Abstract
Background
Several studies have confirmed that laparoscopic colorectal surgery results in improved early post-operative outcomes. Nevertheless, conventional laparoscopic approach and instruments have several limitations. Robotic approach could potentially address of many of these limitations.
Objectives
This review aims to present a summary of the current evidence on the role of robotic colorectal surgery.
Methods
A comprehensive search of electronic databases (Pubmed, Science Direct and Google scholar) using the key words “rectal surgery”, “laparoscopic”, “colonic” and “robotic.” Evidence from these data was critically analysed and summarised to produce this article.
Results
Robotic colorectal surgery is both safe and feasible. However, it has no clear advantages over standard laparoscopic colorectal surgery in terms of early postoperative outcomes or complications profile. It has shorter learning curve but increased operative time and cost. It could offer potential advantage in resection of rectal cancer as it has a lower conversion rates even in obese individuals, distal rectal tumours and patients who had preoperative chemoradiotherpy. There is also a trend towards better outcome in anastomotic leak rates, circumferential margin positivity and perseveration of autonomic function, but there was no clear statistical significance to support this from the currently available data.
Conclusion
The use of robotic approach seems to be capable of addressing most of the shortcomings of the standard laparoscopic surgery. The technique has proved its safety profile in both colonic and rectal surgery. However, the cost involved may restrict its use to patients with challenging rectal cancer and in specialist centres.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several randomised controlled studies (RCTs) [1–3] and review articles [4, 5] have confirmed that laparoscopic colorectal surgery (LCS) results in improved early post-operative outcomes in terms of reduced intraoperative blood loss as well as postoperative pain, ileus and hospital stay. These studies have also confirmed that LCR results in comparable oncological outcomes when compared with open surgery, with some studies suggesting that LCS could result in higher lymph node retrieval, which is particularly relevant in resection of malignant disease.
These observations indicate that the laparoscopic approach, particularly for colonic resections, might become the golden standard in the near future [6]. Nevertheless, the conventional laparoscopic approach and instruments are known to have several limitations. These limitations include assistant-dependent unstable two-dimensional view, inability to perform high-precision suturing, poor ergonomics and fixed tips with limited dexterity of surgical instruments. These limitations are particularly relevant during rectal dissection in the confines of the pelvis as they result in difficult retraction, crowding and clashing of instruments. An experienced assistant is often essential, and the operative view is often further limited by fumes from energy sources in the confined spaces of the pelvis often results in fogging of the camera that could slow the progress of already a technically demanding procedure [7–10].
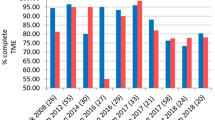
The limitations of standard laparoscopic approach in rectal surgery have always been attributed, at least in part, to the experience and the learning curve of the operator [6]. However, the recently published COLOR II (COlon cancer Laparoscopic or Open Resection) study [11] showed that laparoscopic rectal surgery continues to be demanding even in the hand of highly experienced laparoscopic surgeons. It was interesting to note that, despite the extensive laparoscopic experience of the operating teams participating in the study and almost two decades of continuous equipment improvements, the authors reported conversion rate of 17 %. Moreover, a recent systematic review [12] that included all the published studies on laparoscopic rectal cancer surgery over the last 20 years failed to show clear trend towards improvement in the early post-operative outcomes over time. The lack of clear trend of improvement in the rate of postoperative complications despite 20 years of practice of laparoscopic rectal surgery indicates that other factors, apart from the learning curve, could be involved such as limitations of the current laparoscopic equipment.
Some surgeons believe that the robotic approach could address of many of the limitations of standard laparoscopic rectal surgery [13–15], and consequently, there has been steady increase in the adoption of the robotic technique in colorectal surgery. Even though the robotic approach has been mainly used for rectal surgery [16], there has been slow implementation of its use in colonic surgery as well [17]. This review aims to present a summary of the current evidence on the role of robotic colorectal surgery.
Methods
A comprehensive search of electronic databases (Pubmed, Science Direct and Google scholar) using the key words “rectal surgery”, “laparoscopic”, “colonic” and “robotic.” The reference lists provided by the identified articles were additionally hand-searched for additional studies missed by the search strategy, and this method of cross-referencing was continued until no further relevant publications were identified. Evidence from these data was critically analysed and summarised to produce this article.
All studies reporting outcomes on robotic colorectal resections were included in the review process. The available published data on robotic colorectal surgery comprise nonrandomised retrospective case comparison series, case series and case reports. The studies were subject to significant bias, both in terms of the selection criteria for the study participants and also the reporting of data.
Result
Potential advantages of robotic surgery
The use of robotic surgery could potentially address most of the known limitations of conventional laparoscopic surgery while at the same time preserving all the advantages of the minimally invasive approach [13–15]. The robotic system offers a camera system that is controlled by the operating surgeon combined with three-dimensional tenfold magnification vision, resulting in exceptionally clear still visibility of the operative field [18–20]. Robotic approach has particular advantage during pelvic dissection as the surgeon gets equal access to both sides of the pelvis [21]. The tips of the instruments of a robotic arm gives unprecedented range of movements as it have an endowrist that has functions of 7 degrees of freedom, 180° articulation and 540° rotation [20]. Additionally, the presence of multiarticulated instruments permits a range of angles to approach the rectum from different directions, thus allowing sharp dissection around the lower part of the rectum and mesorectum. The robotic handles transfer the hand movements of the surgeon to the tip of the instruments, offering a comfortable, ergonomically ideal operating position [22]. A number of studies confirmed robotic surgery results in reduced physical strain for the operating surgeon [21]. In addition, robotic technology offers unique features such as motion scaling and remote telesurgical applications including telementoring [23].
Limitations of the current robotic systems
Manufacturers of future generations of robotic systems should attempt to address some of the limitations of the currently available systems. Robotic systems require precise positioning for optimal operative outcome and to avoid robotic arm collision. The docking and separation procedure of a robotic cart from the patient is known to be a time consuming procedure. Additionally, the position of the patient cannot be changed without undocking the robotic arms [21]. Also, repeated docking and undocking of the robot is often needed when using the robot to perform a surgical procedure in different compartments in the abdominal cavity. This results in prolonged operating time when compared with standard laparoscopic surgery [24]. The time taken in undocking the robot could result in major concern when immediate open conversion is needed for serious life-threatening intra-operative bleeding delayed separation of the robotic cart could potentially result in a difficult situation [20].
One of the other major shortcomings in the current robotic systems is lack of both tactile sensation and tensile feedback to the operating surgeon. Consequently, tissue damage can occur easily if excessive traction was applied by the robotic arm and during movement of the robotic instrument [20]. Therefore, the surgeon has to acquire the skill of using visual cues to estimate the amount of tension applied on the tissues [21]. Therefore, great care must be taken to avoid traumatic injuries when handling bowel. This might be of particular relevance in colonic surgery. However, it is interesting to note that iatrogenic colonic injury from excessive traction during surgery has not been reported in any of the studies included in a recent systematic review on robotic colonic surgery [24]. This might reflect the extensive experience in minimally invasive approach for the units currently adopting robotic colorectal surgery, and the complication pattern from the currently available literature might not necessarily mirror the complication pattern in the wider surgical community. Similarly, the same caution should be taken during endoscopic suturing as the suture material can be cut during suturing because there is no tensile feedback to the robotic instrument [20].
Approaches & outcomes of robotic colorectal surgery
Approaches to robotic colonic surgery
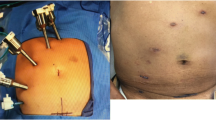
There are subtle variations in the reported approach for robotic colonic resections as there were variations in port position and number. The majority of surgeons in the published literature used between three to six ports [24]. There was one case report of a robotic SILS right hemicolectomy [25].
Specimen extraction was through a Pfannenstiel incision [26–28], a mini-laparotomy over the umbilicus [8, 29] or oblique abdominal incision via left or right hypochondrium or iliac fossa [8, 30].
Robotic right hemicolectomy
Most authors position the patient in a supine Trendelenburg with left-tilted position and a pneumoperitoneum of 12 mmHg. Most surgeons use five ports to perform the procedure: one 12-mm port for the camera, three 8-mm ports for the robotic and another 5-mm port for the assistant. As expected, there are variations in port positions [26, 31]. Dissection has been described, similar to standard laparoscopic surgery, with medial to lateral approach or alternatively inferior to superior approach.
Robotic left hemicolectomy
Again, there are subtle variations in reported technique of robotic left colectomy. Generally, the procedure is often performed with the patient in a supine modified lithotomy position, with the anterior thighs positioned in the same plane as the anterior abdominal wall. There are variations in the reported positions of the trocars, but generally the procedure is performed through a total of four [32] or five trocars [31]. Following mobilisation of the splenic flexure and left colon, division of the inferior mesenteric vein for malignant resections is done. The robot is then disengaged; the patient is placed in Trendelenburg position, and the robot is re-docked from the left hip; the sigmoid colon is elevated, and the inferior mesenteric vascular pedicle division is completed. The rectosigmoid colon is then mobilised circumferentially down to the desired level on the rectum while visualising both ureters. At this point, the robot is disengaged, and endoscopic staplers are used to divide the rectum. The suprapubic port is extended to accommodate extraction of the specimen followed by stapled anastomosis [31].
Approaches to robotic rectal surgery
There are several techniques for robotic rectal cancer surgery described in the surgical literature.
Multiple stages totally robotic technique
This is described as either a two-stage or a three-stage procedure with the number of stages reflecting the number of movements of the robotic cart. The repeated docking and undocking of the robot clearly increases the overall operating time [28].
Hybrid technique
To eliminate the need for repeated repositioning of the robotic system, many surgeons prefer conventional laparoscopic mobilisation of the left colon and splenic flexure as well as division of the inferior mesenteric vessels and then use of the robotic approach for the total mesorectal excision (TME) part of the operation, only because the main advantages of robotic-assisted approach are evident during rectal dissection in the confines of the pelvis. This hybrid approach saves time as it avoids the need for repeated robotic setup. On average, the TME part of the procedure is reported to take around of 60 min [21, 33].
Single-stage totally robotic
This approach has been recently reported, and it aims to abolish the need for repeated docking and undocking of the robot but at the same time preserves the advantages of the use of the robotic approach for the whole procedure [34].
Supporters of the totally robotic approach, whether multiple stage or single stage, believe that robotic dissection around the IMA pedicle is an essential step of the procedure to help identification and preservation the periaortic nerves. They correctly believe that preservation of both pelvic and periaortic nerves is important in avoiding postoperative sexual/bladder dysfunction. They also recommend that the use of robotics could also help easier splenic flexure mobilisation [34].
Learning curve in robotic rectal surgery
The laparoscopic approach to colorectal surgery is known to be technically challenging with relatively long and demanding learning curve [5, 35]. It has been recommended that surgeons should initially attempt performing laparoscopic resections for benign colorectal pathology only. The second step in the learning curve is undertaking colonic cancer resections in highly selected and relatively straightforward patients. Only then should surgeons attempt building their proficiency in laparoscopic TME, and it is recommended that they should start with female patients with T1–T2 high rectal cancer, followed by abdominoperineal resections. Performing laparoscopic TME in male patients with mid-rectal cancer should only be attempted after gaining ‘adequate’ experience. The exact number of cases suggested prior to attempting laparoscopic TME in potentially challenging cases (male/obese patients) has been suggested to range from 30 to 100 cases. This highlights the technically demanding nature of rectal surgery in general and the minimally invasive approach in particular [6].
Many surgeons argue that the three-dimensional view and the ability of the robot to transfer the surgeon’s hand movements to the tips of the surgical instruments makes the learning curve for robotic surgery much shorter than that for laparoscopic colorectal surgery. Therefore, it has been suggested that an inexperienced laparoscopic surgeon is able to operate with the robot safely [21]. This is particularly relevant for distal rectal cancers as the robot offers excellent views during deep pelvic dissection [36]. Also, robotic surgery requires similar cluster of skills for those used in open surgery and thus the learning curve at the console is relatively short [37].
The learning curve of robotic-assisted technology entails the surgeon’s mastery of initial several unique skills to overcome the loss of tensile and tactile feedback by recognising visual cues. Also, the surgeon should conceptualise the spatial relationships of robotic instruments outside the active field of view and mentally visualising the spatial relationships of the robotic arms and cart while operating at the console [38].
To facilitate the acquisition of robotic unique skills in a safe and stepwise manner, the surgeon should ideally has standard laparoscopic skills before using the robotic approach [38]. The learning curve could be divided into three phases. The first phase represents the initial part of the learning curve, and it includes 15 cases. The second phase includes an additional ten cases to allow the consolidation of the additional experience. The third phase is related to the post-learning period when the surgeon can start offering robotic surgery for a more complex and challenging cases. The available data suggest that, after a learning curve phase that involves of 15 to 25 cases, the surgeon may achieve a higher level of competence and consider using robotic surgery for patients presenting with more difficult cases safely [38]. This learning curve suggested by the authors is definitely much shorter compared with the suggested learning curve associated with standard LCS [6].
Cost implications of robotic colorectal surgery
Most, if not all, healthcare systems are currently under undue financial pressure. To accept newly developing surgical techniques, it should not only be safe but it should also prove its cost-effectiveness.
Even though LCS has increased intraoperative cost when compared with open colorectal surgery (OCS), the overall cost of LCS has been shown to be comparable to that of OCS due to reduction in the cost of post-operative care consequent to reduced post-operative hospital stay. Moreover, when the cost of standard LCS is analysed over time, it is projected that the results of future economic evaluations will unequivocally show that standard LCS is cheaper than open surgery due to the expected gradual drop in the cost of equipment, particularly when practiced in Western health care systems where postoperative care cost is high [39].
High capital and running costs of the currently available robotic system have limited its uptake in many countries. Combing the capital cost of the robotic system and the disposable instruments is a major issue when cost-effectiveness of robotic surgery is discussed [20]. Even though it is anticipated that the capital and running costs for the robotic systems might decrease in the future, it is likely that robotic colorectal surgery costs will always remain higher than those of open or laparoscopic colorectal surgery as the main savings in minimally invasive approach comes from reduction in hospital stay. There is no reason to anticipate that robotic colorectal surgery would result in reduced hospital stay when compared on laparoscopic colorectal surgery except, perhaps, through reduction in conversion rates in the more challenging cases of male, obese, or lower two thirds rectal tumours [16].
Outcomes of robotic colonic surgery
A recent systematic review of the early postoperative outcomes of robotic colonic surgery confirms that the current evidence has shown both feasibility and a safety profile comparable to standard laparoscopic colonic surgery [24]. However, when the results of robotic colonic surgery were compared with data from five large multiport laparoscopic colonic surgery cohort studies [1–3, 40, 41], it becomes evident that the median length of post-operative stay and time to first bowel movement were comparable. Robotic colonic group showed a greater median lymph node harvest and clearly robotic resections took longer time to perform.
The morbidity data suggest that robotic colonic surgery has a favourable complication profile compared with multiport laparoscopic surgery [24]. However, it should be noted that these results are subject to significant selection bias, as surgeons building their experience with robotic colonic surgery would probably tend to select relatively straightforward cases in the early part of their learning curve. Also, bias towards complication reporting would preclude meaningful comparisons. Finally, most centres performing robotic colonic resections are often have extensive experience in standard laparoscopic surgery, and surgeons in those centres are expanding on their advanced laparoscopic skills by adopting the robotic approach. It should be noted that data from those five large multiport laparoscopic colonic surgery studies [1–3, 40, 41] represented the relatively ‘early’ part of the learning curve for most of the participating surgeons as there was an under-estimation of the length learning curve at that time [6, 42]. Nonetheless, the currently available data did show that robotic colonic surgery could be a safe procedure when undertaken in selected patients and surgical centres [24].
Cost is one of the main concerns regarding robotic colonic surgery. For the reasons explained earlier, it is very unlikely that robotic colonic surgery will be cheaper than standard laparoscopic colorectal surgery in the future. It would also be difficult to recommend the adoption of the robotic approach for colonic resection based on the argument that robotic surgery has a relatively short learning curve. Various studies have shown that the learning curve for laparoscopic colonic surgery is not exceptionally long [43], and, more importantly, the skills acquired are transferable to the other current or future procedures in minimally invasive colorectal surgery, e.g. transanal minimally invasive surgery (TAMIS) [44]. Whether the general surgical community should embark on a new learning curve for robotic colonic surgery to universally adopt the robotic approach as a standard in colonic surgery can only be answered in the light of future studies. However, the current evidence does not certainly support this [24].
Outcomes of robotic rectal surgery
A recent systematic review on the studies reporting the use of the robotic approach for resection of rectal cancer failed to show clear significant reduction in early post-operative complications when compared with standard laparoscopic surgery with only potentially better short-term outcomes when applied in selected patients such as obesity, male sex, preoperative radiotherapy and tumours in the lower two thirds of the rectum [16].
Surgeon’s experience and learning curve
In most of the published literature, robotic rectal surgery were performed by experienced laparoscopic colorectal surgeons. However, in one multicentre study [45], the enrolled surgeons had different expertise in laparoscopic colorectal surgery. Interestingly, in one of the participating centres, the surgeons did not have any prior experience in standard laparoscopic colorectal surgery before the use of Da Vinci System. Nevertheless, the transfer of surgical skills in open TME to the robotic was rapid, and the operative time reduced during the first 20 cases [45]. These results suggest robotic rectal surgery has a shorter learning curve when compared with standard laparoscopic rectal surgery.
Conversion rate
Reported conversion rates in robotic rectal procedures ranged from 1 % to 7.3 % [16] which definitely compares favourably with conversion rate of 29 % in the CLASSIC trial [2]. The relatively high conversion rate in the CLASSIC trial has been attributed to the effect of learning curve, and this was evident by the reduction in the conversion rates for every year of the study which in itself taken as an indication that the learning curve was functional during the trial [2].
However, the recently published COLORII study reported conversion rates of 17 % despite the extensive laparoscopic experience of the participating surgeons [11]. These observations indicate that the robotic approach might result in lower conversion rates or allow tackling of more difficult or challenging cases. This inference could be supported by Patriti et al. [46] study which reported a conversion rate of 19 % in the laparoscopic group compared with no conversion in the robotic group. In the same study, the majority of the patients in the robotic group had previous abdominal surgery and also had distal rectal cancer requiring a complete TME. In addition, the number of patients who underwent neoadjuvant chemo-radiotherapy was higher in the robotic group. Commonly reported reasons for conversion were locally advanced tumour, bulky mesorectum for obesity, high BMI, narrow pelvis, adhesions from previous surgery and limitations of the laparoscopic instruments. Therefore, it has been suggested that patients with previous abdominal surgery, lower rectal cancers and previous chemo-radiotherapy may justify a robotic approach [16].
Operating time
Most of the studies report longer operating time for robotic rectal surgery. However, it is interesting to note that, in two comparative studies, the authors found a shorter operating time in the robotic group compared with the standard laparoscopic surgery [47]. The operating time still represents a disadvantage of robotic surgery; however, this might be overcome with increased experience.
Anastomotic leakage
The anastomotic leakage represents one of the most dreaded complications following rectal cancer surgery. Several studies report an increased leakage rate in lower rectal cancer and obese patients, especially if they receive neoadjuvant chemo-radiotherapy previous surgery [21, 23, 48–50]. Overall, the reported median anastomotic leakage of 7.6 % (range,1.8–13.5 %) for robotic procedures compared with a median anastomotic leakage was 7.3 % (range, 2.4–11.2 %) for those performed by standard laparoscopy. This highlights that there was no increased anastomotic leak in the robotic group even though higher number of patients in this group received preoperative chemo-radiotherapy [16].
Data from individual studies are contradictory, as three comparative studies [23, 33] found a lower rate of anastomotic leakage in the robotic group with no statistical difference. Conversely, Baek et al. [47] reported a leakage rate of 8.6 % for the robotic procedures versus a rate of 2.9 % for those cases performed laparoscopically with no statistical difference (p = 0.62).
Oncological data
In several comparative studies, the circumferential margin positive rate and the mean of distal resection margin did not differ significantly between robotic and laparoscopic procedures. However, it should be noted that surgeons tended to use the robotic approach for the more challenging rectal tumours, and yet this was not reflected in increased rate of positive resection margins. Across several studies, the number of lymph nodes harvested ranged from 10.3 and 20 in the robotic group and from 11.2–21 in the laparoscopic group with no significant difference in both groups [16].
Autonomic nerves preservation
Sexual dysfunction
Reporting of erectile dysfunction is rather inconsistent in the available literature [16]. Patriti et al. [46] reported erectile dysfunction rate of 5.5 % and 16.6 % in the robotic and laparoscopic group, respectively, with no statistical difference (p > 0.05). Erectile dysfunction did not seem to be correlated with the extent of mesorectal dissection or location of the tumour. Erectile dysfunction was more correlated with a bulky tumour and the complexity of the mesorectal dissection [46].
Urinary retention
Urinary dysfunction seems to be of a less problem following minimally invasive rectal dissection. In three studies, no urinary dysfunction were identified in the robotic group [48, 51, 52]. In the other studies [21, 46, 53], the median urinary retention range was 2.6 % in the robotic group and from 2.4 % in the laparoscopic group with no significant difference.
Faecal incontinence
Limited data are available regarding this complication. Patriti et al. [46] reported 2.7 % and 6.8 % of faecal incontinence rate in the laparoscopic and in the robotic groups, respectively, with no significant difference. In a second study, none out of the 118 patients included in the analysis experienced this complication in both groups [48].
Cost
Overall, the cost of robotic rectal procedures was higher than the cost of laparoscopic procedures [16]. Leong et al. reported a cost three times higher for robotic surgery than the cost for conventional laparoscopic surgery [49]. Kim et al. [23] reported total hospital costs of 14,080 USD in robotic surgery, 9,120 USD in laparoscopy surgery and 8,386 USD in open surgery (p < 0.01). Nevertheless, the cost implications might be justified for the more difficult or challenging rectal cancer resections as, otherwise, these patients would require open surgery or have increased probability of conversion following standard laparoscopic surgery with its known implication of increased risk of post-operative complications. The disadvantage of the cost may be overcome in the future by limiting the use of robotic surgery to specialist centres to allow high volume use of the capital investment in buying the robot [54].
Newly emerging techniques in robotic colorectal surgery
There are few reports on some novel techniques in minimally invasive colorectal surgery using the robotic approach including robotic TAMIS [55], transanal endoscopic robotic surgery [56] and robotic rectopexy [57]. However, due to the limited number of publications, no clear evidence could be concluded from these studies.
Ongoing major clinical trails
Due to the limited evidence from RCT to support the use of robotic-assisted surgery for rectal cancer, the RO-botic versus LAparoscopic Resection for Rectal cancer (ROLARR) trial has been designed to address this issue. This is an international, multicentre, prospective, randomised, controlled, unblinded, parallel-group trial of robotic-assisted versus laparoscopic surgery for the curative treatment of rectal cancer. The study will perform a detailed analysis of robotic-assisted rectal cancer surgery against conventional laparoscopic rectal cancer resection by means of a randomised, controlled trial.
Conclusion
The use of robotic approach is clearly an exciting development in the field of colorectal surgery as the technique seems to be capable of addressing most of the shortcomings of the standard laparoscopic surgery. The technique has proved its safety profile in both colonic and rectal surgery. However, the cost involved may restrict its use to patients with challenging rectal cancer and in specialist centres.
References
Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM et al (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet 359(9325):2224–2229
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AMH et al (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365(9472):1718–1726
Veldkamp R, Kuhry E, Hop WCJ, Jeekel J, Kazemier G, Bonjer HJ et al (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6(7):477–484
Abraham NS, Young JM, Solomon MJ (2004) Meta-analysis of short-term outcomes after laparoscopic resection for colorectal cancer. Br J Surg 91(9):1111–1124
Aly EH (2009) Laparoscopic colorectal surgery: summary of the current evidence. Ann R Coll Surg Engl 91(7):541–544
Maggiori L, Panis Y (2013) Is it time for a paradigm shift: “laparoscopy is now the best approach for rectal cancer”? Transl G doi: 10.3978/j.issn.2224-4778.2013.05.38
Lee SW (2009) Laparoscopic procedures for colon and rectal cancer surgery. Clin Colon Rectal Surg 22(4):218–224
Delaney CP, Lynch AC, Senagore AJ, Fazio VW (2003) Comparison of robotically performed and traditional laparoscopic colorectal surgery. Dis Colon Rectum 46(12):1633–1639
Choi DJ, Kim SH, Lee PJM, Kim J, Woo SU (2009) Single-stage totally robotic dissection for rectal cancer surgery: technique and short-term outcome in 50 consecutive patients. Dis Colon Rectum 52(11):1824–1830
Cecil TD, Taffinder N, Gudgeon AM (2006) A personal view on laparoscopic rectal cancer surgery. Color Dis Off J Assoc Coloproctol Gt Br Irel 8(3):30–32
Van der Pas MH, Haglind E, Cuesta MA, Fürst A, Lacy AM, Hop WC, et al. (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol.
Shearer R, Gale M, Aly OE, Aly EH. (2013) Have early post-operative complications from laparoscopic rectal cancer surgery improved over the past 20 years? Color. Dis. Off. J. Assoc. Coloproctology Gt. Br. Irel.
Baik SH, Ko YT, Kang CM, Lee WJ, Kim NK, Sohn SK et al (2008) Robotic tumor-specific mesorectal excision of rectal cancer: short-term outcome of a pilot randomized trial. Surg Endosc 22(7):1601–1608
Baik SH, Lee WJ, Rha KH, Kim NK, Sohn SK, Chi HS et al (2008) Robotic total mesorectal excision for rectal cancer using four robotic arms. Surg Endosc 22(3):792–797
Spinoglio G, Summa M, Priora F, Quarati R, Testa S (2008) Robotic colorectal surgery: first 50 cases experience. Dis Colon Rectum 51(11):1627–1632
Scarpinata R, Aly EH (2013) Does robotic rectal cancer surgery offer improved early postoperative outcomes? Dis Colon Rectum 56(2):253–262
Fung AK-Y, Aly EH (2012) Systematic review of single-incision laparoscopic colonic surgery. Br J Surg 99(10):1353–1364
Ballantyne GH, Moll F (2003) The da Vinci telerobotic surgical system: the virtual operative field and telepresence surgery. Surg Clin North Am 83(6):1293–1304, vii
Lanfranco AR, Castellanos AE, Desai JP, Meyers WC (2004) Robotic surgery: a current perspective. Ann Surg 239(1):14–21
Baik SH (2008) Robotic colorectal surgery. Yonsei Med J 49(6):891–896
Hellan M, Anderson C, Ellenhorn JDI, Paz B, Pigazzi A (2007) Short-term outcomes after robotic-assisted total mesorectal excision for rectal cancer. Ann Surg Oncol 14(11):3168–3173
Stylopoulos N, Rattner D (2003) Robotics and ergonomics. Surg Clin North Am 83(6):1321–1337
Kim N-K, Kang J (2010) Optimal total mesorectal excision for rectal cancer: the role of robotic surgery from an expert’s view. J Korean Soc Coloproctol 26(6):377–387
Fung AK-Y, Aly EH (2013) Robotic colonic surgery: is it advisable to commence a new learning curve? Dis Colon Rectum 56(6):786–796
Ragupathi M, Ramos-Valadez DI, Pedraza R, Haas EM (2010) Robotic-assisted single-incision laparoscopic partial cecectomy. Int J Med Robot Comput Assist Surg Mrcas 6(3):362–367
Park JS, Choi G-S, Park SY, Kim HJ, Ryuk JP (2012) Randomized clinical trial of robot-assisted versus standard laparoscopic right colectomy. Br J Surg 99(9):1219–1226
Weber PA, Merola S, Wasielewski A, Ballantyne GH (2002) Telerobotic-assisted laparoscopic right and sigmoid colectomies for benign disease. Dis Colon Rectum 45(12):1689–1694, discussion 1695–1696
D’Annibale A, Pernazza G, Morpurgo E, Monsellato I, Pende V, Lucandri G et al (2010) Robotic right colon resection: evaluation of first 50 consecutive cases for malignant disease. Ann Surg Oncol 17(11):2856–2862
DeSouza AL, Prasad LM, Park JJ, Marecik SJ, Blumetti J, Abcarian H (2010) Robotic assistance in right hemicolectomy: is there a role? Dis Colon Rectum 53(7):1000–1006
Averbach M, Popoutchi P, Marques OW Jr, Abdalla RZ, Podgaec S, Abrão MS (2010) Robotic rectosigmoidectomy—pioneer case report in Brazil. Current scene in colorectal robotic surgery. Arq Gastroenterol 47(1):116–118
Baik SH. Robot surgery [Internet]. Rijeka, Croatia: In: Tech; 2010 [cited 2013 Jun 19]. Available from: http://www.intechopen.com/books/show/title/robot-surgery
DeNoto G, Rubach E, Ravikumar TS (2006) A standardized technique for robotically performed sigmoid colectomy. J Laparoendosc Adv Surg Tech A 16(6):551–556
Baik SH, Kwon HY, Kim JS, Hur H, Sohn SK, Cho CH et al (2009) Robotic versus laparoscopic low anterior resection of rectal cancer: short-term outcome of a prospective comparative study. Ann Surg Oncol 16(6):1480–1487
Kwak JM, Kim SG (2012) The technique of single-stage totally robotic low anterior resection. J Robotic Surg 5:2
Aly EH (2013) Have we improved in laparoscopic resection of rectal cancer: critical review. doi: 10.3978/j.issn.2224-4778.2013.03.03
Abodeely A, Lagares-Garcia JA, Duron V, Vrees M (2010) Safety and learning curve in robotic colorectal surgery. J Robot Surg 4(3):161–165
Giulianotti, P. C.; Coratti, A.; Angelini, M.; et al. (2003) Robotics in general surgery: personal experience in a large community hospital. Arch Surg 138:777-784
Bokhari MB, Patel CB, Ramos-Valadez DI, Ragupathi M, Haas EM (2011) Learning curve for robotic-assisted laparoscopic colorectal surgery. Surg Endosc 25(3):855–860
Aly OE, Quayyum Z (2012) Has laparoscopic colorectal surgery become more cost-effective over time? Int J Colorectal Dis 27(7):855–860
Clinical Outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350(20):2050–2059
Schwenk W, Haase O, Neudecker J, Müller JM (2005) Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev Online 3, CD003145
Simons AJ, Anthone GJ, Ortega AE, Franklin M, Fleshman J, Geis WP et al (1995) Laparoscopic-assisted colectomy learning curve. Dis Colon Rectum 38(6):600–603
Köckerling F, Scheidbach H, Schneider C, Bärlehner E, Köhler L, Bruch HP et al (2000) Laparoscopic abdominoperineal resection: early postoperative results of a prospective study involving 116 patients. The Laparoscopic Colorectal Surgery Study Group. Dis Colon Rectum 43(11):1503–1511
Albert MR, Atallah SB, DeBeche-Adams TC, Izfar S, Larach SW (2013) Transanal minimally invasive surgery (TAMIS) for local excision of benign neoplasms and early-stage rectal cancer: efficacy and outcomes in the first 50 patients. Dis Colon Rectum 56(3):301–307
Pigazzi A, Luca F, Patriti A, Valvo M, Ceccarelli G, Casciola L et al (2010) Multicentric study on robotic tumor-specific mesorectal excision for the treatment of rectal cancer. Ann Surg Oncol 17(6):1614–1620
Patriti A, Ceccarelli G, Bartoli A, Spaziani A, Biancafarina A, Casciola L (2009) Short- and medium-term outcome of robot-assisted and traditional laparoscopic rectal resection. Jsls J Soc Laparoendosc Surg Soc Laparoendosc Surg 13(2):176–183
Baek J-H, Pastor C, Pigazzi A (2011) Robotic and laparoscopic total mesorectal excision for rectal cancer: a case-matched study. Surg Endosc 25(2):521–525
Kwak JM, Kim SH, Kim J, Son DN, Baek SJ, Cho JS (2011) Robotic vs laparoscopic resection of rectal cancer: short-term outcomes of a case–control study. Dis Colon Rectum 54(2):151–156
Leong QM, Son DN, Cho JS, Baek SJ, Kwak JM, Amar AH et al (2011) Robot-assisted intersphincteric resection for low rectal cancer: technique and short-term outcome for 29 consecutive patients. Surg Endosc 25(9):2987–2992
Leong QM, Kim SH (2011) Robot-assisted rectal surgery for malignancy: a review of current literature. Ann Acad Med Singapore 40(10):460–466
Ng KH, Lim YK, Ho KS, Ooi BS, Eu KW (2009) Robotic-assisted surgery for low rectal dissection: from better views to better outcome. Singapore Med J 50(8):763–767
Park JS, Choi G-S, Lim KH, Jang YS, Jun SH (2010) Robotic-assisted versus laparoscopic surgery for low rectal cancer: case-matched analysis of short-term outcomes. Ann Surg Oncol 17(12):3195–3202
Kang J, Min BS, Park YA, Hur H, Baik SH, Kim NK et al (2011) Risk factor analysis of postoperative complications after robotic rectal cancer surgery. World J Surg 35(11):2555–2562
Hottenrott C (2011) Robotic versus laparoscopic surgery for rectal cancer and cost-effectiveness analysis. Surg Endosc 25(12):3954–3956, author reply 3957–3958
Atallah SB, Albert MR, de Beche-Adams TH, Larach SW (2011) Robotic transanal minimally invasive surgery in a cadaveric model. Tech Coloproctology 15(4):461–464
Hompes R, Rauh SM, Hagen ME, Mortensen NJ (2012) Preclinical cadaveric study of transanal endoscopic da Vinci® surgery. Br J Surg 99(8):1144–1148
Buchs NC, Pugin F, Ris F, Volonte F, Morel P, Roche B. (2013) Early experience with robotic rectopexy. Int. J. Med. Robot. Comput. Assist. Surg. MRCAS. DOI: 10.1002/rcs.1498
Disclaimers
None
Sources of finance
None
Submission for poster/presentation/conference
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contribution: Conception and writing the manuscript.
Rights and permissions
About this article
Cite this article
Aly, E.H. Robotic colorectal surgery: summary of the current evidence. Int J Colorectal Dis 29, 1–8 (2014). https://doi.org/10.1007/s00384-013-1764-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-013-1764-z