Abstract
We aimed to determine P268S and M863V polymorphisms in NOD2/CARD15 genes associated with an increased risk of developing Crohn’s disease (CD) and ulcerative colitis (UC) and to establish correlations between P268S and M863V genotypes in Turkish population. This study included 152 healthy controls and 138 patients (62 CD and 76 UC) with IBD. Our results, the P268S CC genotype was prevalent on patients and controls (45 vs. 66%), followed by genotypes CT (48 vs. 28%) and TT (7 vs. 6%) in CD. The prevalence of genotypes of CC (wild-type), CT (heterozygous mutant) and TT (homozygous mutant) profiles for the P268S polymorphism were 68, 25 and 7% respectively in UC patients, and 66, 28 and 6% respectively in healthy control groups. We were found in wild-type M863V in all subjects and no other mutant band. P268S polymorphism may be associated with CD susceptibility in Turkish population, whereas there is not associated between M863V polymorphisms and patients with IBD in Turkish population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Inflammatory bowel disease (IBD) is a polygenic disorder characterized by systemic and gastrointestinal manifestations [1, 2]. In addition, IBD is a chronic and multifactorial disease of the gastrointestinal tract that includes tree similar, yet distinct conditions, namely Crohn’s disease (CD), ulcerative colitis (UC), and undetermined colitis [3]. UC and CD are chronic IBD which are similar to each other for their clinical features and epidemiology [4–6]. In recent years, the prevalence of IBD has increased in Europe and has been reported to increase gradually in Asia. The etiology and pathogenesis of IBD is not clear. However, it is suggested that various factors such as genetics, immunology, environment and infection may be complex interactions [7].
NOD2/CARD15 encodes a protein involved in bacterial recognition by monocytes and is the first verified predisposing gene for CD [7–9]. Mutations in CARD15 (16q12, Protein: NOD2) have been found in patients with CD, where three NOD2/CARD15 polymorphisms, R702W, G908R, and L1007fs, were found to be significantly associated with CD in Caucasian populations [7, 8]. These single nucleotide polymorphisms (SNPs) were not reported to be related with CD in Japanese. Also, the role of these polymorphisms in the CD should be discussed in Hubei, Zhejiang or Hong Kong populations in China [8]. R702W, G908R, and 1007fs mutations are associated with susceptibility CD but not UC [10, 11]. It has also been verified that these mutations are independently associated with CD susceptibility. However, it has been reported that this effect has changed according to ethnic and even regional differences [9].
The P268S and M863V polymorphisms in the NOD2/CARD15 gene have been investigated in different populations [7, 12–14]. It has been reported that M863V polymorphism is usually found in Ashkenazi Jews but not in other populations [13]. P268S polymorphism has been shown to be associated with CD susceptibility in the Zhuang population in the Guangxi Zhuang Autonomous Region, China [7].
We aimed to determine P268S and M863V polymorphisms in NOD2/CARD15 genes associated with an increased risk of developing UC and CD and to establish correlations between P268S and M863V genotypes in Turkish population.
MATERIALS AND METHODS
A total of 290 subjects were investigated. The study included 62 patients with CD (32 males, mean age 41.5 ± 11.56 years; 30 females, mean age 47.1 ± 14.71 years), 76 patients with UC (41 males 47.9 ± 15.29 years; 35 females, mean age 45.7 ± 16.51 years) of which 138 exhibited IBD as confirmed by endoscopy and histology. All patients were diagnosed at the Gastroenterology clinic of Niğ de State Hospital, Niğde, Turkey. Diagnosis of CD and UC were based on generally accepted clinical, endoscopical and histological criteria. The control group consisted of 152 healthy volunteers (59 males, mean age 41.8 ± 14.88 years; 93 females, mean age 44.0 ± 16.43 years) collected from hospital staff, students, and healthy subjects.
Genomic DNA was extracted from the whole blood treated with EDTA using the QIAamp DNA Blood Mini Kit (Maryland, USA), following the manufacturer’s protocol. The extracted DNA was stored at –20°C until analysis.
The selected polymorphisms of genes with previously confirmed evidence for association with CD and UC were as follows: NOD2/CARD15: rs2066842 (P268S), rs104895447 (M863V). The polymerase chain reaction (PCR) reactions were performed in the ABI (Applied Biosystems). The P268S (Primers; F: 5'‑TGCCTCTTCTTCTGCCTTCC-3', R: (5'-AGTA-GAGTCCGCACAGAGAG-3') and M863V (Primers; F: (5'-CTGTTTGCATGATGGGGGG-3', R: (5'-GG-GAGATCACAGCATTAGAG-3') gene regions were amplified using PCR, detected by restriction fragment length polymorphism (RFLP) [7, 13]. PCR reaction conditions consisted of an initial denaturation for 5 min at 94°C, followed by 35 cycles of denaturation at 94°C for 45 s, annealing at different temperatures (P268S; 60°C, M863V; 55°C), for 45 s, extension at 72°C for 45 s, and a final extension at 72°C for 5 min. All of the PCR products were electrophoresed on a 1.5% agarose gel with 1 × Tris-borate-EDTA buffer at 100 V for 30 min and then observed under ultraviolet illumination. The PCR products of P268S, and M863V SNPs of the NOD2/CARD15 gene were digested at 37°C for 12 h with BamHI, (wild-type; 422 bp, heterozygote mutant; 422 bp + 247 bp + 175 bp, and homozygote mutant; 247 + 175 bp) and NcoI (wild-type; 212 + 160 bp, heterozygote mutant; 372 + 212 + 160 bp, and homozygote mutant; 372 bp) restriction enzymes, respectively. The fragments were separated and visualized using gel electrophoresis.
Statistical analysis was performed by using SPSS version 15. The frequency distribution of alleles and genotypes mutations in CD patients, UC patients, and controls were compared using chi-square analysis. For each polymorphism, unconditional logistic regression was used to calculate odds ratios (OR) and 95% confidence intervals (95% CI). All data were expressed as means ± standard deviation (SD). The P value (<0.05) was considered statistically significant in all variables. Calculation of the Hardy–Weinberg equilibrium were performed using Michael H. Court’s (2005–2008) online calculator http://www.tufts.edu/~mcourt01/Documents/ Court%20lab%20%20HW%20calculator.xls.
RESULTS AND DISCUSSION
We investigated the frequencies of the two NOD2/CARD15 gene polymorphisms (P268S and M863V) in 138 patients with CD (n = 62), UC (n = 76) and compared them with 152 controls. The ages of the CD patients were between 18 and 82 years (52%♂, 48%♀); the ages of the control groups were between 18 and 87 years (39%♂, 61%♀). Mean ages were 44.2 ± 13.36 years for the CD patients, 43.2 ± 15.84 years for the control groups. In the CD patients group, 11% (n = 7) were located in colon, 47% (n = 29) were in ileocolon, and 42% (n = 26) were in ileum. The ages of the UC patients were between 19 and 86 years (54%♂, 46%♀), with a mean age of 46.9 ± 15.80 years. While 76 of the UC patients were 46% female and 54% were male, 152 (43.2 ± 15.84 years) of the control groups were 61% female and 39% were male In the UC patients group; 34% (n = 26) were located in rectum, 53% (n = 40) were in left colon, 13% (n = 10) were located in the whole colon.
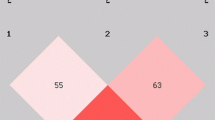
The genotype and allele frequencies of the P268S and M863V polymorphisms in CD patients and healthy controls are shown in Figs. 1, 2 and Table 1.
According our results, the P268S CC genotype was prevalent on patients and controls (45 vs. 66%), followed by genotypes CT (48 vs. 28%) and TT (7 vs. 6%) in CD (Table 1). The mutant allele frequencies of P268S in the patient group were 31%, respectively, compared with frequencies of 20%, respectively, in the control group. The CT genotype of P268S was statistically significant when compared with controls in patients with CD (OR, 2.577: 95% CI, 1.375–4.829; P = 0.003). In addition, the T allele of P268S was over represented in patients with CD compared with that in controls (OR, 0.557: 95% CI, 0.346–0.895; P = 0.015). However, there was no significant associations other genotype TT (OR, 1.603: 95% CI, 1.603; P = 0.456 in the CD patients. The analysed P268S polymorphism was in Hardy–Weinberg equilibrium both in CD patients (χ2 = 1.186, p = 0.27) and healthy controls (χ2 = 2.485, p = 0.12). The mutant genotype for M863V was not detected in any of the CD patients and controls. Just two bands of 212 and 160 bp were found in wild-type M863V in all subjects and no other mutant band (372 and 372 + 212 + 160 bp) of M863V was detected using PCR-RFLP fragment electrophoresis.
Seventy six patients with UC and one hundred and fifty two control subjects from the general population were genotyped for the presence of P268S and M863V polymorphisms. Distribution of genotype and allele frequencies are presented in Table 2.
The prevalence of genotypes of CC (wild-type), CT (heterozygous mutant) and TT (homozygous mutant) profiles for the P268S polymorphism were 68, 25 and 7% respectively in UC patients, and 66, 28 and 6% respectively in healthy control groups (Table 2). No significant difference was noticed in genotype and allele distributions of the P268S polymorphism between the control and patient groups. Likewise, no significant association of UC patients and control group with the M863V polymorphism was found in either cohort. Furthermore, the AG and GG genotypes in M863V polymorphism were not observed in both the UC patients and the control group, and all of the individuals had AA variants (Table 2). When the genotypes distributions of NOD2/CARD15 gene P268S polymorphism were evaluated, no deviation was observed in Hardy–Weinberg equilibrium patients (χ2 = 2.753, p = 0.10) or control group (χ2 = 2.485, p = 0.12).
In this study, NOD2/CARD15 gene P268S and M863V polymorphisms were investigated in the control group with CD and UC. According to our results, we found that CT genotype and T allele frequency of NOD2/CARD15 gene P268S polymorphisms were statistically significant in CD patients (P < 0.05). However, there were no heterozygous or homozygous mutations for M863V polymorphisms in this study.
P268S polymorphism has rarely been reported in Turkey. Ince et al. [14] researched NOD2/CARD15 genetic mutations (1007fs, G908R, R702W) and P268S, IVS8+158 polymorphisms in Turkish inflammatory bowel disease patients. 130 inflammatory bowel disease patients (67 CD, 63 UC) and 87 healthy controls were examined in this survey. Their study demonstrated that R702W gene mutation was significantly lower in the inflammatory bowel disease group (1.5%) than the controls (4.8%) (P < 0.05) [14]. The results also showed that there was no significant statistical difference between CD, UC and control groups for P268S gene polymorphism. On the contrary, our study demonstrated that CT genotype and T allele frequency of P268S polymorphisms were statistically significant in CD patients (P < 0.05).
There is evidence that the prevalence of CD may depend on geographical region and race basis. It is known that R702W, G908R and L1007fsinsC mutations in the NOD2/CARD15 gene in the Caucasus are associated with CD [15, 16]. The CD prevalence was found to be higher in the Ashkenazi Jews than in the Sephardic Jews (originally Mediterranean, North Africa and Asia) [17]. Several studies have reported that the rate of mutation in Israeli Jewish patients is 27–41% [18, 19]. Karban et al. [15] told that the CH prevalence was much lower in Israeli Arabs compared to the entire population in a survey of Israeli Arabs and Israeli Jews [15]. Sugimura et al. [20] also studied NOD2/CARD15 gene polymorphism in 211 Crohn’s patients (64 Ashkenazi Jews and 147 non-Jewish white families). In this study, the 268S-JW1 combination in the NOD2/CARD15 gene shown that a further increased risk (OR = 5.75, P = 0.0005) and the highest population-attributable risk (15.1%) for CD among reported disease-prone mutations (DPMs) in Jews [20]. In another study of the Ashkenazi and Sephardic Jewish families in America, it was determined that P268S polymorphism is important in Crohn’s disease in Ashkenazi Jews [13]. Similar results were obtained in another study conducted in Europe [9].
In recent years, the incidence of CD, a complex IBD, has been reported to increase rapidly. Scudiero et al. [21] comparatively analyzed, by PCR and direct sequencing, the exons 4, 8 and 11 of NOD2/CARD15 gene in Italian patients with CD (n = 42) and in controls (n = 66). Furthermore, these investigators found that the allele T frequency of c.802C > T (p.P268S) SNP (rs2066842) was significantly higher than that of healthy controls in CD patients (p = 0.018; OR = 2.02) [21]. Our results are similar to the results of these researchers in P268S polymorphism. In another study examined the association of nine polymorphisms in four different genes with the development of CD and UC in Saudi patients with IBD. It has been shown that association of IBD with nine gene polymorphisms was only significant in two of these polymorphic variants in this study [22].
The M863V polymorphism of the NOD2/CARD15 gene was found to be significantly associated with CD in Ashkenazi Jewish populations [13]. Our results indicated that M863V mutations of the NOD2/CARD15 gene were not detected in Turkish patients with IBD. All individuals in the patients (CD and UC) and controls were identified as homozygous wild-type. This is the first study to report the M863V mutations of the NOD2/CARD15 gene in patients with CD and UC in Turkish population.
CONCLUSIONS
In conclusion, in this study we investigated the P268S and M863V polymorphisms of NOD2/CARD15 gene that are associated with CD and UC patients. In Turkish population, it has been determined that P268S polymorphism may be associated with in CD patient, but M863V polymorphism is not associated with both CD and UC patients.
REFERENCES
Lacher, M., Schroepf, S., Ballauff, A., Lohse, P., Von Schweinitz, D., Kappler, R., and Koletzko, S., Autophagy 16-like 1 rs2241880 G allele is associated with Crohn’s disease in German children, Acta. Paediatr., 2009, vol. 98, no. 11, pp. 1835–1840. https://doi.org/10.1111/j.1651-2227.2009.01438.x
Latiano, A., Palmieri, O., Valvano, M.R., D’Incà, R., Cucchiara, S., Riegler, G., Staiano, A.M., Ardizzone, S., Accomando, S., de Angelis, G.L., Corritore, G., Bossa, F., and Annese, V., Replication of interleukin 23 receptor and autophagy-related 16-like 1 association in adult-and pediatric-onset inflammatory bowel disease in Italy, World. J. Gastroenterol., 2008, vol. 14, no. 29, pp. 4643–4651. https://doi.org/10.3748/wjg.14.4643
Serbati, N., Senhaji, N., Diakite, B., Badre, W., and Nadifi, S., IL23R and ATG16L1 variants in Moroccan patients with inflammatory bowel disease, BMC Res. Notes, 2014, vol. 7, pp. 570–75. https://doi.org/10.1186/1756-0500-7-570
Boirivant, M. and Cossu, A., Inflammatory bowel disease, Oral. Dis., 2012, vol. 18, no. 1, pp. 1–15. https://doi.org/10.1111/j.1601-0825.2011.01811.x
Barreiro-de Acosta, M. and Peña, A.S., Clinical applications of NOD2/CARD15 mutations in Crohn’s disease, Acta Gastroenterol. Latinoam., 2007, vol. 37, no. 1, pp. 49–54.
El-Tawil, A.M., Genetic predisposition and inflammatory bowel disease, Gastroenterol. Res., 2013, vol. 6, no. 1, pp. 1–3. https://doi.org/10.4021/gr523w
Long, W.Y., Chen, L., Zhang, C.L., Nong, R.M., Lin, M.J., Zhan, L.L., and Lv, X.P., Association between NOD2/CARD15 gene polymorphisms and Crohn’s disease in Chinese Zhuang patients, World. J. Gastroenterol., 2014, vol. 20, no. 16, pp. 4737–4744. https://doi.org/10.3748/wjg.v20.i16.4737
Chen, L., Lin, M.J., Zhan, L.L., and Lv, X.P., Analysis of TLR4 and TLR2 polymorphisms in inflammatory bowel disease in a Guangxi Zhuang population, World. J. Gastroenterol., 2012, vol. 18, no. 46, pp. 6856–6860. https://doi.org/10.3748/wjg.v18.i46.6856
Lesage, S., Zouali, H., Cézard, J.P., Colombel, J.F., Belaiche, J., Almer, S., Tysk, C., O’Morain, C., Gassull, M., Binder, V., Finkel, Y., Modigliani, R., Gower-Rousseau, C., Macry, J., Merlin, F., Chamaillard, M., Jannot, A.S., Thomas, G., and Hugot, J.P., CARD15/NOD2 mutational analysis and genotype-phenotype correlation in 612 patients with inflammatory bowel disease, Am. J. Hum. Genet., 2002, vol. 70, no. 4, pp. 845–857. https://doi.org/10.1086/339432
Hampe, J., Cuthbert, A., Croucher, P.J., Mirza, M.M., Mascheretti, S., Fisher, S., Frenzel, H., King, K., Hasselmeyer, A., MacPherson, A.J., Bridger, S., van Deventer, S., Forbes, A., Nikolaus, S., Lennard-Jones, J.E., Foelsch, U.R., Krawczak, M., Lewis, C., Schreiber, S., and Mathew, C.G., Association between insertion mutation in NOD2 gene and Crohn’s disease in German and British populations, Lancet, 2001, vol. 357, no. 9272, pp. 1925–1928. https://doi.org/10.1016/S0140-6736(00)05063-7
Hugot, J.P., Chamaillard, M., Zouali, H., Lesage, S., Cézard, J.P., Belaiche, J., Almer, S., Tysk, C., O’Morain, C.A., Gassull, M., Binder, V., Finkel, Y., Cortot, A., Modigliani, R., Laurent-Puig, P., Gower-Rousseau, C., Macry, J., Colombel, J.F., Sahbatou, M., and Thomas, G., Association of NOD2 leucine- rich repeat variants with susceptibility to Crohn’s disease, Nature, 2001, vol. 411, no. 6837, pp. 599–603. https://doi.org/10.1038/35079107
Medici, V., Mascheretti, S., Croucher, P.J.P., Stoll, M., Hampe, J., Grebe, J., Sturniolo, G.C., Solberg, C., Jahnsen, J., Moum, B., Schreiber, S., and Vatn, M.H., Extreme heterogeneity in CARD15 and DLG5 Crohn disease-associated polymorphisms between German and Norwegian populations, Eur. J. Hum. Genet. 2006, vol. 14, no. 4, pp.459–468. https://doi.org/10.1038/sj.ejhg.5201576
Tukel, T., Present, D., Rachmilewitz, D., Mayer, L., Grant, D., Risch, N., Shalata, A., and Desnick, R.J., Crohn disease: frequency and nature of CARD15 mutations in Ashkenazi and Sephardi/oriental Jewish families, Am. J. Hum. Genet., 2004, vol. 74, no. 4, pp. 623–636. https://doi.org/10.1086/382226
Ince, A.T., Hatirnaz, O., Ovünc, O., and Ozbek, U., 1007fs, G908R, R702W mutations and P268S, IVS8+158 polymorphisms of the CARD15 gene in Turkish inflammatory bowel disease patients and their relationship with disease-related surgery, Dig. Dis. Sci., 2008, vol. 53, no. 6, pp. 1683–92. https://doi.org/10.1007/s10620-007-0054-4
Karban, A., Atia, O., Leitersdorf, E., Shahbari, A., Sbeit, W., Ackerman, Z., and Eliakim, R., The relation between NOD2/CARD15 mutations and the prevalence and phenotypic heterogeneity of Crohn’s disease: lessons from the Israeli Arab Crohn’s disease cohort, Dig. Dis. Sci., 2005, vol. 50, no. 9, pp. 1692–1697. https://doi.org/10.1007/s10620-005-2917-x
Gasche, C., Nemeth, M., Grundtner, P., Willheim-Polli, C., Ferenci, P., and Schwarzenbacher, R., Evolution of Crohn’s disease-associated Nod2 mutations, Immunogenetics, 2008, vol. 60, no. 2, pp. 115–120. https://doi.org/10.1007/s00251-008-0274-6
Yang, H., McElree, C., Roth, M.P., Shanahan, F., Targan, S.R., and Rotter, J.I., Familial empiric risks for inflammatory bowel disease: difference between Jews and non-Jews, Gut, 1993, vol. 34, no. 4, pp. 517–524. https://doi.org/10.1136/gut.34.4.517
Fidder, H.H., Olschwang, S., Avidan, B., Zouali, H., Lang, A., Bardan, E., and Chowers, Y., Association between mutations in the CARD15 (NOD2) gene and Crohn’s disease in Israeli Jewish patients, Am. J. Med. Genet., 2003, vol. 121, no. 3, pp. 240–244. https://doi.org/10.1002/ajmg.a.20209
Karban, A., Waterman, M., Panhuysen, C.I., Pollak, R.D., Nesher, S., Datta, L., Weiss, B., Suissa, A., Shamir, R., Brant, S.R., and Eliakim, R., NOD2/CARD15 genotype and phenotype differences between Ashkenazi and Sephardic Jews with Crohn’s disease, Am. J. Gastroenterol., 2004, vol. 99, no. 6, pp. 1134–1140. https://doi.org/10.1111/j.1572-0241.2004.04156.x
Sugimura, K., Taylor, K.D., Lin, Y.C., Hang, T., Wang, D., Tang, Y.M., and Yang, H.A., Novel NOD2/CARD15 haplotype conferring risk for Crohn disease in Ashkenazi Jews, Am. J. Hum. Genet., 2003, vol. 72, no. 3, pp. 509–518. https://doi.org/10.1086/367848
Scudiero, O., Nigro, E., Monaco, M.L., Polito, R., Capasso, M., Canani, B.R., Castaldo, G., and Daniele, A., 802C>T NOD2/CARD15 SNP is associated to Crohn’s disease in Italian patients, Hered. Genet., 2015, S7. https://doi.org/10.4172/2161-1041.S7-005
Al-Sulaiman, R.M., Ismail, M.H., Yasawy, M.I., Al-Ateeq, S.A., Abdelrashid, M.M., Hussameddin, A.M., and Al-Quorain, A.A., Association of NOD2/CARD15, DLG5, OCTN1 and toll-like receptor 4 gene polymorphisms with inflammatory bowel disease: a university hospital experience, Saudi. J. Med. Med. Sci., 2014, vol. 2, no. 2, pp. 81–85. https://doi.org/10.4103/1658-631X.136988
Funding
We would like to thank the Scientific Research Project Unit of Niğde Ömer Halisdemir University (project no. FEB 2015/19 BAGEP).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests. The authors declare that they have no conflict of interest.
Statement of compliance with standards of research involving humans as subjects. The study was approved by the local ethics committee (Erciyes University School of Medicine, KAEK 2013/729 and KAEK 2016/148 and all the participants provided appropriate consent. This study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki.
About this article
Cite this article
Diler, S.B., Polat, F. & Yaraş, S. The P268S and M863V Polymorphisms of the NOD2/CARD15 Gene in Crohn’s Disease and Ulcerative Colitis. Cytol. Genet. 53, 424–429 (2019). https://doi.org/10.3103/S0095452719050074
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.3103/S0095452719050074