 % CO2; furthermore, there is a constant environment of intraperitoneal temperature and humidity for the time of surgery, depending on the humidity and temperature of the gas inflated [5, 19].
In our experimental setting, we selectively altered one of these variables. All rats experienced the same trauma and were not exposed to increased intra-abdominal pressure or CO2, but the rats operated in the incubator were subjected to a controlled environment of constant humidity and temperature. Our model is therefore limited to mimic the conditions found during laparoscopic surgery because we still use open surgery without the use of a capnoperitoneum.
The literature discusses a reduction of peritoneal desiccation by employing warmed and humified gas for laparoscopy [20]. Meta-analyses were able to show reduced post-operative pain after laparoscopy with warm, humified gas but fail to show further beneficial effects [21, 22].
Our results reflect the specific effects of humidity and temperature on the process of tissue regeneration, distinguishing our model from other rodent models for laparoscopic surgery [11].
Clinical analyses show a lesser degree of adhesions after laparoscopic compared to open surgery [23]. Animal studies show a modulation of the degree of adhesions by different compounds of the gas used for the pneumoperitoneum and hypothermia [20, 24]. In our experiment, the rats operated in the incubator tended to develop fewer adhesions. Even though the results are not significant, they suggest an influence of humidity and temperature. Other groups have shown that the effects on peritoneum and wound healing of pneumoperitoneum compare to those of a laparotomy [25, 26]. Constant temperature and humidity are a plausible approach to explaining the clinically observed beneficial effects of laparoscopic surgery on the formation of adhesions.
None of the parameters determined are capable of showing improved tissue regeneration in those rats operated in the incubator. Without being significant, our results strongly argue to the contrary: Mean bursting pressure tends to be lower for the groups operated at higher temperature and humidity. Earlier experimental studies have shown that a healthy small bowel has to stand an intermittent pressure of 50 mmHg [27]. G3, subjected to a constant intra-abdominal temperature of 37 °C, featured three rats with a very low bursting pressure just above the threshold to rupturing.
The evaluation of hydroxyproline content and histopathological evaluation of submucosal bridging indicate the same: Higher temperature and humidity show a very strong tendency to attenuate the regeneration of submucosal tissue. Our results indicate a disturbance of collagen synthesis and integration or increased collagen depletion rendered by an environment of increased intraoperative humidity and temperature.
We observed an increased infiltration of the anastomotic tissue with polymorphonuclear cells and macrophages in G2 and G3. Experimental studies have shown that pharmacological stimulation with granulocyte-macrophage colony-stimulating factor has beneficial effects on bursting pressure and hydroxyproline concentration in rats with impaired wound healing [28–30]. The presence of macrophages seems to be crucial for a sufficient tissue regeneration process. Macrophages secrete a number of degrading enzymes, in particular collagenases like matrix metalloproteinase (MMP) which disintegrate connective tissue and have a crucial role in the early stages of wound healing [10].
Our results indicate, though, that possibly a boosted macrophage activity might also have a disruptive effect on anastomotic healing. We were able to show a clear correlation between high count of inflammatory cells in the anastomotic tissue and attenuated bursting pressure in a different setting. Perioperative crystalloid fluid overload in rats undergoing small-bowel resection leads to reduced bursting pressure [31], an increased infiltration of inflammatory cells and an overexpression of MMPs [17].
Studies indicate that collagen cleavage by MMP is temperature-dependent [32, 33] and were able to show a hypothermia-induced decreased MMP-activity in stroke patients [34]. Temperature-induced accelerated collagen cleavage by collagenases like MMP would be a feasible approach to explain diminished bursting pressure and submucosal bridging found in the early stage of wound healing in rats operated at higher temperature and humidity. The observed effect might not be relevant towards stability of the anastomosis after tissue regeneration is completed (day 7 and after).
The analysis of serum CRP at the fourth post-operative day is a marker for the systemic inflammatory response of the animal. The serum CRP concentration of healthy laboratory rats was described previously as 300–600 ng/ml, rising to around 900 ng/ml during an acute-phase response [18]. Therefore, rats have a high baseline CRP compared to other species, while it only shows a weak increase due to a systemic inflammatory response. Consequently, the marked increase in serum CRP observed in G3 is not only statistically significant but has to be considered highly relevant and underlines a strong influence of perioperative humidity and temperature on the post-operative systemic response.
Previous clinical analyses have shown an attenuating effect of intraoperative hypothermia on the release of systemic inflammatory parameters in patients undergoing abdominal surgery [35]. An increased serum CRP level in G3 compared to control is thus plausible.
Analysis of the anastomotic tissue shows a tendency towards impaired anastomotic healing in G3. Clinical observations have proven a weakened anastomotic stability and greater risk of anastomotic leak in patients operated during sepsis or severe SIRS [36]. The pathogenesis appears to be impaired colonic reparative collagen synthesis [37] and modulation of the immune response [38].
The observed increased serum CRP levels are a feasible approach to explain the tendency to impaired wound healing and disturbance in collagen synthesis in G3.
Our experimental data do not show significantly altered healing of intestinal anastomoses due to different perioperative temperature and humidity. High operative temperature leads to an increased systemic inflammatory response and seems to affect structural anastomotic healing. Our conclusions are based on experiments with a limited number of animals and should be regarded cautiously when looking for differences between the study groups. Further experiments are necessary to evaluate the clinical relevance of perioperative temperature and humidity.
References
Thornton M, Joshi H, Vimalachandran C et al (2011) Management and outcome of colorectal anastomotic leaks. Int J Colorectal Dis 26(3):313–320. doi:10.1007/s00384-010-1094-3
Luján JJ, Németh ZH, Barratt-Stopper PA et al (2011) Factors influencing the outcome of intestinal anastomosis. Am Surg 77(9):1169–1175
Levack M, Berger D, Sylla P et al (2011) Laparoscopy decreases anastomotic leak rate in sigmoid colectomy for diverticulitis. Arch Surg 146(2):207–210. doi:10.1001/archsurg.2010.325
Wang G, Jiang Z, Zhao K et al (2012) Immunologic response after laparoscopic colon cancer operation within an enhanced recovery program. J Gastrointest Surg 16(7):1379–1388. doi:10.1007/s11605-012-1880-z
Veenhof AAFA, Vlug MS, van der Pas MHGM et al (2012) Surgical stress response and postoperative immune function after laparoscopy or open surgery with fast track or standard perioperative care: a randomized trial. Ann Surg 255(2):216–221. doi:10.1097/SLA.0b013e31824336e2
Dekker JWT, Liefers GJ, van Mol Otterloo de JCA et al (2011) Predicting the risk of anastomotic leakage in left-sided colorectal surgery using a colon leakage score. J Surg Res 166(1):e27–e34. doi:10.1016/j.jss.2010.11.004
Richards CH, Campbell V, Ho C et al (2011) Smoking is a major risk factor for anastomotic leak in patients undergoing low anterior resection. Colorectal Dis 14:628–633. doi:10.1111/j.1463-1318.2011.02718.x
Boccola MA, Buettner PG, Rozen WM et al (2011) Risk factors and outcomes for anastomotic leakage in colorectal surgery: a single-institution analysis of 1576 patients. World J Surg 35(1):186–195. doi:10.1007/s00268-010-0831-7
Boccola MA, Lin J, Rozen WM et al (2010) Reducing anastomotic leakage in oncologic colorectal surgery: an evidence-based review. Anticancer Res 30(2):601–607
Marjanovic G, Hopt UT (2011) Physiologie der Anastomosenheilung (Physiology of anastomotic healing). Chirurg 82(1):41–47. doi:10.1007/s00104-010-1898-2
Tytgat SHAJ, Rijkers GT, van der Zee DC (2011) The influence of the CO(2) pneumoperitoneum on a rat model of intestinal anastomosis healing. Surg Endosc 26:1642–1647. doi:10.1007/s00464-011-2086-2
Glatz T, Seifert G, Holzner PA et al (2012) A novel rodent model modifying perioperative temperature and humidity during bowel surgery and mimicking laparoscopic conditions. Surg Sci 3(7):353–357
Marjanovic G, Holzner P, Kulemann B et al (2010) Pitfalls and technical aspects during the research of intestinal anastomotic healing in rats. Eur Surg Res 45(3–4):314–320. doi:10.1159/000320768
van der Ham AC, Kort WJ, Weijma IM et al (1992) Healing of ischemic colonic anastomosis: fibrin sealant does not improve wound healing. Dis Colon Rectum 35(9):884–891
Reddy GK, Enwemeka CS (1996) A simplified method for the analysis of hydroxyproline in biological tissues. Clin Biochem 29(3):225–229
Verhofstad MH, Lange WP, van der Laak JA et al (2001) Microscopic analysis of anastomotic healing in the intestine of normal and diabetic rats. Dis Colon Rectum 44(3):423–431
Kulemann B, Timme S, Seifert G et al (2013) Intraoperative crystalloid overload leads to substantial inflammatory infiltration of intestinal anastomoses-a histomorphological analysis. Surgery 154:596–603. doi:10.1016/j.surg.2013.04.010
de Beer FC, Baltz ML, Munn EA et al (1982) Isolation and characterization of C-reactive protein and serum amyloid P component in the rat. Immunology 45(1):55–70
Rosch R, Stumpf M, Junge K et al (2004) Impact of pressure and gas type on anastomotic wound healing in rats. Langenbecks Arch Surg 389(4):261–266. doi:10.1007/s00423-004-0491-x
Binda MM, Molinas CR, Hansen P et al (2006) Effect of desiccation and temperature during laparoscopy on adhesion formation in mice. Fertil Steril 86(1):166–175. doi:10.1016/j.fertnstert.2005.11.079
Birch DW, Manouchehri N, Shi X et al (2011) Heated CO(2) with or without humidification for minimally invasive abdominal surgery. Cochrane Database Syst Rev 1:CD007821. doi:10.1002/14651858.CD007821.pub2
Sammour T, Kahokehr A, Hill AG (2008) Meta-analysis of the effect of warm humidified insufflation on pain after laparoscopy. Br J Surg 95(8):950–956. doi:10.1002/bjs.6304
Gutt CN, Oniu T, Schemmer P et al (2004) Fewer adhesions induced by laparoscopic surgery? Surg Endosc 18(6):898–906. doi:10.1007/s00464-003-9233-3
Elkelani OA, Binda MM, Molinas CR et al (2004) Effect of adding more than 3 % oxygen to carbon dioxide pneumoperitoneum on adhesion formation in a laparoscopic mouse model. Fertil Steril 82(6):1616–1622. doi:10.1016/j.fertnstert.2004.07.933
Brokelman WJA, Lensvelt M, Borel Rinkes IHM et al (2011) Peritoneal changes due to laparoscopic surgery. Surg Endosc 25(1):1–9. doi:10.1007/s00464-010-1139-2
Agalar F, Hamaloglu E, Daphan C et al (2000) Effects of CO2 insufflation and laparotomy on wound healing in mice. Aust N Z J Surg 70(10):739–742
Müller G, Kieninger G, Breucha G et al (1978) Vergleichende Untersuchungen ein- und zweireihiger Anastomosen am Schweinedünndarm (Comparative study on single layer and two layer anastomoses of small intestine (author’s transl)). Langenbecks Arch Chir 346(1):37–45
Liu Y, Yang Y, Liu H et al (2012) Preliminary study on mechanisms of granulocyte macrophage-colony stimulating factor in enhancing impaired colonic anastomotic healing in rats treated with intraperitoneal oxaliplatin. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 26(10):1232–1236
Dinc S, Ozbirecikli B, Gulcelik MA et al (2004) The effects of locally injected granulocyte macrophage-colony stimulating factor on the healing of intraoperatively irradiated intestinal anastomoses in rats. J Exp Clin Cancer Res 23(1):77–82
Gulcelik MA, Dinc S, Bir F et al (2005) Locally applied molgramostim improves wound healing at colonic anastomoses in rats after ligation of the common bile duct. Can J Surg 48(3):213–218
Marjanovic G, Villain C, Juettner E et al (2009) Impact of different crystalloid volume regimes on intestinal anastomotic stability. Ann Surg 249(2):181–185. doi:10.1097/SLA.0b013e31818b73dc
Löffler G, Petrides P (eds) (2003) Biochemie und Pathobiochemie, 7th edn. Springer, Heidelberg
Lu KG, Stultz CM (2013) Insight into the degradation of type-I collagen fibrils by MMP-8. J Mol Biol 425(10):1815–1825. doi:10.1016/j.jmb.2013.02.002
Horstmann S, Kalb P, Koziol J et al (2003) Profiles of matrix metalloproteinases, their inhibitors, and laminin in stroke patients: influence of different therapies. Stroke 34(9):2165–2170. doi:10.1161/01.STR.0000088062.86084.F2
Beilin B, Shavit Y, Razumovsky J et al (1998) Effects of mild perioperative hypothermia on cellular immune responses. Anesthesiology 89(5):1133–1140
Sido B, Teklote J, Hartel M et al (2004) Inflammatory response after abdominal surgery. Best Pract Res Clin Anaesthesiol 18(3):439–454
Ahrendt GM, Tantry US, Barbul A (1996) Intra-abdominal sepsis impairs colonic reparative collagen synthesis. Am J Surg 171(1):102–107. doi:10.1016/S0002-9610(99)80082-8, discussion 107–8
Naycı A, Cömelekoğlu U, Cıngı E et al (2005) Splenektomi yapılan sıçanlarda sepsis kolon anastomozunun iyileşmesini olumsuz etkiler mi? (Does sepsis impair the healing of colonic anastomosis in splenectomized rats?). Ulus Travma Acil Cerrahi Derg 11(4):282–286
Conflict of interest
Drs. Torben Glatz, Sylvia Timme, Birte Kulemann, Gabriel Seifert, Philipp Anton Holzner, Jodok Matthias Grüneberger, Simon Küsters, Sophia Chikhladze, Johannes Boldt, Olivia Sick, PD Dr. med. Jens Höppner, Prof. Dr. med. Ulrich Theodor Hopt, and PD Dr. med. Goran Marjanovic have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Glatz, T., Boldt, J., Timme, S. et al. Impact of intraoperative temperature and humidity on healing of intestinal anastomoses. Int J Colorectal Dis 29, 469–475 (2014). https://doi.org/10.1007/s00384-014-1832-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-014-1832-z