Abstract
Background
Several studies have confirmed that laparoscopic colorectal surgery (LCS) has superior short-term outcomes when compared to open colorectal surgery. However, the evidence for cost-effectiveness of LCS is less clear.
Aim
The aim of this study is to explore the cost-effectiveness of LCS over time since it was first developed in 1991.
Methods
Systematic review of the literature was conducted. Electronic databases (PubMed, ScienceDirect and Google Scholar) were searched for studies from 1991 to 2010 using the keywords “laparoscopic, colorectal surgery cost, economic evaluation”.
Results
Fifteen economic evaluations met the inclusion criteria. The percentage cost difference between open and laparoscopic surgery varied widely between different studies. The general trend when observing all the included economic evaluations is that there is a moderate negative correlation between progression of time and the size of the cost gap between laparoscopic and open surgery (R-value = −0.44). This correlation is even stronger (R-value = −0.64, P = 0.046) if the studies are subdivided by the country where the surgery was carried out in. Western healthcare systems, even though they had a heterogeneous set of results (SD = 27%), showed a decline in costs of laparoscopic surgery with time.
Conclusion
From the current trends, it is projected that the results of future economic evaluations will unequivocally show that laparoscopic surgery is cheaper than open surgery. The initial higher costs of laparoscopic surgery training may be worth the savings made in the long term if it is practised in settings where postoperative care is expensive.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer is the second most common malignancy in England and Wales in terms of both incidence and mortality. Approximately 36,000 new patients were diagnosed in 2002 and 17,000 people died from colorectal cancer in the same year. About 80% of all patients diagnosed with colorectal cancer underwent surgery [1].
For several decades, open colorectal surgery (OCS) has been the standard method for surgical removal of primary colorectal tumours. Minimally invasive approaches to treat colorectal diseases were developed to take advantage of the benefits observed in laparoscopic procedures elsewhere in the gastrointestinal tract. A minimally invasive procedure is defined as any procedure (surgical or otherwise) that is less invasive than open surgery used for the same purpose [2]. However, the safety and cost-effectiveness of each procedure must be demonstrated with randomised controlled trials.
Open surgical resection of primary colorectal tumour is the most common procedure for treating colorectal cancer. However, morbidity rates associated with this can be high. As laparoscopic surgery is less invasive, it is therefore likely to lead to a more rapid recovery from the operation. It has also been suggested that the reduced trauma associated with laparoscopic procedures might minimise any disruption to the immune system caused by surgery and hence reduce the risk of recurrence [2]. Other disadvantages associated with open colorectal surgery include the following: incisional pain, intraoperative and postoperative metabolic stress, tissue trauma and postoperative ileus from manual intestinal manipulation [3]. It has been postulated that laparoscopic surgery may reduce the impact of these. If so, this might justify the apparent increase in interest amongst surgeons to introduce laparoscopic techniques to treat colorectal cancer.
Jacobs et al. [4] reported the first series of laparoscopic colonic resections in 20 patients in 1991. However, laparoscopic colectomy has not been accepted quickly as laparoscopic as other laparoscopic procedures. This was because of its steep learning curve, unstudied clinical outcomes, absence of randomised controlled trials (RCTs) and concerns about its costs in the already financially strained health systems [5]. To justify the routine use of laparoscopy in the management of colorectal cancer, it must be proven to be both clinically safe and cost-effective.
Clinical effectiveness
Abraham et al. [6] reported the outcome of the meta-analysis of RCTs till 2002. They compared the short-term outcomes of laparoscopic resection and open resection for colorectal cancer. They included 12 RCTs with a combined total of 2,521 procedures. Laparoscopic resection took 30% more time to perform but had less morbidity, earlier return of bowel function, reduced analgesia requirements and reduced hospital stay. There was no difference in mortality or cancer clearance. This study concluded that laparoscopic resection for colorectal cancer is associated with better short-term outcomes without compromising oncological clearance.
Cost-effectiveness
From the previous review, it is clear that laparoscopic colorectal surgery is superior to open surgery in terms of better short-term outcomes. However, the evidence for cost-effectiveness is less clear. There is a wide range of opinions regarding the cost-effectiveness of LCR for colorectal cancer. A recent systematic review of economic evaluations of RCTs comparing open and laparoscopic surgery showed that laparoscopic is slightly more expensive than open surgery [1]. However, the inclusion criteria were very restrictive, and hence, the study looked at a small portion of the currently available evidence on the cost gap between laparoscopic and open resections in colorectal surgery.
Aim
The aim of this study is to explore the cost-effectiveness of laparoscopic colorectal surgery over time since it was first developed in 1991.
Methods
In order to explore the reasons behind the inconsistency of results on the cost-effectiveness of laparoscopic colorectal surgery compared to open surgery, a systematic review of the literature was conducted. Electronic databases (PubMed, ScienceDirect and Google Scholar) were searched for studies from 1991 to September 2010. The search terms used were “laparoscopic, colorectal surgery cost, economic evaluation”. A review of economic evaluations was done by extracting data from studies that met the inclusion criteria below:
-
1.
Operations included colorectal cancers and not just benign disease.
-
2.
Studies had to compare, in terms of both direct costs (labour costs, equipment costs, theatre time, hospital stay and burden of complications) and clinical outcomes, laparoscopic with open surgery for treatment of colorectal cancer.
-
3.
Raw costs of both the laparoscopic and open intervention were stated clearly in the study. This was to allow the percentage difference between the two interventions to be calculated; this allowed further comparisons to be made across studies regardless of currencies and inflation rates.
Both randomised and nonrandomised studies were included. The total costs of the open and laparoscopic interventions were extracted from the economic evaluations, and the percentage cost difference between them was calculated.
Linear regression lines and correlation data were calculated in Excel. For correlation data, the Pearson product-moment correlation coefficient was used. Standard deviation from the average cost difference was used to identify subgroups in the studies.
Results
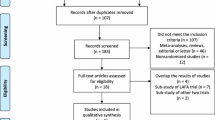
Out of the 289 search results, 15 economic evaluations met the inclusion criteria [7–21]. Studies by Ridgway et al. [22] and Bouvet et al. [23] performed relevant economic evaluations but did not include the price differences; therefore, they were excluded from the analysis (Fig. 1). Table 1 shows the studies that met the inclusion criteria and their results. Initial analysis of the data showed a discrepancy between the results from Asian & Western healthcare systems. Further analysis is shown in Table 2 to confirm this observation.
The percentage cost difference between open and laparoscopic surgery varied widely between different studies, as seen in the standard deviations in Table 2. Moreover, there was a variation in the cost differences in relation to the year the procedures were conducted (Fig. 2).
The general trend when observing all the included economic evaluations is that there is a moderate negative correlation between progression of time and the size of the cost gap between laparoscopic and open surgery (R-value = −0.44). This correlation is even stronger (R-value = −0.64) if the studies are subdivided by the country of origin where the surgery was carried out. This trend of decline costs over time reaches statistical significance (P = 0.046). Studies from Western healthcare systems, even though they had a heterogeneous set of results (SD = 27%), showed a decline in costs of laparoscopic surgery with time (Fig. 3). The overall price difference was small, with laparoscopic surgery being 5.6% more expensive than open surgery.
On the other hand, studies from Asian healthcare systems consistently (SD = 5.98%) had a higher price gap between open and laparoscopic surgery that very weakly correlated with progression of time (R-value = −0.20) (Fig. 4). There was no significant trend found in the cost over time (P = 0.152).
From the trends demonstrated in Figs. 1 and 2, it can be predicted that currently, laparoscopic surgery may be on average cheaper than open surgery. However, the correlation between time and cost gap is too weak in studies from Asian healthcare systems to be able to predict when laparoscopic colorectal surgery will be cheaper than open procedures (Fig. 4).
Discussion
These conflicting results may arise from lack of consensus concerning study methodology, differences between medical service systems in different nations and, especially, variations in the experience levels of surgeons [24]. The effects of these factors on the cost-effectiveness of laparoscopic surgery merits further discussion and studies.
The longer operative time required during the learning period of any surgical procedure may make it economically less attractive compared to older or simpler techniques. A study by Park et al. [20] extensively studied the cost-effectiveness of laparoscopic colorectal surgery compared to open surgery during the learning period. They discovered that the learning curve based on operative time flattens off at 37 cases of laparoscopic surgery. This also corresponded with the timing when laparoscopic surgery became a similar but still has more expensive cost than open surgery.
The overall trends seen in Figs. 1 and 2 may suggest that a global increase in laparoscopic colorectal experience may be increasing its cost-effectiveness. This may also explain the high average cost gap between laparoscopic and open resections in Asian healthcare systems which have just recently adopted laparoscopic techniques, and some of them could be still in the early part of the learning curve (Table 2).
Intraoperative difficulties may result in the conversion of a laparoscopic procedure to open surgery. The conversion rate is known to vary widely between studies: 7–25% in large series and 2–41% in smaller series [25]. Although conversion itself is not a complication, it is associated with a greater postoperative morbidity, which ultimately has been shown to reflect in greater costs incurred since the postoperative course of a conversion is associated with appreciably poorer results in terms of morbidity, mortality, convalescence, blood transfusion requirement and hospital stay [26]. Bouvet et al. [23] has shown that conversions are the single biggest factor that raises the price of laparoscopic surgery. Laparoscopic instrument manufacturers argue that if the conversion rates are reduced below 10%, laparoscopic colorectal surgery is more cost-effective than open surgery [27]. This may explain the cost effectiveness of laparoscopic colorectal surgery in large experienced centres as studies have shown that both the number of intraoperative laparoscopic complications and the conversion rate decreased with increasing experience [26].
Another factor that could explain the decline in the cost of laparoscopic surgery compared to open surgery is the improvement in the methodology of economic evaluations. More rigorous data collection, intention to treat analysis and indirect costs are features exclusive to some of the more recent economic evaluations [20, 21, 28].
The cost of laparoscopic instruments is one of the main components of the increased operating costs associated with laparoscopic colorectal surgery. Variation in the equipment used across different studies may account to the heterogeneity of the current evidence. For example, Ridgway et al. [22] calculated an extra 8% (Є12,000 over 35 cases) savings if nondisposable metal ports were used instead of the standard disposable ones.
From the currently available evidence, it has been shown by several studies [11, 22] that laparoscopic colorectal surgery can be cheaper than open surgery. However, the discrepancy in the results of the current economic evaluations means that the notion of laparoscopic colorectal surgery as standard across all healthcare systems should be taken with caution. Laparoscopic colorectal surgery has become more cost-effective over the years in studies from Western healthcare systems mainly due to the increased experience of surgeons; however, this change in cost effectiveness does not seem to be present in Asian healthcare systems despite comparable operating times and conversion rates [20]. This may indicate that core savings from laparoscopic colorectal surgery come from the reduced hospital stay which is significantly more expensive in Western healthcare systems.
Therefore, laparoscopic colorectal surgery could be routinely practised in Western healthcare systems by experienced surgeons in dedicated units. However, laparoscopic colorectal surgery may be cost-ineffective during the time spent in the learning phase. On the other hand, Asian healthcare systems should practise laparoscopic colorectal surgery if the short-term benefits of the surgery are deemed worth the extra costs laparoscopic surgery incurs.
Currently, only three economic evaluations have studied the indirect societal costs caused by colorectal surgery [11, 29, 30]. Since laparoscopic surgery is associated with faster return to normal activities, future studies should include indirect costs to avoid underestimating the savings of laparoscopic colorectal surgery.
The 15 economic evaluations reviewed in this report come from a wide variety of settings; therefore, care must be taken before generalising the results to the UK healthcare system. For example, this report included several studies from Asian countries where Choi et al. [21] reported that the hospital stay costs are relatively small compared to those of other countries. This may explain why laparoscopic colorectal surgery is still more expensive than open surgery in these areas since the imported equipment costs are far larger than local labour costs. Further research in UK teaching and district hospitals may be required to determine the exact setting where laparoscopic colorectal surgery can be feasibly be practised from an economic standpoint.
Randomised control trials are considered to be the top individual unit of research. They are believed to be the most reliable form of scientific evidence as they eliminate spurious causality and bias [31]; however, they are usually conducted under conditions that are different from normal clinical practice [32]. In the case of colorectal surgery, in routine clinical practice where laparoscopic colorectal surgery is well established, the surgeon chooses the intervention suitable for the patient based on several factors to minimise complications and to reduce the probability of a costly conversion. Therefore, randomised controlled trials studying colorectal surgery may have underestimated the true cost-effectiveness of laparoscopic surgery if patients at high risk of conversion were randomised to the laparoscopic group. Future economic evaluations should use the same conversion prediction models [33, 34] used in clinical practice to allocate patients into the laparoscopic or open intervention groups while adjusting for any confounding factors that may result from the removal of randomisation.
In Asian healthcare systems, operative costs overshadow the cost savings gained by reduced hospital stay. Therefore, LCS will remain more expensive in developing countries compared OCS until manufacturers can reduce intraoperative equipment cost. This might put patients in some countries at an underprivileged position regarding access to LCS.
Conclusion
From the current trends, it is projected that the results of future economic evaluations will unequivocally show that laparoscopic surgery is cheaper than open surgery for the majority of patients in Western healthcare systems. The laparoscopic approach to colorectal cancer may become the gold standard similar to laparoscopic cholescyctecomy. The initial higher costs of laparoscopic surgery training may be worth the savings made in the long term if it is practised in settings where postoperative care is expensive.
References
Hernández RA, de Verteuil RM, Fraser CM, Vale LD, Aberdeen Health Technology Assessment Group (2008) Systematic review of economic evaluations of laparoscopic surgery for colorectal cancer. Colorectal Dis 10(9):859–868
Bonjer HJ, Hop WC, Nelson H, Sargent DJ, Lacy AM, Castells A, Guillou PJ, Thorpe H, Brown J, Delgado S, Kuhrij E, Haglind E, Påhlman L, Transatlantic Laparoscopically Assisted vs Open Colectomy Trials Study Group (2007) Laparoscopically assisted vs open colectomy for colon cancer: a meta-analysis. Arch Surg 142(3):298–303
Chapman AE, Levitt MD, Hewett P, Woods R, Sheiner H, Maddern GJ (2001) Laparoscopic-assisted resection of colorectal malignancies. Ann Surg 234(5):590–606
Jacobs M, Verdeja JC, Goldstein HS (1991) Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc 1(3):144–150
Joo JS, Amarnath L, Wexner SD (1998) Is laparoscopic resection of colorectal polyps beneficial? Surg Endosc 12(11):1341–1344
Abraham NS, Young JM, Solomon MJ (2004) Meta-analysis of short-term outcomes after laparoscopic resection for colorectal cancer. Br J Surg 91(9):1111–1124
Saba AK, Kerlakian GM, Kasper GC, Hearn AT (1995) Laparoscopy assisted colectomies versus open colectomy. J Laparoendosc Surg 5(1):1–6
Pfeifer J, Wexner SD, Reissman P et al (1995) Laparoscopic vs open colon surgery: costs and outcome. Surg Endosc 9:1322–1326
Philipson BM, Bokey EL, Moore JW et al (1997) Cost of open versus laparoscopically assisted right hemicolectomy for cancer. World J Surg 21:214–217
Khalili TM, Fleshner PR, Hiatt JR et al (1998) Colorectal cancer: comparison of laparoscopic with open approaches. Dis Colon Rectum 41:832–838
Janson M, Björholt I, Carlsson P, Haglind E, Henriksson M, Lindholm E, Anderberg B (2004) Randomized clinical trial of the costs of open and laparoscopic surgery for colonic cancer. Br J Surg 91:409–417
Delaney CP, Kiran RP, Senagore AJ et al (2003) Case-matched comparison of clinical and financial outcome after laparoscopic or open colorectal surgery. Ann Surg 238:67–72
Shabbir A, Roslani AC, Wong KS, Tsang CB, Wong HB, Cheong WK (2009) Is laparoscopic colectomy as cost beneficial as open colectomy? ANZ J Surg 79(4):265–270
Leung KL, Kwok SP, Lam SC, Lee JF, Yiu RY, Ng SS et al (2004) Laparoscopic resection of rectosigmoid carcinoma: prospective randomised trial. Lancet 363:1187–1192
Zheng MH, Feng B, Lu AG et al (2005) Laparoscopic versus open right hemicolectomy with curative intent for colon carcinoma. World J Gastroenterol 11:323326
Braga M, Vignali A, Zuliani W et al (2005) Laparoscopic versus open colorectal surgery: cost-benefit analysis in a single-center randomized trial. Ann Surg 242:890–896
Senagore AJ et al (2005) Diagnosis related group assignment in laparoscopic and open colectomy: financial implications for payer and provider. Dis Colon Rectum 48:1016–1020
Franks (2006) unpublished data extracted from Murray A, Lourenco T, de Verteuil R, Hernandez R, Fraser C, McKinley A, Krukowski Z, Vale L, Grant A. (2006) Clinical effectiveness and cost-effectiveness of laparoscopic surgery for colorectal cancer: systematic reviews and economic evaluation. Health Technol Assess 10:1–141
King PM, Blazeby JM, Ewings P, Franks PJ, Longman RJ, Kendrick AH et al (2006) Randomized clinical trial comparing laparoscopic and open surgery for colorectal cancer within an enhanced recovery programme. Br J Surg 93:300–308
Park J et al (2007) Economics and the laparoscopic surgery learning curve: comparison with open surgery for rectosigmoid cancer. World J Surg 31:1827–1834
Choi YS et al (2007) Economic Outcomes of Laparoscopic Versus Open Surgery for Colorectal Cancer in Korea. Surg Today 37:127–132
Ridgway PF, Boyle E, Keane FB, Neary P (2007) Laparoscopic colectomy is cheaper than conventional open resection. Colorectal Dis 9(9):819–824
Bouvet M, Mansfield PF, Skibber JM, Curley SA, Ellis LM, Giacco GG, Madary AR, Ota DM, Feig BW (1998) Clinical, pathologic, and economic parameters of laparoscopic colon resection for cancer. Am J Surg 176(6):554–558
Bennett CL, Stryker SJ, Ferreira MR, Adams J, Beart RW Jr (1977) The learning curve for laparoscopic colorectal surgery: preliminary results from a prospective analysis of 1194 laparoscopic-assisted colectomies. Arch Surg 132(1):41–44
Gervaz P, Pikarsky A, Utech M, Secic M, Efron J, Belin B, Jain A, Wexner S (2001) Converted laparoscopic colorectal surgery. Surg Endosc 15(8):827–832
Marusch F, Gastinger I, Schneider C, Scheidbach H, Konradt J, Bruch HP, Köhler L, Bärlehner E, Köckerling F, Laparoscopic Colorectal Surgery Study Group (LCSSG) (2001) Importance of conversion for results obtained with laparoscopic colorectal surgery. Dis Colon Rectum 44(2):207–214
NICE. Colorectal cancer—laparoscopic surgery (review). Available at: http://www.nice.org.uk/TA105 [Accessed December 20, 2010]
Faiz O, Warusavitarne J, Bottle A, Tekkis PP, Darzi AW, Kennedy RH (2009) Laparoscopically assisted vs. open elective colonic and rectal resection: a comparison of outcomes in English National Health Service Trusts between 1996 and 2006. Dis Colon Rectum 52(10):1695–1704
King PM et al (2006) Randomized clinical trial comparing laparoscopic and open surgery for colorectal cancer within an enhanced recovery programme. Br J Surg 93:300–308
Franks. Unpublished data extracted from Murray A, Lourenco T, de Verteuil R, Hernandez R, Fraser C, McKinley A, Krukowski Z, Vale L, Grant A. (2006) Clinical effectiveness and cost-effectiveness of laparoscopic surgery for colorectal cancer: systematic reviews and economic evaluation. Health Technol Assess 10:1–141
Lachin JM, Matts JP, Wei LJ (1988) Randomization in clinical trials: conclusions and recommendations. Control Clin Trials 9(4):365–374
Naylor CD (1995) Grey zones of clinical practice: some limits to evidence-based medicine. Lancet 345(8953):840–842
Tekkis PP, Senagore AJ, Delaney CP (2005) Conversion rates in laparoscopic colorectal surgery: a predictive model with, 1253 patients. Surg Endosc 19(1):47–54
Rotholtz NA, Laporte M, Zanoni G, Bun ME, Aued L, Lencinas S, Mezzadri NA, Pereyra L (2008) Predictive factors for conversion in laparoscopic colorectal surgery. Tech Coloproctol 12(1):27–31
Author information
Authors and Affiliations
Corresponding author
Additional information
This paper was presented as a Poster in the ESCP Meeting in 2010 in Sorrento, Italy. This was published as an abstract in Colorectal Disease 2010, 12 (Suppl. 3): p5.
Rights and permissions
About this article
Cite this article
Aly, O.E., Quayyum, Z. Has laparoscopic colorectal surgery become more cost-effective over time?. Int J Colorectal Dis 27, 855–860 (2012). https://doi.org/10.1007/s00384-012-1410-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-012-1410-1