Abstract
Background
Data addressing the outcomes and patterns of recurrence after pulmonary metastasectomy (PM) in patients with colorectal cancer (CRC) and previously resected liver metastasis are limited.
Methods
We searched the PubMed database for studies assessing PM in CRC and gathered individual data for patients who had PM and a previous curative liver resection. The influence of potential factors on overall survival (OS) was analyzed through univariate and multivariate analysis.
Results
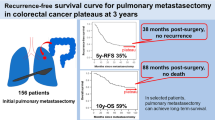
Between 1983 and 2009, 146 patients from five studies underwent PM and had previous liver resection. The median interval from resection of liver metastasis until detection of lung metastasis and the median follow-up from PM were 23 and 48 months, respectively. Five-year OS and recurrence-free survival rates calculated from the date of PM were 54.4 and 29.3 %, respectively. Factors predicting inferior OS in univariate analysis included thoracic lymph node (LN) involvement and size of largest lung nodule ≥2 cm. Adjuvant chemotherapy and whether lung metastasis was detected synchronous or metachronous to liver metastasis had no influence on survival. In multivariate analysis, thoracic LN involvement emerged as the only independent factor (hazard ratio 4.86, 95 % confidence interval 1.56–15.14, p = 0.006).
Conclusions
PM offers a chance for long-term survival in selected patients with CRC and previously resected liver metastasis. Thoracic LN involvement predicted poor prognosis; therefore, significant efforts should be undertaken for adequate staging of the mediastinum before PM. In addition, adequate intraoperative LN sampling allows proper prognostic stratification and enrollment in novel adjuvant therapy trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Pulmonary metastasectomy (PM) has become a standard therapeutic strategy for patients with resectable lung metastasis from colorectal cancer (CRC). The wide acceptance of this surgery is based on retrospective data showing encouraging 5-year overall survival (OS) rates of 40–60 %.1–7
Approximately two thirds of patients with metastatic CRC develop extrahepatic recurrence after hepatic metastasectomy, with lungs being a common site of recurrence.8,9 Although there is no uniform agreement on the optimal management of these patients once they develop lung metastasis, the indications for PM has expanded to include this subgroup based on data showing encouraging 5-year OS rates of 30–50 % after PM.2–4,10,11
Conflicting data exist from literature concerning the prognostic significance of previously resected liver metastasis on outcomes after PM. Although some studies reported inferior outcome after PM, majority of studies failed to reveal any adverse influence of previously resected liver metastasis on survival.2,4–6,10,12,13 Therefore, patients should not be denied PM if they have prior liver resections. The challenge is to identify methods for selection.
Although most CRC patients with lung metastasis have previous liver metastasis, patients with prior curative liver resection constitute only 20–40 % of the cohorts of most studies of PM in CRC.6,10,12,14 Therefore, the applicability of the prognostic factors identified in those studies to the subpopulation with previous liver metastasis is not realistically possible. Therefore, we undertook a separate analysis to investigate the influence of clinicopathologic parameters on survival of that particular subgroup through pooling of individual patients’ data, in order to provide better understanding of expected outcomes and factors influencing survival.
Methods
Search Strategy and Data Collection
The search methods were previously reported in a previous pooled analysis that was performed to construct a lung metastasectomy prognostic model and included a PubMed search to identify studies assessing PM in CRC, using the following terms: (lung metastasis), (colon cancer), (surgery) or (metastasectomy).6 Studies including <20 patients or published before the year 2000 were excluded. For this current analysis, the authors of the retrieved articles were asked to provide data for every patient with previously treated liver metastasis. Data included age, gender, status of lymph node (LN) in the primary CRC, previous therapy for liver metastasis, and the disease-free interval (DFI) defined as the interval from liver resection until detection of lung metastasis. Furthermore, we collected data on characteristics of lung metastasis, details of PM, prethoracotomy carcinoembryonic antigen (CEA), whether adjuvant chemotherapy was given, whether intraoperative LN sampling was performed, and whether patients had pathologically confirmed thoracic LN involvement. Additionally, detailed data of any recurrences after PM and dates of last follow-up or death were documented.
Statistical Analysis
Survival curves were calculated according to the Kaplan–Meier method and compared by means of the log-rank test. p < 0.05 was considered to indicate a statistically significant difference. Factors with p values of <0.1 in the univariate analysis were entered into the multivariate analysis and tested with the backward stepwise Cox regression model. Heterogeneity between patient’s characteristics from different studies was measured using a fixed-effect model and expressed by the χ 2 test. All statistical analyses were carried out with SPSS software, version 16 (IBM, Armonk, NY).
Results
Search Results and Patients
Our search strategy retrieved 84 relevant retrospective studies. Forty-three studies were excluded because they included <20 patients and/or they were published before the year 2000; 41 remained eligible. Authors of five studies included 163 patients and provided detailed data for their patients.11,12,15–17
Seventeen patients were excluded because liver metastases were treated with nonoperative therapies, and 13 were excluded for incomplete resection of lung metastasis. All the other 146 patients had complete (R0) resection of liver metastasis and subsequently had complete (R0) resection of lung metastasis. Pulmonary metastasis was detected at a median interval of 23 months after liver resection. Lung and liver metastasis were detected simultaneously in seven patients; all of these seven patients had PM within 2 months after hepatic resection. All 146 patients had pathologically confirmed liver and lung metastasis.
The first PM was carried out through video-assisted thoracic surgery (VATS) in 31 patients; the rest underwent thoracotomies.
Demographic, disease-related characteristics, and therapeutic strategies for the patients are outlined in Table 1.
Survival Outcomes
At the time of analysis, 63 patients had died of disease. The 5-year OS calculated from the date of PM for the entire cohort was 54.4 %. The corresponding 5-year recurrence-free survival (RFS) was 29.3 %.
There was no statistically significant difference in the 5-year OS between patients who underwent VATS resection or thoracotomy (46 and 53 %, respectively, p = 0.82). Likewise, no statistically significant differences in 5-year RFS were observed (16 and 31 %, respectively, p = 0.37).
Interestingly, performing intraoperative LN sampling had no influence on outcomes. Patients whose operation included LN sampling had 5-year RFS of 25 % compared to 34 % for patients without LN sampling (p = 0.33). Furthermore, OS was not statistically different between the two groups; 5-year OS of 42 and 60 %, respectively (p = 0.14). Nine patients had pathologically confirmed thoracic LN involvement identified through intraoperative sampling and had inferior OS in univariate analysis (Fig. 1). Thoracic LN involvement also predicted higher risk of recurrence. The RFS and OS outcomes by status of thoracic LN involvement are outlined in Table 2. Size of largest pulmonary nodule of ≥2 cm was another factor that correlated with inferior OS (Table 1). The other factors did not influence OS. However, status of LN in the primary CRC approached statistical significance (p = 0.055). In multivariate analysis, thoracic LN involvement emerged as the sole independent factor that correlated with inferior OS (hazard ratio 4.86, 95 % confidence interval 1.56–15.43, p = 0.006); whereas status of LN in the primary CRC and size of largest nodule ≥2 cm were not significant.
No heterogeneity in patient and disease characteristics was identified among patients included from the different studies (χ 2 test = 0.93, p = 0.5771).
At the date of last follow-up, we observed 12 patients who survived for more than 10 years from the first PM, including patients with multiple nodules, bilateral lung metastasis, and repeated pulmonary resection. Six of those 12 patients were free of disease at >10 years after PM.
Patients with Synchronous Liver and Lung Presentation
Synchronous liver–lung presentation was defined as detection of lung metastasis within 6 months of surgical resection of liver metastasis, whereas metachronous presentation was defined as detection of lung metastasis later than 6 months.
The 5-year OS of the 26 patients with synchronous presentation was not statistically different from the OS of patients with metachronous presentation (57 and 55 %, respectively, p = 0.96). Additionally, the OS of the seven patients with simultaneously detected liver and lung metastases was not statistically different from the OS of patients whose lung metastasis was detected at a later time (5-year OS 64 and 55 %, respectively, p = 0.85). Furthermore, no significant OS differences based on the DFI at different cutoffs of 12, 24, and 36 months were identified.
Influence of Adjuvant Chemotherapy on Survival
Forty-eight patients received adjuvant 5-fluorouracil-based chemotherapy. We assessed the influence of adjuvant chemotherapy on the OS by univariate analysis, by including chemotherapy in the multivariate analysis model and by exploratory subanalyses.
There was no difference in median OS between patients who received chemotherapy and those who did not (63.8 and 59.3 months, respectively, p = 0.98). In addition, median RFS was comparable between the two groups (23.0 and 22.9 months, respectively, p = 0.83) (Fig. 2). After adding chemotherapy to the multivariate analysis, thoracic LN involvement emerged as the sole independent prognostic factor for OS (hazard ratio 6.76, 95 % confidence interval 1.77–25.78, p = 0.005). Finally, exploratory subanalyses did not identify any subgroup that derived OS or RFS advantage of chemotherapy.
Recurrence Outcomes
Ninety-three patients (64 %) had documented recurrence after PM. The exact interval from resection of lung metastasis to recurrence was uncertain for 15 patients. The other 78 patients had median time to recurrence of 13 months (range 3–81.8 months). Data about patterns of first recurrence were available for 91 patients; 46 (50 %) had isolated recurrence in the lungs (21 had repeated PM), 14 (16 %) had isolated recurrence in liver (eight had repeated liver resection), and 31 (34 %) had other or multiple metastatic sites.
Influence of Patterns of Recurrence on Postrecurrence Survival
Seventy-four patients were assessable for the influence of patterns of recurrence on postrecurrence survival and were divided into 4 groups; lung-only recurrence treated with repeated PM (n = 21), lung-only recurrence treated with chemotherapy (n = 20), liver-only recurrence (n = 10), and all other patterns of recurrence (n = 23). The corresponding 5-year postrecurrence survival were 60, 0, 18, and 5 %, respectively, p < 0.0001 in favor of patient with lung-only recurrence treated with repeated PM (Fig. 3).
There was no statistically significant difference in postrecurrence survival for patients with liver-only recurrence treated with repeated liver resection (n = 5) and those treated with chemotherapy (n = 5); 5-year postrecurrence survival rates were 25 and 0 %, respectively, p = 0.79.
Discussion
The current meta-analysis, which is based on individual patient data and includes the largest series of patients with CRC who had undergone PM in a background of previously resected liver metastasis, provides clear evidence that implementation of this surgical strategy is associated with the probability of long-term survival and a chance for cure. Additionally, this study provides basis for selection of candidates for PM in this patient population.
Recognition of the association of thoracic LN involvement with short RFS and OS has important practical implication. According to our data, status of thoracic LN provides solid basis for selecting patients for PM. In fact, the reported median OS and RFS for patients with thoracic LN involvement are almost comparable with the survival outcomes after systemic chemotherapy without PM.18–20 Therefore, preoperative assessment of the mediastinum through positron emission tomographic scan, and mediastinoscopy or endobronchial ultrasound biopsy for pathologic assessment of suspicious LN seems necessary to save patients with involved LN unnecessary and potentially morbid surgery. In addition, positron emission tomographic scan is a useful modality to exclude extrapulmonary metastasis before proceeding to PM.
Existing data from literature support the feasibility and efficacy of VATS surgery in resecting CRC pulmonary metastasis. Consistent with our data, Onaitis et al. did not find survival differences between VATS surgery and thoracotomy; however, VATS was associated with improved chest tube duration and hospital stay.7
High prethoracotomy CEA is predictive of poor survival after PM in series where the majority of subjects have lung-only metastasis.1,2,5,6,15,21 CEA level is predictive for survival in patients with unresectable and disseminated metastatic CRC as well.22 Data addressing the prognostic significance of CEA for patients who had undergone PM and had previously resected liver metastasis are scarce and conflicting. In a series of 43 patients with metastatic CRC and previously resected liver metastasis, Regnard et al. reported a correlation between serum CEA and survival.23 Headrick et al. reported similar findings.24 However, we did not identify such survival difference based on serum CEA; in fact, the OS of patients with serum CEA ≥5 ng/ml were exactly comparable with patients with values <5 ng/ml in our study (5-year OS = 53 % in each group). Consistent with our data, Nojiri et al. did not identify correlation between CEA and survival.25
The number of nodules and the DFI were not prognostic in our study as opposed to other studies where majority have lung-only metastasis.5,6,13,17 Contrary to our finding, other investigators found significant association between number of nodules and survival of patients with previous liver metastasis.25,26 Our data showed similar survival rates for patients with synchronous and metachronous liver and lung metastasis. In addition, Patients with simultaneously detected liver and lung metastasis had survival rates that are similar to patients whose lung metastasis developed later. Interestingly enough, one of the seven patients with simultaneously detected liver and lung metastasis is alive without evidence of disease at 127 months from PM. Consistent with our data, other authors did not identify any survival difference for patients with synchronous or metachronous liver–lung presentation.7,12,27
Although positive thoracic LN involvement is among the most consistently reported predictors of poor survival for PM in CRC, there is no uniform consensus about the necessity for preoperative mediastinoscopy or intraoperative thoracic LN sampling.1,2,4–6,12,21,24 In a survey of the opinions and beliefs of members of the European Society of Thoracic Surgeons (ESTS), although 65 % considered pathologically involved thoracic LN a contraindication to PM, a similar number rarely perform mediastinoscopy before PM; furthermore, 55 % reported that they perform routine mediastinal LN sampling, whereas 33 % perform no nodal dissection.28
Although intraoperative LN sampling adds important prognostic information, we emphasize that such an approach was never shown to be associated with therapeutic or survival advantage. However, this approach identifies the subgroup that is expected to do poorly after surgery, may suggest the need for additional chemotherapy for those with involved LN, and may provide basis for prognostic stratification. Therefore, we propose that intraoperative LN sampling should be included in the design of any future trial that intends to investigate efficacy of adjuvant therapies after PM in CRC.
We could not identify any benefit from adjuvant chemotherapy in this analysis; however, we emphasize that these data must be interpreted with caution, as information regarding the exact type of chemotherapy regimens was missing for significant proportion of patients. In addition, most of the patients in this analysis were treated in an era when modern oxaliplatin and Irinotecan based chemotherapy regimens were not utilized. Data supporting the benefit from perioperative chemotherapy are more clear for patients who are treated with hepatic metastasectomy; in that setting, chemotherapy improved disease-free survival.29
Consistent with our data, Shah et al. reported that 50 % of the recurrences in patients with CRC who are treated with PM and had prior liver resection are limited to lungs.27 However, our analysis provided formal investigation of the influence of patterns of recurrence on postrecurrence survival and suggested that continuing surveillance to detect the patients who develop isolated lung recurrence may have an impact on the outcomes, as repeated PM is associated with long-term postrecurrence survival.
Beside the limitation of assessing chemotherapy, we acknowledge other important limitations. First, data on operative morbidity were absent; second, quality of life could not be reported in this study as a result of its retrospective design; third, long-term consequences after PM such as requirement of home oxygen, postthoracotomy pain syndrome, and the ability to tolerate exercise were not reported as a result of missing data.
In conclusion, PM is associated with improved survival and the probability of cure in selected CRC patients with previously resected liver metastasis. Thoracic LN involvement is associated with poor outcome; therefore, preoperative staging of the mediastinum is necessary for patient selection, whereas intraoperative thoracic LN sampling is important for prognostic stratification.
References
Inoue M, Ohta M, Iuchi K, et al; Thoracic Surgery Study Group of Osaka University. Benefits of surgery for patients with pulmonary metastases from colorectal carcinoma. Ann Thorac Surg. 2004;78:238–44.
Saito Y, Omiya H, Kohno K, et al. Pulmonary metastasectomy for 165 patients with colorectal carcinoma: a prognostic assessment. J Thorac Cardiovasc Surg. 2002;124:1007–13.
Suemitsu R, Takeo S, Kusumoto E, et al. Results of a pulmonary metastasectomy in patients with colorectal cancer. Surg Today. 2011;41:54–9.
Welter S, Jacobs J, Krbek T, et al. Prognostic impact of lymph node involvement in pulmonary metastases from colorectal cancer. Eur J Cardiothorac Surg. 2007;31:167–72.
Gonzalez M, Poncet A, Combescure C, Robert J, Ris HB, Gervaz P. Risk factors for survival after lung metastasectomy in colorectal cancer patients: a systematic review and meta-analysis. Ann Surg Oncol. 2013;20:572–9.
Salah S, Watanabe K, Welter S, et al. Colorectal cancer pulmonary oligometastases: pooled analysis and construction of a clinical lung metastasectomy prognostic model. Ann Oncol. 2012;23:2649–55.
Onaitis MW, Petersen RP, Haney JC, et al. Prognostic factors for recurrence after pulmonary resection of colorectal cancer metastases. Ann Thorac Surg. 2009;87:1684–8.
Kim HK, Cho JH, Lee HY, Lee J, Kim J. Pulmonary metastasectomy for colorectal cancer: how many nodules, how many times? World J Gastroenterol. 2014;20:6133–45.
Simmonds PC, Primrose JN, Colquitt JL, Garden OJ, Poston GJ, Rees M. Surgical resection of hepatic metastases from colorectal cancer: a systematic review of published studies. Br J Cancer. 2006;94:982–99.
Landes U, Robert J, Perneger T, et al. Predicting survival after pulmonary metastasectomy for colorectal cancer: previous liver metastases matter. BMC Surg. 2010;10:17.
Gonzalez M, Robert JH, Halkic N, et al. Survival after lung metastasectomy in colorectal cancer patients with previously resected liver metastases. World J Surg. 2012;36:386–91.
Zabaleta J, Aguinagalde B, Fuentes MG, et al. Survival after lung metastasectomy for colorectal cancer: importance of previous liver metastasis as a prognostic factor. Eur J Surg Oncol. 2011;37:786–90.
Yedibela S, Klein P, Feuchter K, et al. Surgical management of pulmonary metastases from colorectal cancer in 153 patients. Ann Surg Oncol. 2006;13:1538–44.
Embún R, Fiorentino F, Treasure T, et al. Pulmonary metastasectomy in colorectal cancer: a prospective study of demography and clinical characteristics of 543 patients in the Spanish colorectal metastasectomy registry (GECMP-CCR). BMJ Open. 2013;3(5): e002787
Watanabe K, Nagai K, Kobayashi A, Sugito M, Saito N. Factors influencing survival after complete resection of pulmonary metastases from colorectal cancer. Br J Surg. 2009;96:1058–65.
Riquet M, Foucault C, Cazes A, et al. Pulmonary resection for metastases of colorectal adenocarcinoma. Ann Thorac Surg. 2010;89:375–80.
Borasio P, Gisabella M, Billé A, et al. Role of surgical resection in colorectal lung metastases: analysis of 137 patients. Int J Colorectal Dis. 2011;26:183–90.
Hurwitz H, Fehrenbacher L, Novotny W, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med. 2004;350:2335–42.
Hurwitz H. New combinations in metastatic colorectal cancer: what are our expectations? Oncologist. 2005;10:320–2.
Beretta GD, Petrelli F, Stinco S, et al. FOLFIRI + bevacizumab as second-line therapy for metastatic colorectal cancer pretreated with oxaliplatin: a pooled analysis of published trials. Med Oncol. 2013;30:486.
Iida T, Nomori H, Shiba M, et al. Prognostic factors after pulmonary metastasectomy for colorectal cancer and rationale for determining surgical indications: a retrospective analysis. Ann Surg. 2013;257:1059–64.
Hsu CW, King TM, Wang HT, Wang JH. Factors that influence survival in unresectable metastatic or locally advanced colorectal cancer. Int J Colorectal Dis. 2011;26:1559–66.
Regnard JF, Grunenwald D, Spaggiari L, et al. Surgical treatment of hepatic and pulmonary metastases from colorectal cancers. Ann Thorac Surg. 1998;66:214–8.
Headrick JR, Miller DL, Nagorney DM, et al. Surgical treatment of hepatic and pulmonary metastases from colon cancer. Ann Thorac Surg. 2001;71:975–9.
Nojiri K, Tanaka K, Nagano Y, et al. Efficacy of surgery for lung metastases from colorectal cancer synchronous to or following that for liver metastases. Anticancer Res. 2011;31:1049–54.
Kobayashi K, Kawamura M, Ishihara T. Surgical treatment for both pulmonary and hepatic metastases from colorectal cancer. J Thorac Cardiovasc Surg. 1999;118:1090–6.
Shah SA, Haddad R, Al-Sukhni W, et al. Surgical resection of hepatic and pulmonary metastases from colorectal carcinoma. J Am Coll Surg. 2006;202:468–75.
Internullo E, Cassivi SD, Van Raemdonck D, Friedel G, Treasure T. ESTS Pulmonary Metastasectomy Working Group. Pulmonary metastasectomy: a survey of current practice amongst members of the European Society of Thoracic Surgeons. J Thorac Oncol. 2008;3:1257–66.
Nordlinger B, Sorbye H, Glimelius B, et al. Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet. 2008;371(9617):1007–16.
Conflict of interest
Samer Salah, Francesco Ardissone, Michel Gonzalez, Pascal Gervaz, Marc Riquet, Kazuhiro Watanabe, Jon Zabaleta, Dalia Al-Rimawi, Samar Toubasi, Ehab Massad, Elena Lisi, and Osama H Hamed declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Salah, S., Ardissone, F., Gonzalez, M. et al. Pulmonary Metastasectomy in Colorectal Cancer Patients with Previously Resected Liver Metastasis: Pooled Analysis. Ann Surg Oncol 22, 1844–1850 (2015). https://doi.org/10.1245/s10434-014-4173-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-4173-9