Abstract
Purpose
The aim of this study was to investigate the prognostic significance of the response of primary rectal lesions to preoperative radiotherapy, pathological nodal status, and carcinoembryonic antigen (CEA) levels before and after radiotherapy in rectal cancer patients treated with a total mesorectal excision.
Methods
We investigated the prognostic significance of the clinical and pathological factors in 97 patients treated with preoperative radiotherapy (50–50.4 Gy over 5–6 weeks) followed by curative resections.
Results
A high CEA level (>5 ng/mL) after radiotherapy (hazard ratio, 2.849; 95% confidence interval, 1.061–7.651; p = 0.0377) and pathological lymph node metastasis (hazard ratio, 0.350; 95% confidence interval, 0.154–0.797; p = 0.0124) were independently associated with postoperative recurrence. Although the CEA level before radiotherapy was associated with disease-free survival in a univariate analysis, it lost its statistical significance in a multivariate analysis. The response of the primary rectal lesions, evaluated pathologically by T stage and the degree of regression, was not associated with disease-free survival. In patients without lymph node metastasis, the 5-year disease-free survival of those with a high CEA level after radiotherapy was significantly worse than those with low CEA after radiotherapy (61.6% vs. 89.0%, respectively, p = 0.0234).
Conclusions
Pathological lymph node metastasis and a high CEA level after radiotherapy were independent predictors of a poor outcome in rectal cancer patients treated with preoperative radiotherapy. The CEA level after radiotherapy was capable of discriminating patients with a high risk of recurrence among pathologically node-negative patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preoperative radiotherapy and total mesorectal excision (TME) have been shown to improve local control and possibly survival after the curative resection of rectal cancer [1–11], and these procedures have been incorporated into the standard practice for patients with rectal cancer. Recently, we reported a 5-year disease-free survival rate of more than 75% after TME for advanced rectal cancer following preoperative radiotherapy [12]. To further improve postoperative outcome, the identification of a patient subgroup with a poor prognosis that may require adjuvant therapy is important. Prognostic factors after surgery for colorectal cancers have been well documented [13]; however, some of the clinical and pathological features, such as the depth of transmural invasion, lymph node metastasis, and tumor marker levels, can be altered in response to preoperative therapy; thus, the prognostic factors of rectal cancers treated with preoperative radiotherapy must be discussed separately from those treated without neoadjuvant therapy.
Preoperative radiotherapy is considered to improve the oncological outcome by reducing both the primary rectal lesion and pelvic lymph node metastasis, if present [8]. The transmural depth of the primary lesion (T stage) is a proven prognostic factor for colorectal cancers [13]. Some of the patients treated with preoperative radiotherapy show down-staging in T stage. However, the responses of primary rectal lesions to preoperative radiotherapy vary among patients; some show almost no response, while others exhibit a complete pathological response. Whether the responses of primary rectal lesions to preoperative radiotherapy are correlated with postoperative recurrence or survival remains controversial [14–17]. Lymph node metastasis is also one of the most important prognostic factors after the curative resection of rectal cancer [13] and is also associated with postoperative recurrence, including distant metastasis, following preoperative radiotherapy [18, 19]. Preoperative radiotherapy has been shown to sterilize the lymphatic spread of rectal cancer [20, 21]. Thus, patients who have been pathologically diagnosed as node-negative after preoperative radiotherapy might include those who originally had lymph node metastasis that subsequently disappeared after preoperative radiotherapy. Therefore, pathological nodal status after resection following preoperative radiotherapy might underscore the risk of postoperative recurrence in such patients. The preoperative serum carcinoembryonic antigen (CEA) level is another definitive prognostic factor after the resection of rectal cancers [13], including those treated with preoperative radiotherapy [22, 23]. Throughout the course of preoperative radiotherapy, the CEA level can change: in some cases, the CEA level decreases in accordance with the reduction of the primary rectal lesion or pelvic lymph node metastasis; in other cases, the CEA level increases. Therefore, the CEA levels before and after preoperative radiotherapy can reflect the cancer status in response to preoperative radiotherapy. In this study, we investigated the prognostic significance of the response of primary rectal lesions, evaluated by pathological T stage and the degree of histologic regression, pathological nodal status, and the CEA levels before and after radiotherapy in rectal cancer patients treated with TME following preoperative radiotherapy.
Materials and methods
Patients
A total of consecutive 97 patients with locally advanced rectal cancer who underwent curative resections following neoadjuvant preoperative radiotherapy between 1993 and 2006 were studied retrospectively. The indication criteria for preoperative radiotherapy were as follows: (1) rectal cancer involving the lower third of the rectum (below the peritoneal reflection), (2) no distant metastasis (M−), and (3) a tumor depth beyond the muscularis propria (clinical T3 and T4). Preoperative staging was performed by digital examination, colonoscopy, endorectal ultrasound, barium enema, computed tomography (CT), and magnetic resonance imaging. Tumors were defined as involving the lower third of the rectum when the anal border of the tumor was distal to the second valve of Huston, which Corman described as almost corresponding to the peritoneal reflection [24]. Distance between the distal tumor margin and anocutaneous verge was also measured. Median (range) follow-up period was 39.9 (0.9–106.6) months.
Radiation methods
All the patients received pelvic preoperative radiotherapy as described previously [12]. Neoadjuvant chemotherapy, which we employed in practice in 2006, was not done concomitantly in this study period. The total dose of preoperative radiotherapy was 50 or 50.4 Gy, which was given in a fractionated and long-course fashion (2 Gy × 25 Fr over 5 weeks or 1.8 Gy × 28 Fr over 6 weeks, respectively). Treatment planning was done using CT scans, and the clinical target volume included the primary tumor, anus, and regional lymph nodes. The regional lymph nodes included the nodes around the inferior mesenteric, internal iliac and middle rectal vessels, the presacral nodes, and the nodes around the obturator foramen.
Surgical method
After the completion of preoperative radiotherapy, curative-intent operations were performed. Median (range) interval between the completion of radiotherapy and the operation was 34 (15–144) days. The surgical procedures consisted of a low anterior resection, abdominoperineal resection, Hartmann operation, and total pelvic exenteration. All the procedures included a lymphadenectomy utilizing a standard TME technique for dissecting the perirectal lymph nodes and lymph nodes along the superior rectal artery.
Pathological study
All the resected specimens were examined pathologically, and the findings were recorded in accordance with the tumor–node–metastases (TNM) classification [25]. In addition to the pathological T stage (ypT stage), the response of the primary rectal lesion to radiotherapy was evaluated also by the degree of histologic regression of cancer and was classified as either a high responder (Hi-R) or a low responder (Lo-R). Cases in which more than two thirds of the cancer had degraded, necrotized, or disappeared pathologically were classified as Hi-R, while the remaining cases were classified as Lo-R according to the classification of the Japanese Society for Cancer of the Colon and Rectum [26].
Serum CEA level
Serum CEA level was measured preoperatively both prior to (Pre-Rad CEA) and after (Post-Rad CEA) the completion of radiotherapy. The cutoff value is 5.0 ng/mL in our laboratory, and CEA levels exceeding this value were classified as high CEA, while those below this value were classified as low CEA.
Statistical analysis
Disease-free survival curves were created using the Kaplan–Meier method and were compared using the log-rank test. Univariate and multivariate analysis for factors associated with disease-free survival was performed using the Cox proportional hazard model. In a multivariate analysis, factors with p values less than 0.2 in a univariate analysis were analyzed. Paired t test, chi-square test, and Fisher's exact test were also performed where indicated. p values less than 0.05 were considered to denote statistical significance.
Results
Clinical and pathological features and disease-free survival
Table 1 shows the clinical and pathological features of the patients. Male patients were dominant (72.2%), and the median (range) age of the patient was 64 (29–82) years. The median (range) distance between the distal tumor margin and anocutaneous verge was 4 (0–8) cm. Clinical T stage before radiotherapy was T4 in two patients and T3 in the other. Postoperative recurrence, including local and distant recurrence, was seen in 22 patients, and cumulative 5-year recurrence rate was 27.4%. Local recurrence was seen in one patient, and the other recurrences were distant metastasis (liver, 11 patients; lung, 11 patients; bone, 2 patients; lymph node, 1 patient; skin, 1 patient). Table 2 shows the associations of clinical and pathological features with postoperative disease-free survival analyzed using the Kaplan–Meier method and the Cox hazard model (univariate analysis). Age, gender, and histologic type were not correlated with disease-free survival. Range of interval between the completion of radiotherapy and the operation was mainly due to patient reasons. No significant difference was seen in disease-free survival rates of the patients with shorter (≤33 days) interval and those with longer (≥34 days) interval.
Response of the primary rectal lesions
We evaluated the response of the primary rectal lesions to preoperative radiotherapy according to ypT stage and the degree of histologic regression (Hi-R and Lo-R). Stage ypT0-2, which was considered as down-staging because this study included cT3-4 before radiotherapy, was seen in 36 patients (37.1%). Stage ypT0, meaning a complete pathological response to preoperative radiotherapy, was seen in six patients (6.2%). Hi-R, including the six complete response cases, comprised 23 patients (23.7%). The 5-year disease-free survival rate was not statistically different between the patients with ypT0-2 and those with ypT3-4 (72.0% vs. 69.6%, respectively, p = 0.6984) or between Hi-R and Lo-R (67.7% vs. 71.4%, respectively, p = 0.8514). Thus, the response of the primary rectal lesion, determined by ypT stage or the degree of histologic regression, was not significantly correlated with disease-free survival. In this series, local recurrence was seen in only one patient with ypT3, a Lo-R patient, and all other recurrences were distant metastases.
Pathological nodal status
Median (range) of the number of harvested and examined lymph node was 13 (1–68). Pathological lymph node metastasis was seen in 32 patients (33.0%); 29 patients were ypN1, and 3 patients were ypN2. When analyzed according to the degree of histologic regression of the primary lesion, lymph node metastasis was less frequently observed in Hi-R (18.1%) than in Lo-R (36.0%); however, the difference was not statistically significant (p = 0.115). None of the patients who showed a complete response had lymph node metastasis. The 5-year disease-free survival rate was 80.6% in patients without lymph node metastasis, which was significantly better than the 5-year disease-free survival rate of 51.3% seen in patients with lymph node metastasis (p = 0.0029). The 5-year disease-free survival rate of the patients with less than 13 harvested lymph nodes was worse (63.8% vs. 75.6%); however, the difference was not statistically significant (p = 0.3301).
Serum CEA level
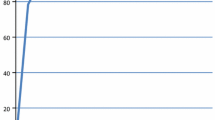
The median (range) Pre-Rad CEA level was 5.7 (1.1–201.3) ng/mL, while the median (range) Post-Rad CEA level was 3.8 (0.7–39.2) ng/mL (p = 0.0005). The Pre-Rad CEA level was high in 52 patients (53.6%), and the Post-Rad CEA level was high in 34 patients (35.1%); this difference was statistically significant (p = 0.0093). The Post-Rad/Pre-Rad CEA ratio was less than 1, which indicates decline in CEA level in response to radiotherapy, in 76 patients (78.3%). Both a high Pre-Rad CEA level and a high Post-Rad CEA level were significantly correlated with poor disease-free survival (p = 0.0331 and p = 0.0021, respectively, Fig. 1a, b). The Post-Rad/Pre-Rad CEA ratio was not significantly correlated with disease-free survival (p = 0.7656).
Disease-free survival curves according to CEA level before preoperative radiotherapy (a) and CEA level after preoperative radiotherapy (b). High Pre-Rad (Post-Rad) CEA patients with CEA > 5 ng/mL before (after) radiotherapy; Low Pre-Rad (Post-Rad) CEA patients with CEA ≤ 5 ng/mL before (after) radiotherapy
Multivariate analysis
In the multivariate analysis of clinicopathological features with p values less than 0.2 in a univariate analysis, pathological lymph node metastasis (p = 0.0124) and a high Post-Rad CEA level (p = 0.0377) were independently associated with poor disease-free survival (Table 3). Although both the Pre-Rad CEA level and the Post-Rad CEA level were significantly associated with disease-free survival in a univariate analysis, the Pre-Rad CEA level lost its statistical significance (p = 0.685) in the multivariate analysis. Furthermore, among patients with a low Post-Rad CEA level, patients with a high Pre-Rad CEA level (n = 23) and those with a low Pre-Rad CEA level (n = 41) had comparably fair 5-year disease-free survival rates (81.0% vs. 82.3%, respectively, p = 0.6014, Fig. 2). Thus, for patients with a low Post-Rad CEA level, the previous Pre-Rad CEA level is of little significance.
Disease-free survival curves of the patients with low CEA level after radiotherapy according to CEA level before radiotherapy. High Pre-Rad → Low Post-Rad CEA, patients with CEA > 5 ng/mL before radiotherapy and CEA ≤ 5 ng/mL after radiotherapy. Low Pre-Rad → Low Post-Rad CEA, patients with CEA ≤ 5 ng/mL before and after radiotherapy
Significance of Post-Rad CEA level in node-negative patients
To further examine the prognostic significance of the Post-Rad CEA level, we performed a combined analysis of nodal status and the Post-Rad CEA level, both of which were selected as independent prognostic factors in the multivariate analysis. Figure 3 shows the disease-free survival curves of the patient subgroups stratified according to the combination of pathological nodal status and Post-Rad CEA level. The 5-year disease-free survival of the patients with a high Post-Rad CEA level was significantly worse than that of the patients with a low Post-Rad CEA level among node-negative patients (61.6% vs. 89.0%, respectively, p = 0.0234), and it approximated the disease-free survival of patients with lymph node metastasis (51.3%). Thus, the Post-Rad CEA level was able to discriminate a patient subgroup with a worse prognosis among pathologically node-negative patients.
Disease-free survival curves according to pathological nodal status and CEA level after preoperative radiotherapy. ypN-/High Post-Rad CEA, node-negative patients with CEA > 5 ng/mL after radiotherapy. ypN-/Low Post-Rad CEA, node-negative patients with CEA ≤ 5 ng/mL after radiotherapy. ypN+, node-positive patients. * ypN-/High Post-Rad CEA vs. ypN-/Low Post-Rad CEA
Discussion
In this study, we separately analyzed the prognostic significance of CEA levels before and after radiotherapy and found that the Post-Rad CEA level was an independent prognostic factor in a multivariate analysis but that the Pre-Rad CEA level was not. The preoperative serum CEA level has been shown to be a prognostic factor after the curative resection of colorectal cancer [13, 27], and the preoperative CEA level, prior to radiotherapy, has also been shown to be of prognostic significance for rectal patients treated with preoperative radiotherapy [22]. However, few studies have focused on the change in CEA levels throughout the course of treatment, including surgery and radiotherapy. Concerning the CEA levels before and after resection of rectal cancer, Park et al. reported that the consistently high CEA level was a risk factor for systemic recurrences [28], and Kim et al. showed that clearance pattern of CEA after surgery was well correlated with patient survival [29]. Recently, Larsen et al. reported that the CEA response to preoperative radiotherapy was a predictor of postoperative local recurrence [30]. They showed that the local recurrence rate of the patients with a reduced CEA level was better than those with a consistently high CEA level and as good as those with a consistently normal CEA level. In their study, the change in the CEA levels was not of prognostic significance for overall survival. Our results match well with recent reports concerning the CEA levels before and after preoperative chemoradiotherapy [31, 32]. Perez et al. showed that a normal CEA level after preoperative chemoradiotherapy was associated with improved overall and disease-free survival [31]. In addition, they showed that reduction in CEA level was not correlated with survival, which is also in accordance with our results. Therefore, not reduction in CEA level but reduction to normal (below the cutoff value) level seems to predict improved survival. The patients with a high Pre-Rad CEA level that then decreased to a normal level after radiotherapy showed an equally fair disease-free survival compared with the patients that consistently exhibited a low CEA level before and after radiotherapy. It was speculated that a high CEA level that subsequently normalized after preoperative radiotherapy or after surgery might indicate localized disease that was controlled by pelvic radiotherapy or completely removed by surgery, whereas a consistently high CEA level after radiotherapy or surgery might indicate the presence of systemic disease which keeps a serum CEA level high despite control or removal of the primary rectal lesion.
Lymph node metastasis after a curative resection for colorectal cancer is a well-documented prognostic factor, and patients with lymph node metastasis are recommended to undergo postoperative adjuvant chemotherapy to reduce the risk of recurrence [13, 33, 34]. In patients treated with preoperative chemoradiotherapy, lymph node metastasis also has been shown to be the most important prognostic factor [35, 36]. In the present study as well, nodal status after preoperative radiotherapy was a significant prognostic factor. However, in patients who received preoperative radiotherapy for rectal cancer, regional lymph node metastasis disappeared in some patients, resulting in a down-staging of the N stage [2, 21]. Therefore, patients with lymph node metastasis prior to preoperative radiotherapy that subsequently disappears after radiotherapy would be classified as pathologically node-negative after surgery, and the risk of postoperative recurrence, especially in the distant area outside the radiation field, might be underrated. Such high-risk patients should be discriminated from among pathologically node-negative patients treated with preoperative radiotherapy, and postoperative adjuvant chemotherapy should be considered for such patients. In an attempt to select a high-risk subgroup in patients without pathological lymph node metastasis, we performed a combined analysis of nodal status and Post-Rad CEA level, both of which were independent prognostic factors in a multivariate analysis. As shown in Fig. 3, patients with a high Post-Rad CEA level comprised a subgroup with a high risk of recurrence among pathologically node-negative patients. Therefore, the Post-Rad CEA level may serve as an indicator of a high risk of recurrence among pathologically node-negative patients and might be useful for adjusting the risk stratification according to the standard TNM classification in patients treated with radiotherapy followed by TME.
In this study, disease-free survival was not associated with either pathological T stage or the degree of histologic regression of rectal cancer. Local recurrence after resection was observed only in one patient, who showed a poor response to preoperative radiotherapy, and the majority of recurrences were distant metastases, such as liver and lung metastases. Therefore, preoperative radiotherapy followed by TME was considered to reduce local recurrence irrespective of the response of the primary rectal lesions; however, preoperative radiotherapy did not have therapeutic effect on distant metastasis at sites outside the radiation field. The response of the primary lesion to preoperative radiotherapy is not considered to predict recurrence in settings where the majority of recurrences are distant metastases. Recently, the addition of chemotherapy to preoperative radiotherapy (chemoradiotherapy) has been shown to further improve local control after the curative resection of rectal cancer [37]; however, the additional effects of chemotherapy on postoperative recurrence at distant sites remains undetermined. Thus, future study regarding whether the degree of response to chemoradiotherapy is associated with postoperative survival is necessary.
In conclusion, disease-free survival was not correlated with the down-staging of the T stage or the degree of histologic regression of the primary rectal lesion following preoperative radiotherapy. Pathological lymph node metastasis and the Post-Rad CEA level, but not the Pre-Rad CEA level, were independent predictors of a poor prognosis after TME for rectal cancer. The Post-Rad CEA level was capable of discriminating a subgroup with a high risk of recurrence among pathologically node-negative patients, and thus the Post-Rad CEA level might compensate pathological TNM stage in risk stratification for appropriate postoperative surveillance and adjuvant therapy of rectal cancer patients treated with preoperative radiotherapy.
References
Stockholm Rectal Cancer Study Group (1990) Preoperative short-term radiation therapy in operable rectal carcinoma. A prospective randomized trial. Cancer 66:49–55
Swedish Rectal Cancer Trial (1997) Improved survival with preoperative radiotherapy in resectable rectal cancer. N Engl J Med 336:980–987
Colorectal Cancer Collaborative Group (2001) Adjuvant radiotherapy for rectal cancer: a systematic overview of 8,507 patients from 22 randomised trials. Lancet 358:1291–1304
Gerard A, Buyse M, Nordlinger B et al (1988) Preoperative radiotherapy as adjuvant treatment in rectal cancer. Final results of a randomized study of the European Organization for Research and Treatment of Cancer (EORTC). Ann Surg 208:606–614
Kapiteijn E, Kranenbarg EK, Steup WH et al (1999) Total mesorectal excision (TME) with or without preoperative radiotherapy in the treatment of primary rectal cancer. Prospective randomised trial with standard operative and histopathological techniques. Dutch colorectal cancer group. Eur J Surg 165:410–420
Mendenhall WM, Million RR, Bland KI et al (1985) Preoperative radiation therapy for clinically resectable adenocarcinoma of the rectum. Ann Surg 202:215–222
Myerson RJ, Genovesi D, Lockett MA et al (1999) Five fractions of preoperative radiotherapy for selected cases of rectal carcinoma: long-term tumor control and tolerance to treatment. Int J Radiat Oncol Biol Phys 43:537–543
Nagawa H, Muto T, Sunouchi K et al (2001) Randomized, controlled trial of lateral node dissection vs. nerve-preserving resection in patients with rectal cancer after preoperative radiotherapy. Dis Colon Rectum 44:1274–1280
Watanabe T, Tsurita G, Muto T et al (2002) Extended lymphadenectomy and preoperative radiotherapy for lower rectal cancers. Surgery 132:27–33
Folkesson J, Birgisson H, Pahlman L et al (2005) Swedish rectal cancer trial: long lasting benefits from radiotherapy on survival and local recurrence rate. J Clin Oncol 23:5644–5650
Heald RJ, Ryall RD (1986) Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1:1479–1482
Kiyomatsu T, Watanabe T, Muto T et al (2007) The 4-portal technique decreases adverse effects in preoperative radiotherapy for advanced rectal cancer: comparison between the 2-portal and the 4-portal techniques. Am J Surg 194:542–548
Compton CC, Fielding LP, Burgart LJ et al (2000) Prognostic factors in colorectal cancer. College of American pathologists consensus statement 1999. Arch Pathol Lab Med 124:979–994
Pucciarelli S, Toppan P, Friso ML et al (2004) Complete pathologic response following preoperative chemoradiation therapy for middle to lower rectal cancer is not a prognostic factor for a better outcome. Dis Colon Rectum 47:1798–1807
Suarez J, Vera R, Balen E et al (2008) Pathologic response assessed by Mandard grade is a better prognostic factor than down staging for disease-free survival after preoperative radiochemotherapy for advanced rectal cancer. Colorectal Dis 10:563–568
Tsujinaka S, Kawamura YJ, Konishi F et al (2008) Long-term efficacy of preoperative radiotherapy for locally advanced low rectal cancer. Int J Colorectal Dis 23:67–76
Beddy D, Hyland JM, Winter DC et al (2008) A simplified tumor regression grade correlates with survival in locally advanced rectal carcinoma treated with neoadjuvant chemoradiotherapy. Ann Surg Oncol 15:3471–3477
Bujko K, Michalski W, Kepka L et al (2007) Association between pathologic response in metastatic lymph nodes after preoperative chemoradiotherapy and risk of distant metastases in rectal cancer: an analysis of outcomes in a randomized trial. Int J Radiat Oncol Biol Phys 67:369–377
Chapet O, Romestaing P, Mornex F et al (2005) Preoperative radiotherapy for rectal adenocarcinoma: which are strong prognostic factors? Int J Radiat Oncol Biol Phys 61:1371–1377
Leibold T, Shia J, Ruo L et al (2008) Prognostic implications of the distribution of lymph node metastases in rectal cancer after neoadjuvant chemoradiotherapy. J Clin Oncol 26:2106–2111
Swedish Rectal Cancer Trial (1993) Initial report from a Swedish multicentre study examining the role of preoperative irradiation in the treatment of patients with resectable rectal carcinoma. Br J Surg 80:1333–1336. doi:1333
Peng JJ, Cai SJ, Lu HF et al (2007) Predicting prognosis of rectal cancer patients with total mesorectal excision using molecular markers. World J Gastroenterol 13:3009–3015
Das P, Skibber JM, Rodriguez-Bigas MA et al (2007) Predictors of tumor response and downstaging in patients who receive preoperative chemoradiation for rectal cancer. Cancer 109:1750–1755
Corman O (1998) Colon and rectal surgery, 4th edn. Lippincott Williams, Philadelphia
Sobin L, Wittekind C (2002) TNM classification of malignant tumours. Springer, New York
Japanese Society for Cancer of the Colon and Rectum (2006) General rules for clinical and pathological studies on cancer of the colon, rectum and anus, 7th edn. Kanehara, Tokyo
Takahashi T, Kato T, Kodaira S et al (1996) Prognostic factors of colorectal cancer. Results of multivariate analysis of curative resection cases with or without adjuvant chemotherapy. Am J Clin Oncol 19:408–415
Park YA, Lee KY, Kim NK et al (2006) Prognostic effect of perioperative change of serum carcinoembryonic antigen level: a useful tool for detection of systemic recurrence in rectal cancer. Ann Surg Oncol 13:645–650
Kim JY, Kim NK, Sohn SK et al (2009) Prognostic value of postoperative CEA clearance in rectal cancer patients with high preoperative CEA levels. Ann Surg Oncol 16:2771–2778
Larsen SG, Wiig JN, Dueland S et al (2008) Prognostic factors after preoperative irradiation and surgery for locally advanced rectal cancer. Eur J Surg Oncol 34:410–417
Perez RO, Sao Juliao GP, Habr-Gama A et al (2009) The role of carcinoembriogenic antigen in predicting response and survival to neoadjuvant chemoradiotherapy for distal rectal cancer. Dis Colon Rectum 52:1137–1143
Park JW, Lim SB, Kim DY et al (2009) Carcinoembryonic antigen as a predictor of pathologic response and a prognostic factor in locally advanced rectal cancer patients treated with preoperative chemoradiotherapy and surgery. Int J Radiat Oncol Biol Phys 74:810–817
Akasu T, Moriya Y, Ohashi Y et al (2006) Adjuvant chemotherapy with uracil-tegafur for pathological stage III rectal cancer after mesorectal excision with selective lateral pelvic lymphadenectomy: a multicenter randomized controlled trial. Jpn J Clin Oncol 36:237–244
Hisashige A, Yoshida S, Kodaira S (2008) Cost-effectiveness of adjuvant chemotherapy with uracil-tegafur for curatively resected stage III rectal cancer. Br J Cancer 99:1232–1238
Fietkau R, Barten M, Klautke G et al (2006) Postoperative chemotherapy may not be necessary for patients with ypN0-category after neoadjuvant chemoradiotherapy of rectal cancer. Dis Colon Rectum 49:1284–1292
Rodel C, Martus P, Papadoupolos T et al (2005) Prognostic significance of tumor regression after preoperative chemoradiotherapy for rectal cancer. J Clin Oncol 23:8688–8696
Wong RK, Tandan V, De Silva S et al (2007) Pre-operative radiotherapy and curative surgery for the management of localized rectal carcinoma. Cochrane Database Syst Rev. doi:10.1002/14651858, CD002102
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ishihara, S., Watanabe, T., Kiyomatsu, T. et al. Prognostic significance of response to preoperative radiotherapy, lymph node metastasis, and CEA level in patients undergoing total mesorectal excision of rectal cancer. Int J Colorectal Dis 25, 1417–1425 (2010). https://doi.org/10.1007/s00384-010-1051-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-010-1051-1