Abstract
Purpose
Our aims were to evaluate protein tyrosine phosphatase nonreceptor type 22 (PTPN22) gene polymorphisms in ulcerative colitis (UC) and explore PTPN22 mRNA levels in colonic biopsies of UC patients in central China.
Methods
A total of 165 Chinese UC patients and 300 healthy controls were enrolled in this study. PTPN22 −1123G/C, +1858C/T, and +788G/A polymorphisms were genotyped by PCR-restriction fragment length polymorphism method. PTPN22 mRNA expressions in colonic biopsies and serum C-reactive protein (CRP) levels were determined by quantitative PCR and immunonephelometry, respectively.
Results
The frequency of C carrier was higher in UC patients than in healthy controls (66.7 vs. 53.3 %, P = 0.005, odds ratios = 1.75, 95 % CI 1.18–2.60) and associated with extensive colitis (P = 0.029). PTPN22 mRNA levels were elevated in UC patients than in healthy controls (P < 0.001). Among UC patients, PTPN22 mRNA expression levels were higher in biopsies of inflamed colonic tissue compared with noninflamed tissue (P < 0.001) and were correlated with CRP levels (r = 0.578, P < 0.001). PTPN22 mRNA expression levels were elevated in extensive colitis compared to proctitis (P = 0.008) and to left-sided colitis (P = 0.029) and were higher in moderate and severe disease than in mild disease (P = 0.005).
Conclusions
Our study showed the potential association between PTPN22 −1123G/C polymorphism and UC in central China. PTPN22 mRNA levels were highly expressed in UC, especially in active disease, and were correlated with CRP levels, disease location, and disease severity in UC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammatory bowel disease (IBD) is a chronic, relapsing intestinal inflammatory disorder and is commonly classified into ulcerative colitis (UC) and Crohn’s disease (CD). Current studies suggest that this disease results from the complex interaction of genetic, immune, and environmental factors [1]. UC has been considered as a typical model of disease as a result of an exaggerated T-cell response [1]. The gene protein tyrosine phosphatase nonreceptor type 22 (PTPN22) encodes the gatekeeper of T-cell receptor (TCR) signaling, cytoplasmic lymphoid tyrosine phosphatase (LYP), and as such is a likely candidate risk factor for UC because of its role in down-regulation of T-cell activation [2].
In T cells, LYP is a potent negative regulator of TCR signaling through dephosphorylation of several key mediators of TCR signal transduction, including the Src family kinases Lck and Fyn, as well as ZAP-70 and TCRzeta [3, 4]. These studies also suggest that inhibition of LYP might be beneficial in autoimmunity. Several academic laboratories have begun developing small molecule inhibitors of LYP [5, 6]. If confirmed by further validation data, this will make LYP as a possible drug target for autoimmunity. Mutation of PTPN22 gene may influence T-cell activation and induce autoimmune diseases such as type 1 diabetes, autoimmune thyroid disease, and rheumatoid arthritis [7].
Numerous studies provide evidence that the PTPN22 gene is involved in human susceptibility to autoimmune diseases [2, 7, 8]. Several single nucleotide polymorphisms have been associated with type 1 diabetes, rheumatoid arthritis, systemic lupus erythematosus, IBD, and other autoimmune diseases; however, some of these associations have not been confirmed, and there are even some contradictory data in different populations [9–11]. Specifically, the +1858C/T (R620W) has been the most investigated PTPN22 polymorphism in autoimmunity diseases, and the allele frequencies vary remarkably among the different populations [7]. The R620W variation disrupts the interaction between Lck and LYP, leading to reduced phosphorylation of LYP, which ultimately contributes to gain-of-function inhibition of T-cell activation [3]. Inspiringly, Kawasaki et al. [12] carried out a systemic research on PTPN22 gene by direct sequencing in the Japanese population and found that the mutation of PTPN22 gene associated with type 1 diabetes is not +1858C/T but −1123G/C. Recently, the polymorphism of −1123G/C, located in the promoter region of the PTPN22 gene, was shown to be correlated with rheumatoid arthritis and type 1 diabetes in Chinese population [13–15]. The newly described polymorphism, +788G/A in exon 10 of PTPN22 gene, within the catalytic domain of the enzyme, was found to be associated with UC [11] and was a loss-of-function mutation that confers protection against development of rheumatoid arthritis and systemic lupus erythematosus [16, 17].
Despite the promising role of the PTPN22 gene, there are very few studies that have assessed its role in UC patients; it is not clear whether the −1123G/C mutation or another variant somewhere else within the PTPN22 gene is associated with UC in Chinese population. Therefore, in this study, we performed a detailed genotype–phenotype analysis of the polymorphism of −1123G/C, +1858C/T, and +788G/A in PTPN22 gene in a cohort of UC patients and healthy controls in central China and investigated PTPN22 mRNA expression levels in colonic biopsies and serum levels of C-reactive protein (CRP) in patients with UC.
Materials and methods
Subjects
A total of 165 unrelated Chinese patients with UC of Han ethnicity were collected from The Central Hospital of Wuhan in central China in this study. The diagnosis was based on conventional clinical, radiological, endoscopic, and histological criteria [18]. The location of disease was defined according to the Montreal classification (ulcerative proctitis, left-sided colitis, and extensive colitis) [19]. The severity of UC was determined according to Truelove and Witts criteria (mild colitis, moderate colitis, and severe colitis) [20]. We combined moderate and severe colitis since there were only nine patients in the severe group. A total of 57 of 165 UC patients were randomly selected for PTPN22 mRNA expression analysis. Demographic characteristics and clinical features of the patients with UC are shown in Table 1. We also analyzed PTPN22 mRNA expression levels in 25 patients with other form of colitis (OFCs). The OFC group consisted of patients with non-IBD gastrointestinal inflammation, including infectious colitis, ischemic colitis, and colitis related to diverticular disease.
A total of 300 age- and sex-matched healthy controls were selected from the medical staff of The Central Hospital of Wuhan, as well as from healthy volunteers in the same geographic area of Wuhan City. The healthy controls were ethnically matched and had no symptoms suggestive of chronic bowel disease and no personal or family history of UC. In all, 11 of 300 healthy controls were randomly selected for PTPN22 mRNA analysis. Informed consent was taken from all study subjects. The study protocol was approved by the ethics committees of The Central Hospital of Wuhan.
DNA isolation
A blood sample was obtained from each case and healthy control and was used for DNA extraction. Genomic DNA was isolated from 5 ml EDTA anticoagulated venous blood according to the standard protocol of the QiAamp DNA Blood Midi kit (Qiagen, Hilden, Germany). The quality of DNA samples was checked by measuring the A 260/280 ratio using a NanoDrop2000C spectrophotometer (Thermo, Asheville, NC, USA). The ratio fell between 1.8 and 2.0 for all samples.
PTPN22 genotyping
The −1123G/C, +1858C/T, and +788G/A polymorphisms in PTPN22 gene were determined by PCR-restriction fragment length polymorphism (PCR-RFLP) analysis.
For genotyping of the −1123G/C (rs2488457) variant in PTPN22 gene, PCR was performed to detect −1123G/C polymorphism by using forward primer 5′-CCA TTG AGA GGT TAT GCG AGC T-3′ and reverse primer 5′-CGC CAC CTT GCT GAC AAC AT-3′ [14]. PCR was performed as follows: initial denaturation at 95 °C for 5 min, followed by 35 cycles of 95 °C for 40 s, 58 °C for 40 s, and 72 °C for 40 s, and final extension at 72 °C for 5 min. The PCR product of −1123G/C variant was digested at 37 °C for 3 h with SacI restriction enzyme (Fermentas, Burlington, ON, Canada). DNA fragments were then separated by electrophoresis on 2.5 % agarose gel and were stained with ethidium bromide. The product after digestion with SacI was 323 bp fragment representing a C/C genotype, two fragments of 298 and 25 bp representing a G/G genotype, and three fragments of 323, 298, and 25 bp representing a G/C genotype.
For genotyping of the +1858C/T (rs2476601) variant in PTPN22 gene, PCR was performed to detect +1858C/T polymorphism by using forward primer 5′-ACC CAT TGA GAG GTT ATG CGA GCT-3′ and reverse primer 5′-TAG AAA GCC TGA AGA ACT G-3′ [13]. PCR was performed as follows: initial denaturation at 95 °C for 5 min, followed by 35 cycles of 95 °C for 40 s, 53 °C for 40 s, and 72 °C for 40 s, and final extension at 72 °C for 5 min. The PCR product of +1858C/T variant was digested at 37 °C for 3 h with RsaI restriction enzyme (Fermentas). DNA fragments were then separated by electrophoresis on 2.5 % agarose gel and were stained with ethidium bromide. The product after digestion with RsaI was 252 bp fragment representing a T/T genotype, two fragments of 217 and 35 bp representing a C/C genotype, and three fragments of 252, 217, and 35 bp representing a T/C genotype.
For genotyping of the +788G/A (rs33996649) variant in PTPN22 gene, PCR was performed to detect +788G/A polymorphism by using forward primer 5′-GAT GGA GCA AGA CTC AGA CAC-3′ and reverse primer 5′-CCC CAT GTT AGA AGA GCA GAT-3′ [14]. PCR was performed as follows: initial denaturation at 95 °C for 5 min, followed by 35 cycles of 95 °C for 40 s, 53 °C for 40 s, and 72 °C for 40 s, and final extension at 72 °C for 5 min. The PCR product of +788G/A variant was digested at 37 °C for 3 h with MspI restriction enzyme (Fermentas). DNA fragments were then separated by electrophoresis on 2.5 % agarose gel and were stained with ethidium bromide. The product after digestion with MspI was 234 bp fragment representing an A/A genotype, two fragments of 91 and 143 bp representing a G/G genotype, and three fragments of 234, 91, and 143 bp representing a G/A genotype.
For quality control purposes of genotyping, all experiments were repeated twice, and positive and negative controls were processed with each batch of samples to ensure accuracy. Positive controls consisted of randomly chosen samples (20 %), as determined by direct DNA sequencing using an ABI 3730 apparatus (Applied Biosystems, Foster City, CA, USA).
Colonic biopsies
Biopsies were taken from patients with UC and patients with non-IBD controls undergoing diagnostic colonoscopy and from healthy controls undergoing screening colonoscopy for colorectal cancer after written informed consent. Four biopsies were collected from each UC patient: two from macroscopically noninflamed sites and two from macroscopically inflamed mucosa. Two biopsies from macroscopically inflamed mucosa were collected from non-IBD controls. Two biopsies from macroscopically noninflamed mucosa were collected from healthy controls. PTPN22 mRNA expression levels were measured in each individual biopsy.
RNA extraction and complimentary DNA (cDNA) synthesis
Total RNA was extracted from fresh colonic biopsies of UC patients, non-IBD controls, and healthy controls, with Trizol reagent according to the manufacturer’s instruction (Invitrogen, Carlsbad, CA, USA). A total of 1 μg of RNA was reverse-transcribed into cDNA using a First Strand cDNA Synthesis Kit (Fermentas).
Quantitative PCR of PTPN22 mRNA
Expression levels of PTPN22 mRNA in colonic biopsies were detected by quantitative PCR analysis with a Rotor-Gene 3000 system (Corbett Research, Concorde, NSW, Australia) using the Quantitect SYBR Green PCR Kit (Takara, Shiga, Japan) following the manufacturer’s guidelines, employing the β-actin gene as a reference gene. The following primer pairs were used [21]: PTPN22—forward 5′-TGC CCA CCA AAC AAG CC-3′ and reverse 5′-TGG TGG TGG ATT CCT TGG-3′; β-actin—forward 5′-AGC CAT GTA CGT TGC TAT-3′ and reverse 5′-CTT AAT GTC ACG CAC GAT TT-3′. PCR conditions were as follows: an initial denaturation at 95 °C for 10 min, followed by 45 cycles of 95 °C for 20 s, 56 °C for 20 s, and 72 °C for 20 s, and final extension at 72 °C for 10 min. The relative changes in gene expression were quantified using comparative CT methods [22, 23].
Determination of serum levels of CRP
A blood sample from each patient and the healthy control was collected in serum separator tubes and was then centrifuged for 15 min at 1,000×g, right after a 30-min clotting period had elapsed. All serum samples were stored at −80 °C until assayed. Serum CRP measurements were performed by immunonephelometry [24] with the Behring Nephelometer Analyzer II (BNII) using the N High Sensitivity kit (Dade Behring, Marburg, Germany) according to manufacturer’s instructions. Each sample was tested in triplicate.
Statistical analysis
The statistical analysis was done by SPSS 13.0 software (SPSS Inc., Chicago, USA). The comparisons of the genotype and allelic frequencies were performed using the chi-square (χ 2) test with Yates’ correction or Fisher’s exact test. Odds ratios (OR) and 95 % confidence intervals (CI) were calculated for the disease in carriers of the specific alleles. Continuous variables were reported as means ± standard deviation (SD), and statistical comparisons were performed with the two-tailed Student’s t test and one-way ANOVA analysis. The correlation coefficients between variables were examined by nonparametric correlation (Spearman r). A P value < 0.05 was considered statistically significant.
Results
Distribution of PTPN22 allele and genotype frequencies in patients with UC and in healthy controls
In all subjects, genotype distributions were in Hardy–Weinberg equilibrium for the −1123G/C polymorphisms (P = 0.645 in UC and 0.057 in controls). The sex ratio and distribution of age did not differ between UC patients and healthy controls (P = 0.592 and P = 0.849, respectively).
The distribution of allele and genotype frequencies of −1123G/C, +1858C/T, and +788G/A in PTPN22 gene in patients with UC and in healthy controls is shown in Table 2. The prevalence of the GC genotype tended to be higher in UC patients than in controls, reaching a significant difference (50.3 vs. 39.7 %, P = 0.027, OR = 1.54, 95 % CI 1.05–2.26). When combining the GC and CC genotypes, the frequency of C carrier was higher in UC patients than in controls (66.7 vs. 53.3 %, P = 0.005, OR = 1.75, 95 % CI 1.18–2.60). Similarly, the frequency of the C allele was increased in UC patients when compared with the controls (41.5 vs. 33.5 %, P = 0.015, OR = 1.41, 95 % CI 1.07–1.86). The distribution of +1858C/T and +788G/A allele and genotype frequencies did not differ between UC patients and the healthy controls.
Association of −1123G/C polymorphism in PTPN22 gene with disease characteristics in UC patients
The association between −1123G/C polymorphism and disease characteristics of UC patients is shown in Table 3. There were no associations between −1123G/C polymorphism and some disease characteristics such as gender, age, extraintestinal manifestation as well as “drug therapy,” but there was a higher incidence of extensive colitis in C carrier of −1123G/C compared to GG genotype in UC patients (34.5 vs. 18.2 %, P = 0.029, OR = 2.38, 95 % CI 1.08–5.23).
PTPN22 mRNA levels were elevated in active UC patients
As illustrated in Fig. 1, PTPN22 mRNA expression levels were increased in biopsies of inflamed colonic tissue from UC patients (n = 43) compared with that of healthy controls (n = 11) (P < 0.001) and with biopsies of inflamed colonic tissue from non-IBD controls (n = 25) (P < 0.001). Among UC patients, PTPN22 mRNA expression levels were higher in biopsies of inflamed colonic tissue (n = 43) compared with noninflamed tissue (n = 14) (P < 0.001). There was no difference in the PTPN22 mRNA expression levels between noninflamed tissue of UC patients and colonic biopsies of healthy controls (P = 0.271). PTPN22 mRNA expression levels did not differ between inflamed tissue of non-IBD controls and colonic biopsies of healthy controls (P = 0.081).
Relative expression levels of PTPN22 mRNA in biopsies of inflamed and noninflamed colonic tissue from UC patients, biopsies of inflamed colonic tissue from non-IBD controls and colonic biopsies from healthy controls (HC), utilizing arbitrary units. PTPN22 mRNA expression levels were normalized to the expression in healthy controls in which PTPN22 mRNA expression levels were set arbitrary as 1.0. Data are expressed as means ± SD. c vs. b, P < 0.05; c vs. a, P < 0.05; b vs. a, P = NS; c vs. g, P < 0.05; a vs. g, P = NS; b vs. g, P = NS. NS not significant
PTPN22 mRNA levels were positively correlated with CRP levels in UC patients
Patients with active UC had statistically significant higher CRP levels compared to patients with inactive disease [(14.54 ± 3.46) vs. (2.97 ± 0.97) mg/l, P = 0.005]. PTPN22 mRNA expression levels in colonic biopsies were positively and significantly correlated with serum CRP levels (r = 0.578, P < 0.001) in UC patients.
Association of PTPN22 mRNA levels with clinical features of UC patients
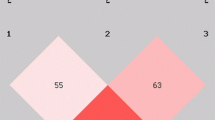
PTPN22 mRNA expression levels in colonic biopsies in patients with UC were analyzed after stratification by the location, extraintestinal manifestation, severity, and −1123G/C polymorphism. The location of disease seemed to affect PTPN22 mRNA expression levels in UC patients. PTPN22 mRNA expression levels were elevated in extensive colitis (n = 13) compared to proctitis (n = 12; P = 0.008) and to left-sided colitis (n = 18; P = 0.029) (Fig. 2). Extraintestinal manifestation was another parameter analyzed and revealed no affection on PTPN22 mRNA expression levels (P = 0.692).
Relative expression levels of PTPN22 mRNA in colonic biopsies in patients with UC after stratification by disease location, utilizing arbitrary units. PTPN22 mRNA expression levels were normalized to the expression in proctitis in which PTPN22 mRNA expression levels were set arbitrary as 1.0. Data are expressed as means ± SD. f vs. d, P < 0.05; f vs. e, P < 0.05; e vs. d, P = NS. NS not significant
Concerning disease severity, PTPN22 mRNA expression levels were influenced by disease severity, exhibiting higher values in moderate and severe disease (n = 27) than in mild disease (n = 16) (Fig. 3, P = 0.005). The PTPN22 mRNA expression levels in subgroups of C carrier of −1123G/C were higher than those in GG genotype, but the differences between PTPN22 mRNA expression levels among them did not reach statistical significance (P = 0.273).
Relative expression levels of PTPN22 mRNA in colonic biopsies in patients with UC after stratification by disease severity, utilizing arbitrary units. PTPN22 mRNA expression levels were normalized to the expression in mild colitis in which PTPN22 mRNA expression levels were set arbitrary as 1.0. Data are expressed as means ± SD
Discussion
This study provides evidence for the association between the −1123G/C polymorphism in PTPN22 gene and UC in the Han Chinese in central China. We found that the frequencies of C allele and C carrier of −1123G/C were significantly higher in UC patients than in healthy controls. Moreover, genotype–phenotype analysis showed that the C carrier of −1123G/C was associated with extensive colitis in UC patients. Our results suggested that the C carrier of −1123G/C may be predictors for extensive colitis among UC patients, and PTPN22 −1123G/C polymorphism was likely to have some effect on disease extent during the course of the disease.
No other studies in the Chinese population on the −1123G/C polymorphism in relation to UC have been published thus far to compare our data; however, a study done in a Chinese population of rheumatoid arthritis patients showed similar results: Feng et al. [15] found that the frequency of the C allele of −1123G/C was significantly increased in patients with rheumatoid arthritis than in healthy controls. Compared with the controls, patients with type 1 diabetes had a significantly higher frequency of the GC genotype of −1123G/C in PTPN22 gene in a Chinese population [13]. The study in Japanese and Korean populations indicated that the −1123G/C but not +1858C/T polymorphism correlates with type 1 diabetes [12]. It has been suggested that the C carrier of −1123G/C polymorphism was associated with rheumatoid arthritis in a Norwegian population [25]. In a recent meta-analysis [26], the polymorphism of the PTPN22 gene rs6679677 associated with an increased risk for Crohn’s disease showed significant protective effects in ulcerative colitis in European ancestry. This discrepancy might be explained by ethnicity, disease specificity, or gene–environment interactions present in populations from central China but not in Europe. These studies and our results indicated a phenomenon that the association of PTPN22 −1123G/C polymorphism with autoimmune diseases may be ubiquitous in the Asian population.
In our study, we observed that the polymorphisms of +1858C/T and +788G/A in PTPN22 gene are almost absent in the Chinese population. It has been suggested that the +1858C/T has been the most investigated PTPN22 polymorphism in relation to autoimmunity diseases in the Caucasian population, whereas it is lacking in Asian or other populations [7, 27]. Diaz-Gallo et al. showed that PTPN22 +788G/A polymorphism was associated with UC in Spanish Caucasian population, but not in Dutch and New Zealand population [11]. This discrepancy might be explained by racial difference.
The current study found that PTPN22 mRNA levels in biopsies of colonic tissue were increased in UC patients and were positively correlated with CRP levels. Among UC patients, PTPN22 mRNA levels were higher in biopsies of inflamed colonic tissue than in noninflamed tissue. Our findings corroborate those of Ronninger et al. [28] in rheumatoid arthritis. It showed that PTPN22 mRNA levels were increased in rheumatoid arthritis than in healthy controls. Chang et al. [21] found that the relative amounts of PTPN22 mRNA and protein expression levels were both increased in human Jurkat T cells after stimulated with anti-CD3. Possible mechanisms producing high levels of PTPN22 mRNA in UC could be (1) the majority of patients with UC might produce high levels of PTPN22 mRNA under certain conditions, for example the increase of antigen-specific activated T cells [29], and (2) PTPN22 mRNA levels may correlate with the immunologic states and complex genetic control.
Furthermore, we evaluated the possible relationship of PTPN22 mRNA levels in biopsies of colonic tissue with clinical features of UC patients. Our findings showed that the increase of PTPN22 mRNA levels in UC patients was rather unaffected from extraintestinal manifestation, but there was a significant association of PTPN22 mRNA levels in biopsies with disease location and severity among the UC patients. PTPN22 mRNA levels were found significantly elevated in UC patients with extensive colitis, in comparison with proctitis and left-sided colitis, and PTPN22 mRNA levels were increased in moderate and severe diseases than in mild disease. As extensive and severe colitis is considered a more severe phenotype with higher rates of dysplasia and colectomy or colorectal cancer, this finding was likely to provide additional support for the PTPN22 mRNA levels in biopsies as risk factors for greater inflammation during the course of UC.
It has been predicted that the DNA sequence around the −1123G/C site of the PTPN22 gene showed its perfect match with that of the binding site for transcription factor activator protein 4 (AP-4). The −1123G/C is located at the critical region of the core motif of the AP-4 binding consensus sequence (−1130gcaaGCTGaa−1121; core motif is shown in uppercase, the position −1123G is in bold). A transcription factor binding site for AP-4 at position −1123 is predicted in the presence of the G allele rather than the C allele [30]. Our results showed that PTPN22 mRNA levels in biopsies were not associated with −1123G/C polymorphism in PTPN22 gene. Huang et al. also found no significant impact of the PTPN22 −1123G/C polymorphism on PTPN22 mRNA expression, although the polymorphism was associated with rheumatoid arthritis [14]. The genotype-related difference in PTPN22 mRNA levels may be confined to certain T-cell subpopulations or a lack of statistical power. As a matter of fact, PTPN22 mRNA levels are affected not only by PTPN22 gene polymorphism, but also other related polymorphic genes, such as HLA, has been envisaged [23]. Further studies are required in order to clarify whether AP-4 influences the transcription activities of the PTPN22 gene.
In conclusion, our study suggests that the C carrier of −1123G/C in PTPN22 gene was associated with UC in the Han Chinese in central China; PTPN22 mRNA levels in colonic biopsies were highly expressed in UC, especially in active disease, and were correlated with CRP levels and disease activity. We recognized that our current study had limitations of small sample size and lack of functional characterization of the C mutation at this position in the promoter activity and T-cell activation. Therefore, further studies with a larger sample size in independent cohorts from the same ethnic group are necessary to determine the relation of the PTPN22 −1123G/C polymorphism with UC patients and to investigate the function of the PTPN22 gene polymorphism.
References
Xavier RJ, Podolsky DK (2007) Unravelling the pathogenesis of inflammatory bowel disease. Nature 448:427–434
Behrens TW (2011) Lyp breakdown and autoimmunity. Nat Genet 43:821–822
Zhang J, Zahir N, Jiang Q et al (2011) The autoimmune disease-associated PTPN22 variant promotes calpain-mediated LYP/Pep degradation associated with lymphocyte and dendritic cell hyperresponsiveness. Nat Genet 43:902–907
Cloutier JF, Veillette A (1999) Cooperative inhibition of T-cell antigen receptor signaling by a complex between a kinase and a phosphatase. J Exp Med 189:111–121
Wu S, Bottini M, Rickert RC et al (2009) In silico screening for PTPN22 inhibitors: active hits from an inactive phosphatase conformation. ChemMedChem 4:440–444
Xie Y, Liu Y, Gong G et al (2008) Discovery of a novel submicromolar inhibitor of the lymphoid specific tyrosine phosphatase. Bioorg Med Chem Lett 18:2840–2844
Stanford SM, Mustelin TM, Bottini N (2010) Lymphoid tyrosine phosphatase and autoimmunity: human genetics rediscovers tyrosine phosphatases. Semin Immunopathol 32:127–136
Dultz G, Matheis N, Dittmar M et al (2009) The protein tyrosine phosphatase non-receptor type 22 C1858T polymorphism is a joint susceptibility locus for immunthyroiditis and autoimmune diabetes. Thyroid 19:143–148
Bottini N, Vang T, Cucca F et al (2006) Role of PTPN22 in type 1 diabetes and other autoimmune diseases. Semin Immunol 18:207–213
Chung SA, Criswell LA (2007) PTPN22: its role in SLE and autoimmunity. Autoimmunity 40:582–590
Diaz-Gallo LM, Espino-Paisán L, Fransen K et al (2011) Differential association of two PTPN22 coding variants with Crohn’s disease and ulcerative colitis. Inflamm Bowel Dis 17:2287–2294
Kawasaki E, Awata T, Ikegami H et al (2006) Systematic search for single nucleotide polymorphisms in a lymphoid tyrosine phosphatase gene (PTPN22): association between a promoter polymorphism and type 1 diabetes in Asian populations. Am J Med Genet A 140:586–593
Liu F, Liu J, Zheng TS et al (2012) The −1123G>C variant of PTPN22 gene promoter is associated with latent autoimmune diabetes in adult Chinese Hans. Cell Biochem Biophys 62:273–279
Huang JJ, Qiu YR, Li HX et al (2012) A PTPN22 promoter polymorphism −1123G>C is associated with RA pathogenesis in Chinese. Rheumatol Int 32:767–771
Feng X, Li YZ, Zhang Y et al (2010) Association of the PTPN22 gene (−1123G>C) polymorphism with rheumatoid arthritis in Chinese patients. Tissue Antigens 76:297–300
Orrú V, Tsai SJ, Rueda B et al (2009) A loss-of-function variant of PTPN22 is associated with reduced risk of systemic lupus erythematosus. Hum Mol Genet 18:569–579
Rodríguez-Rodríguez L, Taib WR, Topless R et al (2011) The PTPN22 R263Q polymorphism is a risk factor for rheumatoid arthritis in Caucasian case–control samples. Arthritis Rheum 63:365–372
Lennard-Jones JE (1989) Classification of inflammatory bowel disease. Scand J Gastroenterol Suppl 170:2–6
Satsangi J, Silverberg MS, Vermeire S et al (2006) The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut 55:749–753
Truelove SC, Witts LJ (1955) Cortisone in ulcerative colitis; final report on a therapeutic trial. Br Med J 2:1041–1048
Chang HH, Tai TS, Lu B et al (2012) PTPN22.6, a dominant negative isoform of PTPN22 and potential biomarker of rheumatoid arthritis. PLoS One 7:e33067
Schmittgen TD, Livak KJ (2008) Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc 3:1101–1108
Inoue A, Takahashi KA, Arai Y et al (2006) The therapeutic effects of basic fibroblast growth factor contained in gelatin hydrogel microspheres on experimental osteoarthritis in the rabbit knee. Arthritis Rheum 54:264–270
Oikonomou KA, Kapsoritakis AN, Kapsoritaki AI et al (2011) Angiogenin, angiopoietin-1, angiopoietin-2, and endostatin serum levels in inflammatory bowel disease. Inflamm Bowel Dis 17:963–970
Viken MK, Olsson M, Flåm ST et al (2007) The PTPN22 promoter polymorphism −1123G>C association cannot be distinguished from the 1858C>T association in a Norwegian rheumatoid arthritis material. Tissue Antigens 70:190–197
Jostins L, Ripke S, Weersma RK et al (2012) Host–microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature 491:119–124
Mori M, Yamada R, Kobayashi K et al (2005) Ethnic differences in allele frequency of autoimmune-disease-associated SNPs. J Hum Genet 50:264–266
Ronninger M, Guo Y, Shchetynsky K et al (2012) The balance of expression of PTPN22 splice forms is significantly different in rheumatoid arthritis patients compared with controls. Genome Med 4:2
Wu J, Katrekar A, Honigberg LA et al (2006) Identification of substrates of human protein-tyrosine phosphatase PTPN22. J Biol Chem 281:11002–11010
Jüliger S, Bongartz M, Luty AJ et al (2003) Functional analysis of a promoter variant of the gene encoding the interferon-gamma receptor chain I. Immunogenetics 54:675–680
Acknowledgments
This project was supported by grants from the Bureau of Public Health of Wuhan (WX12C34).
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, Z., Zhang, H., Xia, B. et al. Association of PTPN22 gene (rs2488457) polymorphism with ulcerative colitis and high levels of PTPN22 mRNA in ulcerative colitis. Int J Colorectal Dis 28, 1351–1358 (2013). https://doi.org/10.1007/s00384-013-1671-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-013-1671-3