Abstract
Objective
The number of colon cancer patients is increasing worldwide. Malnutrition and comorbidities are frequently associated with these patients. The relationships between the preoperative malnutrition and the outcomes of colon cancer patients are unclear; this study aimed to clarify these issues.
Methods
A total of 3,849 consecutive colon cancer patients were enrolled in an analysis of short-term outcomes and 2,529 patients were included in an analysis of the long-term outcomes. These patients were divided into the hypoalbuminemic and normal groups according to the definition of hypoalbuminemia (serum albumin < 35 g/L).
Results
Advanced age, female gender, abnormal CEA levels, right colon or large tumors, mucinous adenocarcinoma, poor differentiation, stage II cancer, TNM advancing T stage, old cardiovascular accident, diabetes, and liver cirrhosis were more likely to be associated with hypoalbuminemia. Hypoalbuminemic patients had a higher rate of postoperative mortality and morbidity, including complications related to wounds, lungs, the urinary system, and anastomosis. The 5-year overall survival rates of patients with normal albumin and hypoalbuminemia were 78.0% and 60.0%, respectively (P < 0.0001), and the 5-year relapse-free survival rates were 78.9% and 73.5%, respectively (P = 0.0042). In a multivariate analysis, the albumin level was also significantly correlated with 5-year overall survival (<35 vs. ≥35, HR 1.75; 95% CI 1.49–2.08) and 5-year relapse-free survival (<35 vs. ≥35, HR 1.28; 95% CI 1.04–1.56).
Conclusions
Hypoalbuminemia is a predictor of poor surgical outcomes of colon cancer and is a poor prognosis factor for long-term survival of colon cancer after curative operation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The number of cases of colon cancer is increasing in Taiwan and in other developed countries; the number of colectomies performed is also increasing. Malnutrition is a commonly encountered problem when treating colon cancer patients. Serum albumin is closely correlated with the degree of malnutrition and is a regularly used, simple marker of nutrition status [1, 2]. According to some previous studies, patients with hypoalbuminemia who underwent gastrointestinal tract surgery have significantly higher postoperative morbidity and mortality [3, 4]; however, some other studies report no significant differences [5, 6]. Hypoalbuminemia has also been used as a predictor of the survival of colorectal cancer patients [7–11], although the results are controversial.
Hypoalbuminemia in cancer patients does not only result from the cancer itself, but may also result from associated comorbidities [12, 13]. Furthermore, some comorbidities influence postoperative mortality and morbidity [13–16], as well as the survival of cancer patients [16–18]. There is little information concerning the relationships between hypoalbuminemia, comorbidities, and the outcomes of colon cancer patients. Therefore, this study aimed to clarify these relationships and determine if preoperative hypoalbuminemia might be useful for predicting the postoperative mortality, morbidity, and prognosis of colon cancer patients after receiving an elective and curative surgery.
Patients and methods
From January 1995 to December 2008 inclusive, a total of 3,849 consecutive patients with colon cancer underwent elective and potentially curative surgery at Chang Gung Memorial Hospital. Excluding 117 patients without preoperative serum albumin data (3.0% of colon cancer patients in our hospital), the remaining 3,732 patients were included in the analysis of short-term outcomes in this study. A total of 2,529 patients who received surgery more than 5 years ago and survived for more than 30 days after surgery were included in the analysis of long-term outcomes.
Detailed information regarding patient- and tumor-related variables and follow-up statuses was retrieved from the Colorectal Section Tumor Registry at Chang Gung Memorial Hospital. All data in this registry were collected prospectively. Patient demographic data, tumor characteristics, operative details, and short- and long-term postoperative outcomes were included in the data collection.
Patient-related variables consisted of age, gender, serum albumin level, CEA level, and comorbidities. The patients were divided into two age groups: ≤65 years (young) and >65 years (old). Hypoalbuminemia was defined as serum albumin < 35 g/L. CEA levels > 5 ng/ml were defined as abnormal. The following comorbidities were recorded: hypertension, cardiac disease, old cardiovascular accident (CVA), asthma, diabetes, hepatitis, liver cirrhosis, thyroid disease, and other comorbidities, such as peptic ulcer disease, urolithiasis, and gall stones.
Tumor-related factors consisted of location, size, morphology, histology, degree of differentiation, and stage. Tumor stages were determined according to the AJCC TNM staging system (sixth edition)[19]. Tumor location was categorized as right colon (from the cecum to transverse colon) or left colon (from the splenic flexure to sigmoid colon). Tumor morphology was divided into polypoid (include flat and polypoid tumors) and nonpolypoid (include ulcerative and infiltrative tumors).
According to the definition of hypoalbuminemia, patients were divided into two groups: hypoalbuminemic or normal. Each patient underwent standard oncological resection of colonic tumors and received routine postoperative care.
The short-term outcomes of surgery include postoperative morbidity and mortality. Postoperative morbidities were defined as complications within 30 days of the primary surgery and classified as wounds (infection or dehiscence), and pulmonary (atelectasis or pneumonia), cardiovascular (myocardial infarction, stroke, or embolism), urinary (bladder dysfunction or urinary tract infection), gastrointestinal (obstruction, ileus, or bleeding), anastomotic (leakage, stenosis, abscess formation, or peritonitis), and other conditions. Postoperative mortality was defined as death within 30 days of the primary surgery.
The endpoints of the long-term outcome study were overall survival (OS) and relapse-free survival (RFS). OS was calculated by death from any cause, and RFS was calculated by considering any relapses from the index cancer as the only events for survival analyses. Relapses of cancer were confirmed histologically or radiographically.
Statistical methods
Quantitative data were compared using Pearson’s chi-squared and Fisher’s exact tests. For multivariate analysis, logistic regression analysis was used to determine any confounding factors of mortality and morbidity; variables where P < 0.05 in the univariate analyses were used in the multivariate analysis. OS and RFS were calculated by univariate analysis using the Kaplan–Meier method. Survival curves were constructed using the Kaplan–Meier method and were compared using the log-rank test. In order to control for confounding factors, the Cox regression model was used for multivariate analysis in which variables for which P < 0.05 in the log-rank analyses were used. All P values were two-tailed, and were considered statistically significant if <0.05.
Results
The clinicopathologic characteristics of the patients categorized by serum albumin data are presented in Table 1. The mean ages (standard deviation) of patients in short- and long-term outcome analyses were 63.14 years (13.58) and 62.47 years (13.59), respectively. The proportion of hypoalbuminemia in stage I, II, and III colon cancer patients with elective surgery was 18.6%.
In short-term outcome analysis, there were no significant differences in tumor morphology and N stage of the TNM system between the normal and hypoalbuminemic groups. Advanced age, females, abnormal CEA levels, right colon tumors, large tumors (tumor size > 5 cm), mucinous adenocarcinoma, poor differentiation, stage II cancer, and advancing T stage of the TNM system were more likely to be associated with hypoalbuminemia. Similar results were found in the long-term outcome analysis—except there was no significant difference related to gender.
The comorbidities of patients in the two groups are presented in Table 2. There was no significant difference with respect to associated medical diseases between the two groups (52.9% and 56.4% of normal and hypoalbuminemic patients, respectively; P = 0.098). There was no significant difference in the occurrence of hypertension, cardiac disease, asthma, hepatitis, and thyroid disease between the two groups. However, CVA (P < 0.001), diabetes (P < 0.001), liver cirrhosis (P < 0.001), other comorbidities (P < 0.001), and combined comorbidities (P < 0.001) were significantly more likely to be associated with hypoalbuminemia.
Short-term outcomes
The analysis of postoperative morbidity and mortality in both groups is presented in Table 3. The postoperative mortality rate was 1.2% (45 of 3,732), and the morbidity rate was 11.7% (436 of 3732). Compared to patients with normal serum albumin, hypoalbuminemic patients have a higher rate of postoperative morbidity and mortality, as well as complications related to wounds, lungs, urinary system, and anastomosis. There was no significant difference between the two groups with regard to complications of the cardiovascular or gastrointestinal systems. In these variables, hypoalbuminemia was the only significant factor related to anastomostic complications. In multivariate analysis, TNM stage, age, sex, each category of comorbidity, CEA level, tumor location, tumor morphology, tumor size, histologic type and grade were taken into analysis if it is significant factor in univariate analysis.
Hypoalbuminemia was an independent factor for postoperative mortality, morbidity, and complications related to wounds, lungs, and the urinary system (Tables 4 and 5). Advanced age, males, asthma, and hypoalbuminemia were significantly associated with morbidity. Advanced age, diabetes, liver cirrhosis, abnormal CEA level, and hypoalbuminemia were significantly associated with mortality. Old CVA and hypoalbuminemia were significantly associated with complications related to wounds. Advanced age, abnormal CEA level, hypoalbuminemia, nonpolypoid tumor, and poorly differentiated tumors were significantly associated with complications of the lungs. Advanced age and hypoalbuminemia were significantly associated with complications of the urinary system. Males, asthma, mucinous adenocarcinoma, and TNM stage II cancer were significantly associated with complications of the gastrointestinal system.
Long-term outcomes
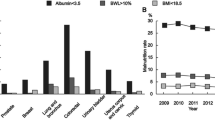
For the 2,529 patients who underwent curative surgery between January 1995 and December 2004 and survived more than 30 days after the operation, the 5-year OS and RFS rates were 74.6% and 77.9%, respectively. When stratified by preoperative serum albumin levels, the 5-year OS rates of patients with normal albumin and hypoalbuminemia were 78.0% and 60.0%, respectively (P < 0.0001), and the 5-year RFS rates were 78.9% and 73.5%, respectively (P = 0.0042). Hypoalbuminemic patients had significantly poorer OS (Fig. 1) and RFS rates (Fig. 2) compared to patients with normal serum albumin.
In a univariate analysis of OS and RFS rates, the following factors were examined: TNM stage, age, sex, each category of comorbidity, CEA level, occurrence of morbidity, tumor location, morphology, size, histologic type, and grade. TNM stage (P < 0.0001), age (P < 0.0001), sex (P = 0.0466), hypertension (P = 0.0028), cardiac disease (P = 0.0336), old CVA (P < 0.0001), diabetes (P < 0.0001), liver cirrhosis (P = 0.0097), other medical diseases (P = 0.0012), CEA level (P < 0.0001), occurrence of morbidity (P < 0.0001), tumor morphology (P = 0.0003), histologic type (P = 0.0024), and histologic grade (P = 0.0019) were significant predictors of OS. TNM stage (P < 0.0001), hypertension (P = 0.0236), cardiac disease (P = 0.0366), CEA level (P < 0.0001), tumor morphology (P < 0.0001), histologic type (P = 0.0001), and histologic grade (P < 0.0001) were significant predictors of RFS.
For multivariate analysis, the significant predictors from univariate analysis were introduced into the Cox regression model; the results are shown in Table 6 (OS) and Table 7 (RFS). For the OS rate, the remaining significant predictors were TNM stage (stage III vs. I—HR 2.11, 95% CI 1.57–2.83), age (>65 vs. ≤65—HR 1.92, 95% CI 1.65–2.23), sex (male vs. female—HR 1.16, 95% CI 1.01–1.33), old CVA (yes vs. no—HR 1.76, 95% CI 1.32–2.36), diabetes (yes vs. no—HR 1.23, 95% CI 1.01–1.49), CEA level (≥5 vs <5—HR 1.64, 95% CI 1.42–1.89), albumin level (<35 vs. ≥35—HR 1.75, 95% CI 1.49–2.08), and histologic type (signet-ring cell vs. adenocarcinoma—HR 2.26, 95% CI 1.16–4.38). For the RFS, the remaining significant predictors were TNM stage (stage II vs. I—HR 1.81, 95% CI 1.11–2.96; stage III vs. I—HR 4.21, 95% CI 2.59–6.85), CEA level (≥5 vs. <5—HR 2.04, 95% CI 1.72–2.43), albumin level (<35 vs. ≥35—HR 1.28, 95% CI 1.04–1.56), tumor morphology (nonpolypoid vs. polypoid—HR 1.53, 95% CI 1.20–1.96), and histologic type (signet-ring cell vs. adenocarcinoma—HR 2.53, 95% CI 1.27–5.06).
In both the uni- and multivariate analyses, hypoalbuminemia was a significant predictor of poorer OS and RFS.
Discussion
Malnutrition is a common problem that debilitates cancer patients—including those with colon cancer [12, 20, 21]. Malnutrition in colon cancer patients may result from higher metabolism rates induced by cancer, reduction of food intake, impairment of hepatic protein synthesis, or blood loss, etc. [12, 20, 21]. Although it cannot comprehensively represent the nutritional status of patients [12], serum albumin level is extensively used. Hypoalbuminemia is widely accepted to be a good indicator of malnutrition [1–4, 22]. In the present study, 18.6% of colon cancer patients were hypoalbuminemic. In reality, the proportion of hypoalbuminemic colon cancer patients may be higher than in the present study because stage IV patients were excluded.
The association between hypoalbuminemia and adverse outcomes of elective [23], cardiac [24], and gastrointestinal surgery [3, 4, 25] has been known for many years. However, hypoalbuminemia is not an independent condition of surgical patients; certain types of diseases and characteristics of colon cancer patients also contribute to hypoalbuminemic status [12, 13]. However, previous studies have not explored the association of hypoalbuminemia with conditions such as diseases related to old CVA, diabetes mellitus, or liver cirrhosis, as well as cancer patient characteristics of advanced age, males, right side colon cancer, tumor size, depth of tumor invasion, mucinous type, poor differentiation, and abnormal CEA revealing in this study. These kinds of diseases and characteristics of colon cancer patients were also associated with adverse surgical outcomes; different factors may be associated with different postoperative complications. The confounding influences of hypoalbuminemia, characteristics of colon cancer patients, and diseases on surgical outcomes are seldom discussed in previous studies—the present study aimed to elucidate these issues. The results of this study show that hypoalbuminemia is an independent risk factor for postoperative mortality, morbidity, as well as complications related to wounds, lungs, the urinary system, and anastomosis, but not the gastrointestinal system or other complications. Although some previous studies suggest that hypoalbuminemia is significantly associated with postoperative ileus [26], this can be neither proved nor disproved by this study since postoperative ileus was not isolated from complications of the gastrointestinal system. The results of this study show that other kinds of adverse outcomes are associated with certain organ diseases. Old CVA patients are significantly associated with postoperative complications of wounds. Asthma patients have higher rate of complications of gastrointestinal system. Diabetes mellitus was a risk factor of postoperative mortality.
It is still controversial whether preoperative hypoalbuminemia influences the long-term outcomes of colon cancer patients. Some studies report that by itself, hypoalbuminemia is not an independent factor of survival [9, 10]. However, in conjunction with other factors, such as CRP [9] and CEA [10], they can significantly alter survival rates. Few studies report that hypoalbuminemia is an independent factor for poor survival [7, 11]. However, the analyses used in past survival studies have included overall, disease-free, cancer-specific, and relapse-free survival rates; the results of survival studies vary according to the definition of survival used. It has previously been reported that non-surgical patients with hypoalbuminemia exhibit poor long-term survival [27, 28]. It is reasonable to suggest that hypoalbuminemic colon cancer patients have poor long-term survival rates because they tend to be older and exhibit comorbidities. Whether preoperative hypoalbuminemia influences the further metastasis of colon cancer is not known. In this study, both overall and relapse-free survival rates—representing the possibility of further metastasis—were analyzed. The results revealed that by itself, preoperative hypoalbuminemia in colon cancer patients is an independent factor for poor long-term outcomes, including overall and relapse-free survival—this holds true even according to multivariate analysis, which included the variances in patient and cancer characteristics, and comorbidities. That is to say, colon cancer patients with preoperative hypoalbuminemia have poorer postoperative OS rates and a higher possibility of further cancer metastasis.
Although hypoalbuminemia is a well-known predictor of poor surgical outcomes, pre- or perioperative administration of albumin does not decrease the occurrence of complications [6, 12, 29, 30]. Recent studies revealed that pre- or perioperative nutritional supplements may improve surgical outcomes [31–33]. Whether the administration of albumin or nutritional supplements can improve long-term outcomes or diminish further metastasis remains unknown; further studies are needed.
Conclusion
Hypoalbuminemia is a predictor of poor surgical outcomes of colon cancer patients. It is also a poor prognosis factor for long-term survival of colon cancer patients after curative operation.
References
Bauer J, Capra S (2003) Comparison of a malnutrition screening tool with subjective global assessment in hospitalised patients with cancer–sensitivity and specificity. Asia Pac J Clin Nutr 12(3):257–260
Fuhrman MP, Charney P, Mueller CM (2004) Hepatic proteins and nutrition assessment. J Am Diet Assoc 104(8):1258–1264
Buzby GP, Mullen JL, Matthews DC, Hobbs CL, Rosato EF (1980) Prognostic nutritional index in gastrointestinal surgery. Am J Surg 139(1):160–167
Detsky AS, Baker JP, O’Rourke K, Johnston N, Whitwell J, Mendelson RA et al (1987) Predicting nutrition-associated complications for patients undergoing gastrointestinal surgery. JPEN J Parenter Enteral Nutr 11(5):440–446
Ryan JA, Taft DH (1980) Preoperative nutritional assessment does not predict morbidity and mortality in abdominal operations. Surg Forum 31:96–98
Nilsson E, Lamke LO, Liljedahl SO, Elfstrom K (1980) Is albumin therapy worthwhile in surgery for colorectal cancer? Acta Chir Scand 146(8):619–622
Heys SD, Walker LG, Deehan DJ, Eremin OE (1998) Serum albumin: a prognostic indicator in patients with colorectal cancer. J R Coll Surg Edinb 43(3):163–168
Crozier JE, Leitch EF, McKee RF, Anderson JH, Horgan PG, McMillan DC (2009) Relationship between emergency presentation, systemic inflammatory response, and cancer-specific survival in patients undergoing potentially curative surgery for colon cancer. Am J Surg 197(4):544–549
McMillan DC, Crozier JE, Canna K, Angerson WJ, McArdle CS (2007) Evaluation of an inflammation-based prognostic score (GPS) in patients undergoing resection for colon and rectal cancer. Int J Colorectal Dis 22(8):881–886
Boonpipattanapong T, Chewatanakornkul S (2006) Preoperative carcinoembryonic antigen and albumin in predicting survival in patients with colon and rectal carcinomas. J Clin Gastroenterol 40(7):592–595
Cengiz O, Kocer B, Surmeli S, Santicky MJ, Soran A (2006) Are pretreatment serum albumin and cholesterol levels prognostic tools in patients with colorectal carcinoma? Med Sci Monit 12(6):CR240–CR247
Franch-Arcas G (2001) The meaning of hypoalbuminaemia in clinical practice. Clin Nutr 20(3):265–269
Alves A, Panis Y, Mathieu P, Mantion G, Kwiatkowski F, Slim K (2005) Postoperative mortality and morbidity in French patients undergoing colorectal surgery: results of a prospective multicenter study. Arch Surg 140(3):278–283
Longo WE, Virgo KS, Johnson FE, Oprian CA, Vernava AM, Wade TP et al (2000) Risk factors for morbidity and mortality after colectomy for colon cancer. Dis Colon Rectum 43(1):83–91
Ondrula DP, Nelson RL, Prasad ML, Coyle BW, Abcarian H (1992) Multifactorial index of preoperative risk factors in colon resections. Dis Colon Rectum 35(2):117–122
Janssen-Heijnen ML, Maas HA, Houterman S, Lemmens VE, Rutten HJ, Coebergh JW (2007) Comorbidity in older surgical cancer patients: influence on patient care and outcome. Eur J Cancer 43(15):2179–2193
Iversen LH, Norgaard M, Jacobsen J, Laurberg S, Sorensen HT (2009) The impact of comorbidity on survival of Danish colorectal cancer patients from 1995 to 2006—a population-based cohort study. Dis Colon Rectum 52(1):71–78
Sarfati D, Hill S, Blakely T, Robson B, Purdie G, Dennett E et al (2009) The effect of comorbidity on the use of adjuvant chemotherapy and survival from colon cancer: a retrospective cohort study. BMC Cancer 9:116
AJCC (2002) AJCC cancer staging manual, 6th edn. Springer, New York
Lohsiriwat V, Lohsiriwat D, Boonnuch W, Chinswangwatanakul V, Akaraviputh T, Lert-Akayamanee N (2008) Pre-operative hypoalbuminemia is a major risk factor for postoperative complications following rectal cancer surgery. World J Gastroenterol 14(8):1248–1251
Van Cutsem E, Arends J (2005) The causes and consequences of cancer-associated malnutrition. Eur J Oncol Nurs 9(Suppl 2):S51–S63
Sungurtekin H, Sungurtekin U, Balci C, Zencir M, Erdem E (2004) The influence of nutritional status on complications after major intraabdominal surgery. J Am Coll Nutr 23(3):227–232
Mullen JL, Buzby GP, Waldman MT, Gertner MH, Hobbs CL, Rosato EF (1979) Prediction of operative morbidity and mortality by preoperative nutritional assessment. Surg Forum 30:80–82
Rich MW, Keller AJ, Schechtman KB, Marshall WG Jr, Kouchoukos NT (1989) Increased complications and prolonged hospital stay in elderly cardiac surgical patients with low serum albumin. Am J Cardiol 63(11):714–718
Gibbs J, Cull W, Henderson W, Daley J, Hur K, Khuri SF (1999) Preoperative serum albumin level as a predictor of operative mortality and morbidity: results from the National VA Surgical Risk Study. Arch Surg 134(1):36–42
Lohsiriwat V, Chinswangwatanakul V, Lohsiriwat S, Akaraviputh T, Boonnuch W, Methasade A et al (2007) Hypoalbuminemia is a predictor of delayed postoperative bowel function and poor surgical outcomes in right-sided colon cancer patients. Asia Pac J Clin Nutr 16(2):213–217
Phillips A, Shaper AG, Whincup PH (1989) Association between serum albumin and mortality from cardiovascular disease, cancer, and other causes. Lancet 2(8677):1434–1436
Harvey KB, Moldawer LL, Bistrian BR, Blackburn GL (1981) Biological measures for the formulation of a hospital prognostic index. Am J Clin Nutr 34(10):2013–2022
Rothschild MA, Oratz M, Schreiber SS (1988) Serum albumin. Hepatology 8(2):385–401
Yuan XY, Zhang CH, He YL, Yuan YX, Cai SR, Luo NX et al (2008) Is albumin administration beneficial in early stage of postoperative hypoalbuminemia following gastrointestinal surgery?: a prospective randomized controlled trial. Am J Surg 196(5):751–755
Mullen JL, Buzby GP, Matthews DC, Smale BF, Rosato EF (1980) Reduction of operative morbidity and mortality by combined preoperative and postoperative nutritional support. Ann Surg 192(5):604–613
Grimes CJ, Younathan MT, Lee WC (1987) The effect of preoperative total parenteral nutrition on surgery outcomes. J Am Diet Assoc 87(9):1202–1206
Moskovitz DN, Kim YI (2004) Does perioperative immunonutrition reduce postoperative complications in patients with gastrointestinal cancer undergoing operations? Nutr Rev 62(11):443–447
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lai, CC., You, JF., Yeh, CY. et al. Low preoperative serum albumin in colon cancer: a risk factor for poor outcome. Int J Colorectal Dis 26, 473–481 (2011). https://doi.org/10.1007/s00384-010-1113-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-010-1113-4