Abstract
Background
Low serum albumin was found as a predictor of long-term mortality in colorectal cancer (CRC) patients. Our aim was to evaluate the value of the pretreatment albumin/globulin ratio (AGR) to predict the long-term mortality in CRC patients.
Methods
Patients were included if they had comprehensive metabolic panel (CMP) before treatment (surgery or chemotherapy). The albumin/globulin ratio, routinely reported in CMP, is calculated [AGR = Albumin/(Total protein − Albumin)]. Patients were divided into three equal tertiles according to their pretreatment AGR. The primary outcome was cancer-related mortality, which was obtained from our cancer registry database.
Results
A total of 534 consecutive CRC patients had pretreatment CMP. The 1st AGR tertile had a significant higher 4-year mortality compared to the second and third AGR tertiles (42 vs. 19 and 7 %, p < 0.0001 according to Fisher’s exact two-tailed test). In the multivariate model, AGR remained an independent predictor of survival with 75 % decrease in mortality among the highest AGR tertile in comparison to the lowest AGR tertile, p < 0.0001. In the subset of 234 patients with normal serum albumin (albumin of >3.5 g/dl), serum AGR continues to be an independent predictor of cancer-related mortality with an adjusted hazard ratio of the third tertile compared to the first tertile equal to 0.05 (95 % confidence interval 0.01–0.33, p = 0.002).
Conclusion
Low AGR was a strong independent predictor of long-term cancer-specific survival among colorectal cancer patients. Additionally, among the patients with normal albumin (>3.5 g/dl), patients with lower globulins but higher albumin and AGR levels had better survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the third leading cause of cancer deaths in USA [1]. Multiple prognostic indicators such as tumor extent, node status, lymphovascular invasion, residual tumor, and tumor grade have been identified as predictors of outcomes following the surgical treatment of the CRC [2–6]. Additionally, markers of inflammation such as neutrophils, lymphocytes, monocytes, platelets, C-reactive proteins (CRP) had been previously studied in cancers and were found to have a prognostic value [7–9]. It has been demonstrated that the proinflammatory chemokines and cytokines in the tumor microenvironment aid in tumor progression, invasion, metastasis, subversion of adaptive immunity, and reduced response to hormones and chemotherapeutic agents, thus affecting survival [10].
Albumin and globulins, the two major constituents of serum proteins, play a pivotal role in the inflammatory process. Immunoglobulins and other acute-phase proteins such as CRP, serum amyloid A, complement C3, fibrinogen, and ceruloplasmin, which are part of the calculated globulins play a crucial role in immunity and inflammation cascades [11, 12]. Hence, we speculated that the increased level of globulins serves as a marker of chronic inflammation and reflects a cumulative exposure of various proinflammatory cytokines. Moreover, hypoalbuminemia is not only a mere marker of low nutritional status but also associated with chronic inflammation [13]. Low albumin in cancer patient can be the result of cytokine-induced suppression [14] or increased degradation as shown in sarcoma-bearing mice models [15]. Prior studies have identified the negative impact of hypoalbuminemia on survival in CRC patients [16, 17]. However, none of the previous studies looked into the effects of both albumin and globulin on CRC patients. The purpose of this study is to assess the effect of albumin to globulin ratio on CRC survival.
Methods
This is a retrospective, longitudinal, cohort study of unselected consecutive 651 patients diagnosed with CRC at a tertiary cancer care center between 2005 and 2011. The patients were included in the cohort if they had comprehensive metabolic panel (CMP) before their initial treatment modality (i.e., surgery or chemotherapy). Exclusion criteria were as follows: patients who had preexisting liver disease, on immunosuppressive therapy including recent steroid exposure, or with chronic inflammatory disease including autoimmune disorder and infection; those who received preoperative chemotherapy; and those presented with bowel obstruction. Out of the 651 patients, a total of 534 patients matched the inclusion and exclusion criteria. The data regarding patient’s demographic characteristics, comorbidities, tumor pathology and stage, treatment modalities, and laboratory variables were collected from the hospital’s database using electronic medical record (EMR) software. The American Joint Committee on Cancer (AJCC) staging system was used to stage the tumor in each subject. Cardiopulmonary disease included any history of congestive heart failure, ischemic heart disease, chronic lung disease, or cerebrovascular disease. Serum chemistries were determined by Beckman coulter (Synchron® System, Anaheim, CA). The total protein level was measured through a reaction between cupric ions in an alkaline solution with proteins and polypeptides containing at least two peptide bonds to produce a violet-colored complex. The combination between albumin and bromocresol purple reagent to form a colored complex product was the basis of albumin measurement in this study. The albumin/globulin ratio (AGR) was calculated [AGR = Albumin/(Total protein − Albumin)]. The primary end point of the study was the cancer-related survival. The data on mortality were taken from the cancer registry, EMR, and Social Security Death Index. The study design and protocol were approved by our institutional review board.
Statistical analysis
Patients were divided into equal tertiles according to the 33rd and 66th AGR percentile (that is the third or highest AGR tertile, including the patient with the uppermost 33 % AGR values). Accordingly, the AGR tertiles were AGR first tertile of <1.028, AGR second tertile of 1.028–1.321, and AGR third tertile of >1.321, and albumin tertiles were albumin first tertile of ≤3.1 g/dl, albumin second tertile of 3.1–3.7 g/dl, and albumin third tertile of >3.7 g/dl. Continuous variables are presented as means and standard deviations, and categorical variables are presented as frequencies and percentages. For group comparisons, chi-square and two-tailed Fisher’s exact tests were used for categorical variables, and analysis of variance and Kruskal–Wallis tests were used for continuous variables (depending on the distribution of the continuous variables). The study was powered to evaluate the 4-year mortality rate with an estimate of 7 % difference in mortality among the three AGR tertiles (68, 75, and 82 %). A minimum of 153 patients in each AGR tertile was required to detect the aforementioned estimated difference in mortality with 80 % power and <5 % type 1 error. A univariate screen of all potential predictors of mortality using the Cox proportional hazard model for each variable was performed. Those variables that were clinically and statistically significant in the univariate analysis were included in multivariate Cox regression models. In the multivariate models, the nonsignificant variables were removed by backward selection. Albumin and globulin were excluded as they were used in the calculation of AGR. Statistical analysis was performed using the SPSS version 19.0 (SPSS A, Inc., Chicago, IL, USA). A result was considered statistically significant with p value of <0.05.
Results
Baseline characteristics
The average age of the patients was 69 years, 53 % females, 88 % whites, and 15 % had previous history of cancers. Most of the patients had grade 2 histology (67 %), followed by grades 3 and 1 (25.88 and 6.63 %, respectively). Also, the AJCC staging among patients was distributed as 25, 31, 26, and 18 % for stages 1, 2, 3, and 4, respectively. The patients in the lowest AGR tertile were significantly older with higher rates of female gender and advanced cancer stages compared to the higher AGR tertiles. Additionally, the lowest AGR tertile had significantly lower rates of treatments with surgery and chemotherapy. Moreover, those patients in the lowest AGR tertile had significantly higher proinflammatory hematological parameters (leukocyte, neutrophil, platelet counts) compared to those in the higher AGR tertiles (Table 1).
Primary outcome according to AGR and albumin tertiles
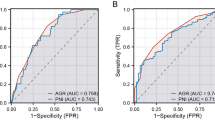
During the follow-up period of 4 years (an average and median follow-up period = 40 months), 120/534 = 22 % patients died. When the groups were divided by AGR tertiles, the lowest AGR tertile had a 4-year mortality rate of 41.6 % as opposed to 18.54 and 7.3 % in the middle and the highest AGR tertiles, p < 0.0001. According to the albumin tertiles, the lowest albumin tertile had a higher 4-year mortality rate of 38 % as opposed to 26 and 5 % in the middle and the highest albumin tertiles, p < 0.0001 (Fig. 1). Likewise, Kaplan–Meier curves showed significant lower 4-year all-cause mortality rates in the third AGR and albumin tertiles in comparison to the first AGR and albumin tertiles (Fig. 2).
The 4-year cancer-related mortality among the colorectal cancer patients, according to their pretreatment serum albumin and AGR, albumin, and AGR with normal albumin. AGR albumin/globulin ratio. Mortality rates across AGR tertiles had chi-square value of 62.4 and p < 0.0001, while across albumin tertiles, rates were 60 and <0.0001, respectively
Univariate screening of predictors of mortality
The results of the univariate analysis, using the individual Cox regressions, showed that age, cardiac or pulmonary disease, grade 3 tumors, increase AJCC stages, and lymph node involvement were all associated with an increase in mortality as expected. Also, lower lymphocyte and elevated leukocyte and neutrophil counts were associated with an increase in mortality. In terms of treatment, only surgical intervention was associated with a statistically significant decrease in mortality. The hazard ratio of each unit increase of serum albumin was 0.34 [confidence interval (CI) 0.27–0.42, p < 0.001], while the hazard ratio of AGR was 0.06 (CI 0.03–0.11, p < 0.001). Similarly, the lowest AGR and albumin tertiles had worse survival compared to the higher AGR and albumin tertiles, respectively (Table 2).
Multivariate analysis of predictors of mortality
Using the multivariate analysis, for each unit increase in the serum albumin, the 4-year mortality decreased by 0.51(CI 0.38–0.67, p < 0.001), and for each unit increase in AGR, the 4-year mortality decreased by 0.17 (CI 0.09–0.34, p < 0.001). Likewise, using the albumin and AGR tertiles, the hazard ratios of the second and third AGR tertiles were 0.52 (CI 0.34–0.80, p = 0.003) and 0.25 (CI 0.13–0.49, p < 0.001) compared to the first AGR tertile (Table 3). Similarly, the second and third albumin tertiles had better survival compared to the first (lowest) albumin tertile [HR 0.73 (CI 0.47–1.14, p = 0.167) and 0.22 (CI 0.11–0.46, p < 0.001), respectively] (Table 3).
Additional analyses
Further subsets analyses were conducted to determine if the above association between AGR and mortality was merely secondary to the hypoalbuminemia or early mortality. After excluding patients with hypoalbuminemia (defined as albumin of ≤3.5 g/dl), 234 patients were analyzed. Among these patients with normal albumin concentrations, patients who had the lowest albumin and the highest globulins tertiles had significantly higher mortality (from the lowest to the highest tertiles, the 4-year mortality rates were as follows: 14.5, 4.2, and 3.4 % for albumin tertiles with p value = 0.022; 2.3, 5.7, and 14.5 % for globulins tertiles with p value = 0.0068; and 14.8, 6.7, and 0 % for AGR tertiles with p value = 0.0003) (Fig. 3). Moreover, in this subset of 234 patients with normal serum albumin, serum AGR continues to remain an independent predictor of overall survival with an adjusted hazard ratio of the third tertile compared to the first tertile equal to 0.05 (95 % CI 0.01–0.33, p = 0.002).
The 4-year cancer-related mortality among colorectal cancer patients with normal serum albumin according to their pretreatment serum albumin, globulin, and albumin/globulin ratio (AGR). The p values, regarding the difference in mortality between the highest and lowest tertiles, were calculated according to two-tailed Fisher’s exact test
In the second additional analysis of the subset of patients that survived beyond 6 months of baseline AGR measurement (467 patients), the lowest AGR tertile had a significantly higher mortality in comparison to the higher AGR tertiles (16.9 vs. 6.6 vs. 5.4 %, p = 0.012) (Fig. 4).
The 4-year cancer-related mortality according to the pretreatment albumin/globulin ratio (AGR) among colorectal cancer patients who survived 6 months after diagnosis. There was a significant difference in mortality between the highest and lowest AGR tertiles, p = 0.021, according to two-tailed Fisher’s exact test
Discussion
Our main finding is that the low pretreatment AGR is a significant predictor of mortality in CRC patients. As observed, patients with low AGR were older and had advanced cancer stages, but after controlling for these confounding variables, low AGR remained an independent predictor of mortality. Further, the negative impact of low AGR was also observed in patients with normal serum albumin (patients with albumin of >3.5 g/dl). The predictive value of low AGR was not solely explained by the higher short-term mortality, as low AGR remains a significant predictor of mortality in the patients who survived beyond 6 months of their diagnosis and baseline AGR measurement.
Low albumin as a predictor of poor survival in CRC
Prior studies demonstrated that the low pretreatment albumin levels had unfavorable prognosis in CRC patients [19–22]. While our study corroborates with prior studies that low albumin is a negative predictor in CRC, we also observed the association of hypoalbuminemia, low AGR, and high inflammatory hematological parameters (WBC, neutrophil, and neutrophil/lymphocyte ratio). According to prior studies, the association of low albumin and systemic inflammatory response was attributed to the upregulation of many proinflammatory cytokines and growth factors (e.g., IL-1β, IL-6, and TNF) that modulate the albumin production by liver cells among cancer patients [13, 18]. Similarly, among hemodialysis patients, the low albumin was attributed to inflammatory status rather than malnutrition [23, 24]. Moreover, an inflammation-based score [Glasgow prognostic score (GPS)], which is derived from CRP and albumin, has been shown preoperatively to predict survival after resection of CRC [17, 22]. Additional studies demonstrated the antiproliferative effect of albumin on human cancer cells [25, 26]. Interestingly, in our study, we have found that higher albumin concentration was associated with better survival even in patients with normal albumin concentration.
Elevated non-albumin proteins (“calculated globulins”) as a predictor of poor survival in CRC
In the comprehensive metabolic panel, the calculated globulins (Total protein − Albumin) include most of the proinflammatory proteins (complement components, CRP, immunoglobulins, interleukins, TNF). Also, tumor markers (e.g., CA 19-9 and CEA) are considered in the calculated globulins as they have peptide bonds that react with cupric ions. Several studies have demonstrated the prognostic value of the non-albumin proinflammatory proteins in cancer patients. Cohen et al. demonstrated that low albumin and high alpha and gamma globulins were associated with poor survival in lung cancer patients [27]. Likewise, Cazador et al. demonstrated the negative impact of high complement 3 and pre- and postoperative IgA levels in CRC patients [28]. Further, higher complement (C3 and C4) levels were also found in lung cancer patients compared to the control group [29]. High levels of serum CRP correlate with decreased survival in patients with gastrointestinal malignancies [30–32]. Interestingly, in a genome-wide association study (n = 10,000), Osman et al. found a strong association between common variants of tumor necrosis factor receptor superfamily member 13B (TNFRSF13B) and other genes with elevated serum non-albumin protein and immunoglobulins [33].
In our study, we observed that patients with elevated globulins had poor survival compared to those with low globulin. This finding was observed also in patients with normal serum albumin, which suggest that the elevated globulin is not a mere compensation to hypoalbuminemia.
In a prior study of 80 cancer patients, Al-Joudi found that patients with low globulin represented as low globulin compensation index [GCI = (Globulin in gram per liter − 25)/(35 − Albumin in gram per liter)] had poor prognosis. In this study, the negative GCI (i.e., low globulin) was found in 46 % of the deceased group and 27 % survivors. The study’s conclusion was that patients who failed to compensate for the low albumin had a poor outcome [34].
The contradictory conclusion of this study led us to analyze our subset of patient with low albumin and calculate their GCI. Out of the 269 patients with albumin of <3.5 g/dl, we found that 60 patients had a negative GCI. In this subset of patients with hypoalbuminemia, we found that 24 % survivors and 19 % deceased had a negative GCI (p = 0.44), which is contrary to the above study. However, in spite of a larger sample size in our study, the results were not statistically significant, and further studies to explore the predictive value of GCI may be needed.
Potential superiority of AGR to albumin as a predictor of survival in CRC
We advocate for the use of AGR rather than albumin to predict survival in CRC for two reasons. The AGR, being a ratio and not just absolute value like albumin, is less vulnerable to the measurement variability (i.e., false elevated and reduced albumin values in dehydration and fluid retention states, respectively). Additionally, low AGR reflects two negative predictors in the form of a ratio (i.e., low albumin and high non-albumin proteins “globulins”). This endorses the value of previously reported GPS that also used albumin and non-albumin protein (CRP) in their calculation. Low AGR was associated with poor survival in breast cancer patients and was found as a predictor of adverse cardiovascular outcomes.
Interestingly, a genome-wide association study (n = 8,842 population) identified multiple signals associated with AGR. In this study, the most compelling association of AGR was with two loci, the TNFRSF13B locus on chromosome 17p11.2 and the FADS1 locus on chromosome 11q12.2. The TNFRSF13B encodes for tumor necrosis factor receptor superfamily, which activates several transcription factors that plays a major role in inflammation [35].
Limitations
This study is retrospective and is single center based. Including other nutritional and inflammatory markers (like prealbumin, CRP, and cytokine) may have strengthened the study.
Conclusion
Pretreatment low AGR is an independent predictor of poor survival in CRC patients even among those with normal albumin. Additionally, among the patients with normal albumin (>3.5 g/dl), patients with higher albumin levels had better survival. Interestingly, elevated non-albumin proteins (calculated globulins) were also associated with poor long-term survival in patients with normal albumin concentrations. Further studies are needed to validate this finding and to investigate the mechanism of low AGR in CRC patients.
References
American Cancer Society (2011) Colorectal cancer facts & figures 2011–2013. American Cancer Society, Atlanta
Betge J, Pollheimer MJ, Lindtner RA et al (2012) Intramural and extramural vascular invasion in colorectal cancer: prognostic significance and quality of pathology reporting. Cancer 118(3):628–638
Gunderson LL, Jessup JM, Sargent DJ, Greene FL, Stewart AK (2010) Revised TN categorization for colon cancer based on national survival outcomes data. J Clin Oncol 28(2):264–271
Huh JW, Kim HR, Kim YJ (2010) Lymphovascular or perineural invasion may predict lymph node metastasis in patients with T1 and T2 colorectal cancer. J Gastrointest Surg 14(7):1074–1080
Swanson RS, Compton CC, Stewart AK, Bland KI (2003) The prognosis of T3N0 colon cancer is dependent on the number of lymph nodes examined. Ann Surg Oncol 10(1):65–71
Wohlke M, Schiffmann L, Prall F (2011) Aggressive colorectal carcinoma phenotypes of invasion can be assessed reproducibly and effectively predict poor survival: interobserver study and multivariate survival analysis of a prospectively collected series of 299 patients after potentially curative resections with long-term follow-up. Histopathology 59(5):857–866
Toiyama Y, Miki C, Inoue Y, Tanaka K, Mohri Y, Kusunoki M (2011) Evaluation of an inflammation-based prognostic score for the identification of patients requiring postoperative adjuvant chemotherapy for stage II colorectal cancer. Exp Ther Med 2(1):95–101
Roxburgh CS, McMillan DC (2010) Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol 6(1):149–163
Inoue Y, Iwata T, Okugawa Y et al (2013) Prognostic significance of a systemic inflammatory response in patients undergoing multimodality therapy for advanced colorectal cancer. Oncology 84(2):100–107
Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A (2009) Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis 30(7):1073–1081
McPherson R, Pincus MR (2011) Henry’s clinical diagnosis and management by laboratory methods, 22nd edn. Saunders, Philadelphia
Gabay C, Kushner I (1999) Acute-phase proteins and other systemic responses to inflammation. N Engl J Med 340(6):448–454
McMillan DC, Watson WS, O’Gorman P, Preston T, Scott HR, McArdle CS (2001) Albumin concentrations are primarily determined by the body cell mass and the systemic inflammatory response in cancer patients with weight loss. Nutr Cancer 39(2):210–213
Fearon KC, Falconer JS, Slater C, McMillan DC, Ross JA, Preston T (1998) Albumin synthesis rates are not decreased in hypoalbuminemic cachectic cancer patients with an ongoing acute-phase protein response. Ann Surg 227(2):249–254
Andersson C, Lonnroth C, Moldawer LL, Ternell M, Lundholm K (1990) Increased degradation of albumin in cancer is not due to conformational or chemical modifications in the albumin molecule. J Surg Res 49(1):23–29
Lai CC, You JF, Yeh CY et al (2011) Low preoperative serum albumin in colon cancer: a risk factor for poor outcome. Int J Color Dis 26(4):473–481
McMillan DC, Crozier JE, Canna K, Angerson WJ, McArdle CS (2007) Evaluation of an inflammation-based prognostic score (GPS) in patients undergoing resection for colon and rectal cancer. Int J Color Dis 22(8):881–886
Gupta D, Lis CG (2010) Pretreatment serum albumin as a predictor of cancer survival: a systematic review of the epidemiological literature. Nutr J 9:69
Cengiz O, Kocer B, Surmeli S, Santicky MJ, Soran A (2006) Are pretreatment serum albumin and cholesterol levels prognostic tools in patients with colorectal carcinoma? Med Sci Monit 12(6):CR240–CR247
Dixon MR, Haukoos JS, Udani SM et al (2003) Carcinoembryonic antigen and albumin predict survival in patients with advanced colon and rectal cancer. Arch Surg 138(9):962–966
Heys SD, Walker LG, Deehan DJ, Eremin OE (1998) Serum albumin: a prognostic indicator in patients with colorectal cancer. J R Coll Surg Edinb 43(3):163–168
Ishizuka M, Nagata H, Takagi K, Horie T, Kubota K (2007) Inflammation-based prognostic score is a novel predictor of postoperative outcome in patients with colorectal cancer. Ann Surg 246(6):1047–1051
Kaysen GA (2001) The microinflammatory state in uremia: causes and potential consequences. J Am Soc Nephrol: JASN 12(7):1549–1557
Kaysen GA (2003) Serum albumin concentration in dialysis patients: why does it remain resistant to therapy? Kidney Int Suppl 87:S92–S98
Sonnenschein C, Soto AM, Michaelson CL (1996) Human serum albumin shares the properties of estrocolyone-I, the inhibitor of the proliferation of estrogen-target cells. J Steroid Biochem Mol Biol 59(2):147–154
Laursen I, Briand P, Lykkesfeldt AE (1990) Serum albumin as a modulator on growth of the human breast cancer cell line, MCF-7. Anticancer Res 10(2A):343–351
Cohen MH, Makuch R, Johnston-Early A et al (1981) Laboratory parameters as an alternative to performance status in prognostic stratification of patients with small cell lung cancer. Cancer Treat Rep 65(3–4):187–195
Codina Cazador A, Salva Lacombe JA, Fernandez-Llamazares Rodriguez J, Ruiz Feliu B, Codina Barreras A, Moreno Aguado V (1989) Immunoglobulins and the complement system in colorectal cancer. Rev Esp Enferm Apar Dig 75(2):143–148
Oner F, Savas I, Numanoglu N (2004) Immunoglobulins and complement components in patients with lung cancer. Tuberk Toraks 52(1):19–23
Shimada H, Nabeya Y, Okazumi S et al (2003) Elevation of preoperative serum C-reactive protein level is related to poor prognosis in esophageal squamous cell carcinoma. J Surg Oncol 83(4):248–252
Gerhardt T, Milz S, Schepke M et al (2006) C-reactive protein is a prognostic indicator in patients with perihilar cholangiocarcinoma. World J Gastroenterol 12(34):5495–5500
Canna K, McArdle PA, McMillan DC et al (2005) The relationship between tumour T-lymphocyte infiltration, the systemic inflammatory response and survival in patients undergoing curative resection for colorectal cancer. Br J Cancer 92(4):651–654
Osman W, Okada Y, Kamatani Y, Kubo M, Matsuda K, Nakamura Y (2012) Association of common variants in TNFRSF13B, TNFSF13, and ANXA3 with serum levels of non-albumin protein and immunoglobulin isotypes in Japanese. PLoS One 7(4):e32683
Al-Joudi FS (2005) Prognostic value of an index for serum globulin compensation in colon and breast cancers. Singap Med J 46(12):710–713
Hong KW, Jin HS, Song D, Kwak HK, Soo Kim S, Kim Y (2013) Genome-wide association study of serum albumin:globulin ratio in Korean populations. J Hum Genet 58(3):174–177
Conflict of interest
The authors report no potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Azab, B., Kedia, S., Shah, N. et al. The value of the pretreatment albumin/globulin ratio in predicting the long-term survival in colorectal cancer. Int J Colorectal Dis 28, 1629–1636 (2013). https://doi.org/10.1007/s00384-013-1748-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-013-1748-z