Abstract
Introduction
Perforated colorectal malignancy is associated with numerous peri-operative complications and dismal long-term survival. The study aimed to review the outcome and factors predicting peri-operative complications and long-term survival of patients who underwent surgery for perforated colorectal malignancy.
Methods
A retrospective review of all patients who underwent operative intervention for perforated colorectal malignancy from February 2003 to April 2008 was performed. The severity of peritonitis was graded using the Mannheim peritonitis index (MPI).
Results
Forty-five patients, median age 67 years (36–97 years), formed the study group. Sigmoid colon (37.8%) and cecum (28.9%) were the most common sites of perforation. Sixteen (35.6%) patients had stage IV disease, while 14 (31.1%) had severe peritoneal contamination (MPI > 26). Hartmann’s procedure and right hemicolectomy were performed most frequently in 17 (37.8%) and 15 (33.4%) patients, respectively. The mortality rate in our series was 17.8%, with another 26.7% requiring surgical intensive care unit care. The independent variables predicting worse peri-operative complications were American Society of Anesthesiologists (ASA) score ≥3 and MPI >26. Left-sided perforation was the only independent factor predicting stoma creation. The only factor predicting long-term survival was the stage of malignancy (p < 0.001). The overall mean survival time for stage II, III, and IV disease were 63.7, 38.1, and 13.8 months, respectively.
Conclusions
Surgery for perforated colorectal malignancy is associated with high morbidity and mortality rates. Short-term outcome is determined by ASA score and severity of peritonitis, while long-term outcome is determined by staging of the cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Perforation from colorectal malignancy is a surgical emergency fraught with numerous challenges. Not only do the surgeons have to tackle the peritoneal contamination, they also have to deal with the primary malignancy [1, 2]. In addition, the long-term prognosis in these patients has been regarded as abysmal due to the advanced malignancy and the possibility of tumor seeding through the perforation site [1, 2].
The operative mortality and morbidity rates in these patients remain prohibitive despite advances in surgical techniques and peri-operative care [3, 4]. Fortunately, the reported incidences of perforated colorectal cancers remain low [5, 6]. As a result, large series analyzing the peri-operative and long-term outcome in these patients are lacking.
In view of all the above issues, we undertook this study with the primary aim to review the treatment and early outcome of patients with perforated colorectal malignancy who underwent emergency surgery. Our secondary aims were to evaluate the various factors predicting peri-operative morbidity and mortality, as well as to document the long-term outcome in these patients.
Methods
Study population
Tan Tock Seng Hospital is a 1,300-bed hospital, the second largest in Singapore, that provides secondary and tertiary medical care for about 1.5 million people. A retrospective review of all patients who underwent operative intervention for peritonitis from perforated colorectal malignancy from February 2003 to April 2008 was performed. Patients were identified from the hospital’s diagnostic index and operating records, while patients who had intraoperative perforations were excluded. Right-sided pathologies were regarded if it was located from the cecum till the transverse colon while left-sided pathologies commenced from the splenic flexure. All malignancies were confirmed upon histological evaluation.
The data collected included age, gender, ASA (American Society of Anesthesiologists) score, and co-morbid conditions. Laboratory values, including full blood count and renal panel, were also recorded. In addition, operative findings and interventions, length of surgery, peri-operative complications, mortality, and length of hospital stay were also documented.
Resection of the tumor would be attempted in all patients except in cases when the tumors were fixed to structures that are specific and not susceptible of resection, or in patients who were hemodynamically unstable. All gastrointestinal anastomoses were either hand-sewn or stapled, while the stoma created could either be a defunctioning or an end stoma.
The severity of abdominal sepsis for all patients was graded using the Mannheim peritonitis index (MPI) [7] (Table 1) with a score of >26 being defined as severe. All colorectal cancers were staged according to the guidelines of the American Joint Committee of Cancer [8]. The grades of complications (GOC) were in concordance to the classification proposed by Clavien and group [9–11] (Table 2).
Peri-operative mortality was defined as death that occurred within 1 month of the operation. Disease recurrence was confirmed through radiological or pathological evaluation. The overall survival duration was documented from the date of surgery until the date of death.
Statistical analysis was performed using both univariate and multivariate analyses. The variables were analyzed to the various outcomes using the Fisher’s exact test, and their odds ratio (OR) and 95% confidence interval (CI) were also reported. For the multivariate analysis, the logistic regression model was applied. The overall survival probability, excluding operative mortality, was estimated according to the Kaplan–Meier method. All analyses were performed using the SPSS 17.0 statistical package (Chicago, IL, USA) and all p values reported are two-sided; p values of < 0.05 were considered statistically significant.
Results
Study group
During the study period, 1,268 patients underwent colorectal cancer-related surgeries. In total, 45 (3.5%) patients were operated on for perforated colorectal malignancy and formed the study group. Six (13.3%) patients had known colorectal malignancy that declined earlier surgical intervention. The median age of the study group was 67 years (36–97 years), with a majority of the patients (n = 30, 66.7%) with an ASA score ≥3. Table 3 illustrates the various characteristics of the study group.
Operative findings and intervention
Sigmoid colon (n = 17, 37.8%) and cecum (n = 13, 28.9%) were the most common sites of perforation (Table 4). Perforation proximal to the tumor (diastatic perforation) was seen in 11 (24.4%) patients, while perforation at the tumor was seen in the remaining 34 (75.6%). Sixteen (35.6%) patients had stage IV disease during surgery. The median MPI was 21 (9–43) with 31.1% (n = 14) having severe peritoneal contamination (>26).
Hartmann’s procedure and right hemicolectomy were performed most frequently in 17 (37.8%) and 15 (33.4%) patients, respectively. In two (4.4%) patients, the primary malignancy was not removed as the rectal primary was deemed unresectable, and a defunctioning stoma at the proximal site of perforation was performed. Both already had metastatic disease and perished within 6 months from the surgery.
Outcome
In our series, eight (17.8%) patients died in the peri-operative period (Table 4). Another 12 (26.7%) required surgical intensive care unit (SICU) care. The median length of stay was 10 (2–54) days
Analysis—predictors of worse complications
After multivariate analysis, the independent variables predicting worse peri-operative complications (GOC III to V) were ASA score ≥3 and worse peritoneal contamination (MPI > 26) (Table 5).
Analysis—predictors of stoma creation
Stoma was created more often in patients with MPI >26 (p = 0.002), pre-operative renal impairment (OR 9.39, 95% CI 1.09–81.04, p = 0.034), and in those with left-sided perforation (OR 8.98, 95% CI 2.01–39.92, p = 0.003). After multivariate analysis, the site of perforation was the only independent factor associated with stoma creation.
Follow-up
Thirty seven (82.2%) patients survived surgery and were followed up for a median period of 25 months (3–73 months). One foreign patient was lost to follow-up as he returned to his home country for further treatment upon discharge.
In those patients who had stoma created, all the patients (n = 4) with defunctioning ileostomy had their stoma closed while only four patients who underwent Hartmann’s procedure had their stoma reversed. The median time from the initial surgery to the reversal of stoma was 11 months (range 3–21 months).
Of the 24 (53.3%) patients in whom the initial surgery was curative (stage II and III), 21 patients were followed up for more than 12 months. The remaining three perished within 1 year post-surgery. While adjuvant chemotherapy was advised for all patients, it was only administered in 12 patients. The chemotherapy regime was not standardized in our current series and was at the discretion of the oncologist. The remaining 12 patients did not undergo adjuvant chemotherapy due to personal reasons or was not advised due to advanced age or numerous co-morbid conditions.
A total of 10 (41.7%) patients had disease recurrence. The median time to recurrence was 13 months (6–48 months). Local recurrence was seen in five patients, while distant metastases were seen in all ten patients with the liver most commonly involved in eight patients. Not surprisingly, most of them (n = 9, 90.0%) had stage III disease initially. The only patient with stage II disease had recurrence only 48 months after the initial surgery. Factors such as site of perforation, diastatic perforation, age, gender, ASA score, and MPI were all not related to recurrence.
In the other group of patients with metastatic disease (n = 12), nine had unresectable metastases on presentation of which eight died within 1 year from surgery. The other patient perished 22 months after the surgery while only on palliative chemotherapy. In the three patients who had potentially resectable metastases, two underwent metastatectomy for hepatic (both patients) and pancreatic metastases. Apart from the surgery, they also received good response from the chemotherapy. Both of them are currently still alive at 28 and 36 months from the initial surgery. The last patient with resectable metastases did not undergo further surgery as the patient and family declined due to his advanced age and the numerous associated peri-operative risk factors. He died within 1 year from the initial surgery. Thus, in total, there were three (25.0%) patients with initial metastatic diseases who lived more than 18 months. Apart from these three patients, another two patients also had chemotherapy, but their response was suboptimal and they perished from their advanced malignancy eventually.
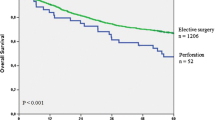
The overall mean survival time for stage II, III, and IV diseases were 63.7 months (95% CI 50.5–76.9 months), 38.1 months (median 26; 95% CI 24.7–51.5 months), and 13.8 months (median 10, 95% CI 7.4–20.3 months), respectively. The staging of the malignancy was the only factor associated with long-term survival (p < 0.001) (Fig. 1). Other factors such as age, gender, ASA score, MPI, site of perforation, and diastatic perforation were not related to survival.
Discussion
Our series affirmed the high peri-operative morbidity and mortality rates associated with perforated colorectal cancers [1–6, 12]. The mortality rate in our series was 17.8%, with another 26.7% requiring SICU stay post-operatively. Fortunately, the incidence of perforated colorectal cancer is rare and was less than 4% in our institution. These figures are similar to those quoted in other series [3, 6].
Numerous factors have been shown to be associated with worse peri-operative outcome. These include advanced age, renal failure, worse peritonitis, advanced malignancy, higher ASA grade, and metastatic disease [1, 3, 13]. In our series, the two independent factors that were related to worse outcome were higher ASA score and MPI >26. Even though there are several other scoring systems for surgical patients, MPI has been adopted by our institution to predict the peri-operative outcome in patients with peritonitis [14]. The ease of application and its high accuracy are some of the underlying explanations behind our current practice.
The relationship between the nature of perforation and patients’ outcome has been the subject of much debate in several series. Proximal perforation has been regarded by some to be associated with worse outcome and increased recurrence [1, 4, 5, 15]. They postulated that the resultant diffuse peritonitis from a proximal perforation compared to a more localized collection if the perforation is at the tumor site is responsible for the difference. However, several other series, including ours, have refuted this association [6, 13, 16]. Confirmation of any relationship between diastatic perforation and patients’ short- and long-term outcome would likely require a much larger series. But the rarity of this condition and its associated high peri-operative mortality rate will make this task challenging.
While the site of perforation was not associated with worse short- or long-term outcome, left-sided perforation was associated with a higher stoma rate in our series. There are several possible explanations for this trend. Firstly, colo-colic or colorectal anastomosis has always been associated with an increased risk of anastomotic dehiscence compared to ileo-colic anastomosis [17–19]. Furthermore, operating on these high-risk patients with significant peritoneal contamination naturally make Hartmann’s procedure or a defunctioning stoma after primary anastomosis an appealing option especially in left-sided perforation.
Unfortunately, the complications associated with a stoma are not negligible, and the low reversal rates of Hartmann’s procedures, also seen in our series, are just some of the considerations to deliberate intra-operatively [20–23]. Thus, some institutions advocated primary anastomosis after resection with or without proximal defunctioning stoma [24]. This obviates the need of a second operation or decreases the technical difficulties encountered during the closure of the stoma compared to a reversal of Hartmann’s procedure. This trend was also seen in our series with the successful closure of all the patients who had defunctioning ileostomy. However, in instances of obstructing left-sided malignancy with right-sided perforation, a more extensive resection such as subtotal or total colectomy is perhaps warranted [24].
Long-term survival in patients with perforated colorectal malignancy has always been regarded as abysmal compared to uncomplicated colorectal cancer [25–27]. However, some studies have reported similar long-term survival between the two groups, possibly disproving the notion of poorer prognosis from the perforation [4–6, 28]. But among patients with perforated colorectal malignancy, factors such as staging of malignancy, diastatic perforation, number of metastatic lymph nodes, and degree of histopathologic differentiation has been associated with worse outcome in several small series [2–5]. From our series, staging of the malignancy was the only and the most important factor associated with long-term survival.
Adjuvant chemotherapy has always been advocated in all patients with stage III colorectal malignancies, and this has been extended to patients with high-risk stage II disease over the past years [29, 30]. These risk factors would include patients with obstruction, perforation, inadequate lymph node sampling, lymphovascular invasion, or even T4 disease [29, 30]. Adjuvant therapy has been shown to improve the disease-free survival in these patients [29, 30]. The authors did not analyze the impact of adjuvant therapy as only half the population underwent adjuvant therapy and their treatment regime was not standardized.
The majority of our patients with stage IV malignancy perished from their illness within 12 months. But our series was able to highlight one trend that is likely to become more prominent in the near future. There were two patients with metastatic disease on presentation who survived more than 28 months post-surgery and are still alive currently. One patient even had two surgeries to remove a hepatic metastasis initially, and then a pancreatic metastasis subsequently when the disease recurred. The other patient had only hepatic metastasectomy. Both these patients highlighted the increasing role of metastasectomy in enhancing the long-term survival in selected patients with stage IV disease [31–34]. Performed in carefully selected patients, metastasectomy and other newer targeted therapies have been shown to improve long-term and disease-free survival [31–36].
Over the past two decades, hyperthermic intra-peritoneal chemotherapy with complete cytoreductive surgery has been shown to be highly successful in achieving better outcome in patients with carcinomatosis peritonei from appendiceal mucinous neoplasm [37]. Its role in colorectal cancers has been explored in recent years [38–40]. Long-term survival is possible if oncologic clearance is achieved [38–40]. However, the complications from this laborious procedure are not negligible and should not be attempted in all patients, especially those with extensive and widespread peritoneal disease [38–40].
There are considerable limitations in our study. This series of patients was enrolled from a single institution, and any retrospective study has inherent flaws. The sample size is extremely small and this may mask several other factors that could be accountable for the outcomes measured. In addition, we did not match the patients with identical cases with non-perforated colorectal malignancy as our focus was to highlight the various issues pertaining to perforated colorectal cancers. Furthermore, we were unable to comment on the impact of chemotherapy in our series due to the numerous limitations highlighted prior. The follow-up period is also not adequate for the authors to have a better understanding of the long-term impact of perforated colorectal malignancy in an Asian population. But through our study, we were able to highlight the numerous challenges in managing these patients, and we also attempted to identify several factors that were associated with worse peri-operative complications, long-term survival, and disease recurrence.
Conclusion
Surgery for perforated colorectal malignancy is associated with high morbidity and mortality rates. Short-term outcome is determined by ASA score and severity of peritonitis, while long-term outcome is determined by stage of the cancer. Long-term survival is possible in selected patients with perforated colorectal cancer and resectable metastases.
References
Carraro PG, Segala M, Orlotti C, Tiberio G (1998) Outcome of large-bowel perforation in patients with colorectal cancer. Dis Colon Rectum 41(11):1421–1426
Lee IK, Sung NY, Lee YS, Lee SC, Kang WK, Cho HM, Ahn CH, Lee do S, Oh ST, Kim JG, Jeon HM, Chang SK (2007) The survival rate and prognostic factors in 26 perforated colorectal cancer patients. Int J Colorectal Dis 22(5):467–473
Anwar MA, D’Souza F, Coulter R, Memon B, Khan IM, Memon MA (2006) Outcome of acutely perforated colorectal cancers: experience of a single district general hospital. Surg Oncol 15(2):91–96
Alvarez JA, Baldonedo RF, Bear IG, Truán N, Pire G, Alvarez P (2005) Presentation, treatment, and multivariate analysis of risk factors for obstructive and perforative colorectal carcinoma. Am J Surg 190(3):376–382
Chen HS, Sheen-Chen SM (2000) Obstruction and perforation in colorectal adenocarcinoma: an analysis of prognosis and current trends. Surgery 127(4):370–376
Mandava N, Kumar S, Pizzi WF, Aprile IJ (1996) Perforated colorectal carcinomas. Am J Surg 172(3):236–238
Billing A, Fröhlich D, Schildberg FW (1994) Prediction of outcome using the Mannheim peritonitis index in 2003 patients. Peritonitis Study Group. Br J Surg 81(2):209–213
Astler VB, Coller FA (1954) The prognostic significance of direct extension of carcinoma of the colon and rectum. Ann Surg 139(6):846–852
Clavien PA, Sanabria JR, Mentha G, Borst F, Buhler L, Roche B, Cywes R, Tibshirani R, Rohner A, Strasberg SM (1992) Recent results of elective open cholecystectomy in a North American and a European center. Comparison of complications and risk factors. Ann Surg 216(6):618–626
Clavien PA, Camargo CA Jr, Croxford R, Langer B, Levy GA, Greig PD (1994) Definition and classification of negative outcomes in solid organ transplantation. Application in liver transplantation. Ann Surg 220(2):109–120
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Kriwanek S, Armbruster C, Dittrich K, Beckerhinn P (1996) Perforated colorectal cancer. Dis Colon Rectum 39:1409–1414
Shinkawa H, Yasuhara H, Naka S, Yanagie H, Nojiri T, Furuya Y, Ariki K, Niwa H (2003) Factors affecting the early mortality of patients with nontraumatic colorectal perforation. Surg Today 33(1):13–17
Tan KK, Zhang J, Liu JZ, Shen SF, Earnest A, Sim R (2009) Right colonic perforation in an Asian population: predictors of morbidity and mortality. J Gastrointest Surg 13(12):2252–2259
Khan S, Pawlak SE, Eggenberger JC, Lee CS, Szilagy EJ, Margolin DA (2001) Acute colonic perforation associated with colorectal cancer. Am Surg 67(3):261–264
Welch JP, Donaldson GA (1974) Perforative carcinoma of colon and rectum. Ann Surg 180(5):734–740
Veyrie N, Ata T, Muscari F, Couchard AC, Msika S, Hay JM, Fingerhut A, Dziri C (2007) Anastomotic leakage after elective right versus left colectomy for cancer: prevalence and independent risk factors. J Am Coll Surg 205(6):785–793
Konishi T, Watanabe T, Kishimoto J, Nagawa H (2006) Risk factors for anastomotic leakage after surgery for colorectal cancer: results of prospective surveillance. J Am Coll Surg 202(3):439–444
Lipska MA, Bissett IP, Parry BR, Merrie AE (2006) Anastomotic leakage after lower gastrointestinal anastomosis: men are at a higher risk. ANZ J Surg 76(7):579–585
Duchesne JC, Wang YZ, Weintraub SL, Boyle M, Hunt JP (2002) Stoma complications: a multivariate analysis. Am Surg 68:961–966
Leong QM, Koh DC, Ho CK (2008) Emergency Hartmann’s procedure: morbidity, mortality and reversal rates among Asians. Tech Coloproctol 12(1):21–25
Arumugam PJ, Bevan L, Macdonald L, Watkins AJ, Morgan AR, Beynon J, Carr ND (2003) A prospective audit of stomas—analysis of risk factors and complications and their management. Colorectal Dis 5(1):49–52
David GG, Al-Sarira AA, Willmott S, Cade D, Corless DJ, Slavin JP (2009) Use of Hartmann’s procedure in England. Colorectal Dis 11(3):308–312
Tan KK, Sim R (2010) Surgery for obstructed colorectal malignancy in an Asian population: predictors of morbidity and comparison between left and right sided cancers. J Gastrointest Surg 14(2):295–302
Steinberg SM, Barkin JS, Kaplan RS, Stablein DM (1986) Prognostic indicators of colon tumors. The Gastrointestinal Tumor Study Group experience. Cancer 57(9):1866–1870
Runkel NS, Schlag P, Schwarz V et al (1991) Outcome after emergency surgery for cancer of the large intestine. Br J Surg 78:183–188
Griffin MR, Bergstralh EJ, Coffey RJ et al (1987) Predictors of survival after curative resection of carcinoma of the colon and rectum. Cancer 60:2318–2324
Kagda FH, Nyam DC, Ho YH, Eu KW, Leong AF, Seow-Choen F (1999) Surgery may be curative for patients with a localized perforation of rectal carcinoma. Br J Surg 86(11):1448–1450
Figueredo A, Coombes ME, Mukherjee S (2008) Adjuvant therapy for completely resected stage II colon cancer. Cochrane Database Syst Rev (3):CD005390
Figueredo A, Germond C, Maroun J, Browman G, Walker-Dilks C, Wong S (1997) Adjuvant therapy for stage II colon cancer after complete resection. Provincial Gastrointestinal Disease Site Group. Cancer Prev Control 1(5):379–392
Fahy BN, D’Angelica M, DeMatteo RP, Blumgart LH, Weiser MR, Ostrovnaya I, Gonen M, Jarnagin WR (2009) Synchronous hepatic metastases from colon cancer: changing treatment strategies and results of surgical intervention. Ann Surg Oncol 16(2):361–370
Shah SA, Haddad R, Al-Sukhni W, Kim RD, Greig PD, Grant DR, Taylor BR, Langer B, Gallinger S, Wei AC (2006) Surgical resection of hepatic and pulmonary metastases from colorectal carcinoma. J Am Coll Surg 202(3):468–475
Abdalla EK, Vauthey JN, Ellis LM, Ellis V, Pollock R, Broglio KR, Hess K, Curley SA (2004) Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Ann Surg 239(6):818–825
Scheele J, Stangl R, Altendorf-Hofmann A (1990) Hepatic metastases from colorectal carcinoma: impact of surgical resection on the natural history. Br J Surg 77(11):1241–1246
Kemeny MM, Adak S, Gray B, Macdonald JS, Smith T, Lipsitz S, Sigurdson ER, O’Dwyer PJ, Benson AB 3rd (2002) Combined-modality treatment for resectable metastatic colorectal carcinoma to the liver: surgical resection of hepatic metastases in combination with continuous infusion of chemotherapy—an intergroup study. J Clin Oncol 20(6):1499–1505
Adam R, Delvart V, Pascal G, Valeanu A, Castaing D, Azoulay D, Giacchetti S, Paule B, Kunstlinger F, Ghémard O, Levi F, Bismuth H (2004) Rescue surgery for unresectable colorectal liver metastases downstaged by chemotherapy: a model to predict long-term survival. Ann Surg 240(4):644–657
Sugarbaker PH (2006) New standard of care for appendiceal epithelial neoplasms and pseudomyxoma peritonei syndrome? Lancet Oncol 7(1):69–76
Yan TD, Black D, Savady R, Sugarbaker PH (2006) Systematic review on the efficacy of cytoreductive surgery combined with perioperative intraperitoneal chemotherapy for peritoneal carcinomatosis from colorectal carcinoma. J Clin Oncol 24(24):4011–4019
Verwaal VJ, Bruin S, Boot H, van Slooten G, van Tinteren H (2008) 8-year follow-up of randomized trial: cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy in patients with peritoneal carcinomatosis of colorectal cancer. Ann Surg Oncol 15(9):2426–2432
Verwaal VJ, Boot H, Aleman BM, van Tinteren H, Zoetmulder FA (2004) Recurrences after peritoneal carcinomatosis of colorectal origin treated by cytoreduction and hyperthermic intraperitoneal chemotherapy: location, treatment, and outcome. Ann Surg Oncol 11(4):375–379
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tan, KK., Hong, CC., Zhang, J. et al. Surgery for perforated colorectal malignancy in an Asian population: an institution’s experience over 5 years. Int J Colorectal Dis 25, 989–995 (2010). https://doi.org/10.1007/s00384-010-0945-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-010-0945-2