Abstract
Pilonidal sinus (PS) disease is a chronic inflammatory disease of the sacrococcygeal region. Although various methods have been described for surgical treatment, there is no consensus on the best surgical technique. The aim of this study was to present the results of a new advancement flap technique named the “Keystone flap (KSF)” and compared with the Limberg flap (LF) technique in pilonidal sinus surgery. A retrospective review was made of 124 consecutive patients surgically treated for PS disease with KSF and LF procedures. Baseline characteristics, operation time, volume of excised specimen, duration of hospitalization, duration of drainage, duration of healing, time to return to work, local complications and recurrence were evaluated and compared between the two procedures. Operation time, healing time, and time to return to work were significantly shorter in the KSF group. Partial wound dehiscense and prolonged wound healing were more common in the LF group. An additional intervention in the operating room was required by 21.1% of the LF group and was a significantly lower rate in the KSF group at 7.5%. There was no significant difference between the groups in terms of recurrence. The KSF procedure seems promising for treating pilonidal sinus disease, with the advantages of shorter operation, healing, and return to work times. It also provides lower partial wound dehiscence and necrosis rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pilonidal sinus (PS) disease is a common chronic inflammatory disease that mostly affects young male adults. It predominantly occurs in the natal cleft of sacrococcygeal area. However, it can also occur in the axilla, neck, suprapubic and periumbilical areas [1]. The incidence of the disease is 26/100,000 [2]. Clinical presentation can vary from asymptomatic pits to chronically draining sinuses [3]. There is no consensus on the etiology of the disease, although environmental and congenital factors are thought to play a role [4]. The estimated risk factors are male gender, sedentary occupation, family history, nature of hairs and vulnerability of the skin [5,6,7]. Hairs in the sacrococcygeal area penetrate the skin after repeated minor trauma and create a foreign body reaction which then leads to secondary infection and pilonidal abscess [8].
The eradication of all the branches of the sinus tract is the basic principle of PS surgery [9]. The ideal surgery should result in minimal time off work with low complication and recurrence rates [10]. The reconstructive stage is the most critical step of surgical treatment. With the intention of reducing wound-related complications and recurrence, it is important to achieve an off-midline closure with flattening of the natal cleft [11].
Due to the various local complications and recurrence, debates about ideal surgical treatment method are still ongoing and there is no consensus on the ideal PS surgery technique. Adaptation to PS surgery of novel flap methods used in defect closure may be beneficial in achieving ideal surgical results. The Keystone flap (KSF) is a curvilinear trapezoid-shaped flap consisting of two conjoined VY island flaps which release the longitudinal tension [12]. It is used for reconstruction in various parts of the body, especially in the extremities and trunk [13,14,15].
The aim of the current study was to present the short-term results of the KSF technique in PS treatment and to compare these with the results of the Limberg flap (LF) technique.
Materials and methods
Patients and study design
A retrospective review was made of the prospectively maintained database of all consecutive patients surgically treated for PS disease with KSF and LF procedures from January 2018 to January 2020. The study was designed in accordance with the principles of the Declaration of Helsinki, and approval for the study was granted by the Institutional Review Board (No: 2021/152).
Inclusion and exclusion criteria
The inclusion criteria for the surgical procedures were age ≥ 18 years, at least 1-year follow-up period, and Cruse-Foord (CF) wound classification < III. Patients with minor inflammation findings (CF class III) were included in the study after antibiotic treatment. The study exclusion criteria were defined as acute abscess formation, CF class IV wound, or recurrent PS disease.
Preoperative evaluation and postoperative follow-up
In the first hospital visit, we informed all patients about the surgical procedures, gave information about the pre-and postoperative periods, and explained the procedures using simple drawings. The patients decided on the surgery type themselves. Written informed consent forms were obtained before the surgery.
Age, gender, body mass index (BMI), smoking, history of diabetes mellitus (DM), operation time, volume of excised specimen (VS), duration of hospitalization, duration of drainage, duration of healing, and time to return to work were obtained from the patient files. Complications and recurrence were recorded.
Postoperative complications were categorized as either major or minor [16]. Major complications were defined as return to the operating room (OR) (for surgical drainage or revision), a need for negative pressure wound therapy, and prolonged wound healing (failure of wound healing at 12 weeks follow-up). Minor complications were defined as seroma, hematoma, wound site infection (managed with oral antibiotics) and partial wound dehiscence (cuticular disruption). The term recurrence was used when symptoms of the disease recurred some time after complete wound healing [17].
The wound was classified according to the Cruse-Foord classification before the surgery [18, 19]. The volume of the excised specimen (VS) was measured with a graduated cylinder as described by Alptekin et al. [9]. Operation time was defined as the time between the first incision and the last skin suture. Hospital stay was recorded as the time between the day of surgery to the day of discharge. Healing time was defined as the interval between the date of surgery and removal of the sutures. For patients with wound-related complications, it was accepted as the time until the wound was completely healed. Time to return to work was defined as the time from surgery until the return to employment or leisure.
Drains were removed when drainage decreased to < 20 ml/day. The patients were advised to avoid forceful squating and pressure on the operated site for 2 weeks. The sutures were removed on the tenth postoperative day in patients without local wound problems.
Surgical technique
Before the operation, gluteal and sacral regions were shaved and prophylactic antibiotic (cefazolin 1 g) was administired. All operations were performed under spinal anesthesia in the jack-knife position. The gluteal skin was retracted towards both sides using adhesive bandages to expose the intergluteal sulcus. Closed-suction drainage was used in patients with a volume of excised specimen > 25 cc.
The KSF was designed according to its original description [12]. After marking the area to be excised including the pilonidal sinus, the KSF was designed as a curvilinear trapezoidal shape with 1:1 ratio width to the expected defect (Fig. 1). The excision of all the sinus tracts and fistula borders was carried out deep to the postsacral fascia. The borders of the flap were incised and dissected down to the deep fascia with minimal undermining of the flap to preserve the vascular perforators. Then, the flap was advanced to cover the defect without leaving any deadspace and was sutured to the defect side. The donor site was closed primarily. The wound was closed in two layers as subcutaneous deep tissue and skin with absorbable (2/0 polyglactin) and non-absorbable (2/0 polypropylene) sutures, respectively (Fig. 2).
The LF procedure was performed as described by Mentes et al. [20]. The excision area including all the pilonidal sinus tracts was marked as a rhomboid form and the flap was designed though the right- or left-side gluteus maximus (Fig. 3). The skin incision was deepened to the postsacral fascia in the midline and the gluteus maximus fascia in the flap area. The rhomboid-shaped tissue was removed en bloc. The flap was fully mobilized and transposed medially to fill the defect. The subcutaneous tissue was drawn together with absorbable (2/0 polyglactin) sutures. The skin was closed with non-absorbable (2/0 polypropylene) interrupted sutures (Fig. 4).
Statistical analyses
Data obtained in the study were analyzed statistically using Statistical Package for the Social Sciences software (SPSS; version 15.0; SPSS Inc., Chicago, Illinois, USA). Continuous variables were presented as mean ± standard deviation (SD) values and categorical variables were presented as number (n) and percentage (%). Normally distributed continuous variables were compared using the Student’s t test and non-normally distributed continuous variables using the Mann–Whitney U test. Categorical variables were compared using the Chi-square test. A value of p < 0.05 was considered statistically significant.
Results
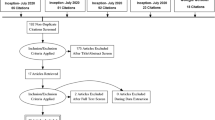
Between the specified dates, 141 consecutive pilonidal sinus patients underwent KSF or LF procedures. A total of 17 patients were excluded due to loss of follow-up and exclusion criteria. Therefore, evaluation was made of 124 patients. The mean follow-up period was 17.6 months (range 13–22 months). The overall follow-up rate was 86.4%. According to the type of surgery, 53 patients were included in the KSF group and 71 patients in the LF group. Of these patients, 7 (5.65%) were female and 117 (94.35%) were male and the mean age was 25.33 ± 6.72 years. There was no statistically significant difference between the groups in terms of baseline characteristics and preoperative wound classification (Table 1).
The mean hospital stay, duration of drainage and VS did not show any significant difference between the groups. The mean operation time was significantly shorter in the KSF group than in the LF group (35.86 ± 8.29 min and 45.31 ± 6.19 min, respectively) (p < 0.01). The mean healing time was 17.35 ± 3.35 days in the LF group, and significantly shorter in the KSF group at 11.90 ± 3.69 days (p < 0.01). The mean time to return work was significantly shorter in the KSF group (14.50 ± 9.95 days in the KSF group and 18.45 ± 4.87 days in the LF group) (p < 0.01). The postoperative outcomes are shown in Table 2.
Negative pressure wound therapy was required by two patients in the LF group and by not patients in the KSF group. Prolonged wound healing was significantly more common in the LF group. It was observed in 12 (16.9%) patients in the LF group and 2 (3.8%) patients in the KSF group (p = 0.02).
An additional intervention in the OR was required by 15 (21.1%) patients in the LF group, and at the significantly lower rate of 4 (7.5%) patients in the KSF group (p = 0.03). Of these patients in the LF group, revision surgery was applied to eight patients due to complete flap dehiscence, and due to necrosis in two, and abscess drainage was applied to five patients. In the KSF group, abscess drainage was applied to two patients and revision due to complete flap dehiscence to two patients. No flap necrosis occurred in the KSF group.
A significant difference was determined between the groups in respect of partial wound dehiscence. It was observed in 5 (9.4%) patients in the KSF group and 17 (23.9%) patients in the LF group (p = 0.03). All these patients were healed with daily dressings without any additional intervention. No significant difference was determined between the groups in respect of other minor complications such as seroma, hematoma and wound infection. The groups did not differ significantly with regard to recurrence of disease (p = 0.73). The overall major–minor complication and recurrence rates are shown in Table 3.
Discussion
The results of this study demonstrated that KSF can be seen as an effective procedure in PS surgery. When compared with the LF procedure, it results in lower wound dehiscence and necrosis rates, and shorter operation time, healing time, and return to work time.
The treatment choice for cases of PS disease usually depends on the clinical presentation. While successful treatment can be achieved with a conservative approach such as shaving the hair or local phenol application in simple cases, complex cases may require wide excision with extensive reconstructive flap procedures [21].
The success of the surgical treatment is based on a short operation time and duration of hospitalization, early return to work, low recurrence rate and few complications [1, 21, 22]. However, most surgical procedures fail to meet all these goals together.
Prolonged operation time has been found to be a risk factor for surgical site infection (SSI) in PS surgery [9]. In the present study, the mean operation time for the LF procedure was 45.31 ± 6.19 min, which was compatible with the literature [11, 23, 24]. In the KSF group, the mean operation time was significantly shorter than in the LF group, presumably because of the relatively straightforward design in which extensive mobilization and transposition are not required. However, the mean SSI rate did not show any significant difference between the groups.
One of the parameters that patients consider when deciding on the surgical technique for PS disease is the time to return work after surgery [25]. A shorter healing time and return to work provides better quality of life after surgery [22]. In the present study, healing time and time to return to work were significantly shorter in the KSF group.
In flap procedures, postoperative complications and recurrence are closely related with proper closure of the resultant defect following the excision of the diseased tissue [7]. Off-midline closure techniques in particular have been suggested to be able to obtain the desired outcomes [26, 27]. LF technique is one of the most preferred off-midline surgical procedures for sacrococcygeal PS disease. It has been in use for a long time, with reported complication and recurrence rates of up to 16% and 5%, respectively [17]. However this procedure has the disadvantage that the scar crosses the natal cleft allowing for increased susceptibility to infection, local complications and recurrence [11].
In the present study, there was a significantly lesser need for additional intervention in the OR in the KSF group and no flap necrosis occurred in this group. In the LF group, necrosis was observed at the upper apex of the rhomboid defect in two patients. Revision was not successful in these patients and secondary wound healing was required. Negative pressure wound therapy was used in these patients to promote wound healing.
Necrosis and flap dehiscence are closely related with tension on the flap in PS surgery. Excessive tension may result in inadequate flap perfusion and necrosis [28]. The lack of necrosis and lower rate of complete wound dehiscence in the KSF procedure may be explained by the design of the flap. In this procedure, the tension on the flap is effectively reduced and re-distributed equally [29], thereby facilitating the healing process. Consistent with this, prolonged wound healing was also significantly lower in the KSF group.
The use of a prophylactic drain in PS surgery is still controversial. Although there is a traditional opinion that the use of a prophylactic drain reduces complications such as seroma and hematoma [24, 30, 31], some surgeons disagree and advocate that the routine usage of a drain is unnecessary [32]. Seroma formation, that is, non-infected fluid collection beneath the flap, can cause local complications varying from delayed wound healing to infection and skin flap necrosis [33]. The risk of seroma is closely related to the size of the dead space left after the excision of the diseased tissue. In our practice, a drain is not routinely placed in cases where the VS is < 25 cc in the PS surgery. The VS reflects the size of excised tissue and the resulting defect [9]. In the present study, there was no significant difference between the groups in respect of the mean duration of drainage, seroma, hematoma, and VS.
Among the minor complications, only partial wound dehiscence showed a difference between the groups. It was observed significantly less in the KSF group. All these patients obtained full healing with daily dressings without any additional intervention.
There were limitations to this study, primarily that it was retrospective and the groups were not randomized. However, we included all consecutive patients surgically treated for PS disease with a flap technique between the study period. These limitations should be considered while interpreting the study results.
Conclusion
The KSF procedure seems to be an effective alternative to the LF procedure in pilonidal sinus surgery, with the advantages of lower partial wound dehiscence and necrosis rates and shorter operation, healing, and return to work times.
References
Çiftci F, Abdurrahman I (2015) A different disease: extrasacrococcygeal pilonidal sinuses etiopathogenesis. Int J Clin Exp Med 8(7):11567
Saydam M, Ozturk B, Sinan H, Balta AZ, Demir P, Ozer MT et al (2015) Comparison of modified Limberg flap transposition and lateral advancement flap transposition with Burow’s triangle in the treatment of pilonidal sinus disease. Am J Surg 210(4):772–777
Eastment J, Slater K (2020) Outcomes of minimally invasive endoscopic pilonidal sinus surgery. Asian J Endosc Surg 13(3):324–328
Johnson EK (2018) Expert commentary on pilonidal disease: management and definitive treatment. Dis Colon Rectum 61(7):777–779
Søndenaa K, Andersen E, Nesvik I, Søreide J (1995) Patient characteristics and symptoms in chronic pilonidal sinus disease. Int J Colorectal Dis 10(1):39–42
Akinci ÖF, Bozer M, Uzunköy A, Düzgün ŞA, Coşkun A (1999) Incidence and aetiological factors in pilonidal sinus among Turkish soldiers. Eur J Surg 165(4):339–342
Kartal A, Aydın HO, Oduncu M, Ferhatoğlu MF, Kıvılcım T, Filiz Aİ (2018) Comparison of three surgical techniques in pilonidal sinus surgery. Prague Med Rep 119(4):148–155
Johnson EK, Vogel JD, Cowan ML, Feingold DL, Steele SR (2019) The American Society of Colon and Rectal Surgeons’ clinical practice guidelines for the management of pilonidal disease. Dis Colon Rectum 62(2):146–157
Alptekin H, Yilmaz H, Kayis SA, Sahin M (2013) Volume of the excised specimen and prediction of surgical site infection in pilonidal sinus procedures (surgical site infection after pilonidal sinus surgery). Surg Today 43(12):1365–1370
Porrett JK, Porrett LJ, Ho Y-H, Rozen WM (2019) Pilonidal sinus—plenty of literature yet lack of direction: a pooled analysis. Int Surg 103(9–10):443–451
Bessa SS (2013) Comparison of short-term results between the modified Karydakis flap and the modified Limberg flap in the management of pilonidal sinus disease: a randomized controlled study. Dis Colon Rectum 56(4):491–498
Behan FC (2003) The keystone design perforator island flap in reconstructive surgery. ANZ J Surg 73(3):112–120
Huang J, Yu N, Long X, Wang X (2017) A systematic review of the keystone design perforator island flap in lower extremity defects. Medicine 96(21):e6842
Parus A, Waler A, Westmoreland T, Johnson C, Kellogg B (2020) Keystone Flap Reconstruction after Resection of a Large Paraspinal Venous Malformation in an Infant. Plast Reconstr Surg Glob Open 8(10):e3141
Rini IS, Gunardi AJ, Marsaulina RP, Aryandono T, Dachlan I, Dwiprahasto I (2020) A systematic review of the keystone design perforator island flap in the reconstruction of trunk defects. Arch Plast Surg 47(6):535
Hatch Q, Marenco C, Lammers D, Morte K, Schlussel A, McNevin S (2020) Postoperative outcomes of Bascom cleft lift for pilonidal disease: A single-center experience. Am J Surg 219(5):737–740
Guner A, Boz A, Ozkan OF, Ileli O, Kece C, Reis E (2013) Limberg flap versus Bascom cleft lift techniques for sacrococcygeal pilonidal sinus: prospective, randomized trial. World J Surg 37(9):2074–2080
Cruse PJ, Foord R (1973) A five-year prospective study of 23,649 surgical wounds. Arch Surg 107(2):206–210
Petersen S, Aumann G, Kramer A, Doll D, Sailer M, Hellmich G (2007) Short-term results of Karydakis flap for pilonidal sinus disease. Tech Coloproctol 11(3):235–240
Mentes O, Bagci M, Bilgin T, Ozgul O, Ozdemir M (2008) Limberg flap procedure for pilonidal sinus disease: results of 353 patients. Langenbecks Arch Surg 393(2):185–189
Harries RL, Alqallaf A, Torkington J, Harding KG (2019) Management of sacrococcygeal pilonidal sinus disease. Int Wound J 16(2):370–378
Destek S, Bektasoglu HK, Kunduz E, Akyuz MN (2020) Comparison of postoperative quality of life of Limberg flap and Karydakis flap in pilonidal sinus operations. Turk J Surg 36(1):59–65
Ates M, Dirican A, Sarac M, Aslan A, Colak C (2011) Short and long-term results of the Karydakis flap versus the Limberg flap for treating pilonidal sinus disease: a prospective randomized study. Am J Surg 202(5):568–573
Can MF, Sevinc MM, Hancerliogullari O, Yilmaz M, Yagci G (2010) Multicenter prospective randomized trial comparing modified Limberg flap transposition and Karydakis flap reconstruction in patients with sacrococcygeal pilonidal disease. Am J Surg 200(3):318–327
Grabowski J, Oyetunji TA, Goldin AB, Baird R, Gosain A, Lal DR et al (2019) The management of pilonidal disease: a systematic review. J Pediatr Surg 54(11):2210–2221
Omer Y, Hayrettin D, Murat C, Mustafa Y, Evren D (2015) Comparison of modified limberg flap and modified elliptical rotation flap for pilonidal sinus surgery: a retrospective cohort study. Int J Surg 16:74–77
McCallum IJ, King PM, Bruce J (2008) Healing by primary closure versus open healing after surgery for pilonidal sinus: systematic review and meta-analysis. BMJ 336(7649):868–871
Arpaci E, Altun S, Orhan E, Eyuboglu A, Ertas NM (2018) A new oval advancement flap design for reconstruction of pilonidal sinus defect. World J Surg 42(11):3568–3574
Shayan R, Behan FC (2013) Re: the “keystone concept’: time for some science. ANZ J Surg 83(7–8):499
Topgül K, Özdemir E, Kiliç K, Gökbayir H, Ferahköşe Z (2003) Long-term results of Limberg flap procedure for treatment of pilonidal sinus. Dis Colon Rectum 46(11):1545–1548
Mentes BB, Leventoglu S, Cihan A, Tatlicioglu E, Akin M, Oguz M (2004) Modified Limberg transposition flap for sacrococcygeal pilonidal sinus. Surg Today 34(5):419–423
Urhan MK, Kücükel F, Topgul K, Özer İ, Sari S (2002) Rhomboid excision and Limberg flap for managing pilonidal sinus. Dis Colon Rectum 45(5):656–659
Calisir A, Ece I, Yormaz S, Colak B, Kirazli H, Sahin M (2020) The effects of platelet-rich plasma to decrease the risk of seroma formation after mastectomy and axillary dissection. J Surg Res 256:156–162
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
This protocol was approved by the local Institutional Review Board (No: 2021/152).
Informed consent
Informed consent was obtained from patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Calisir, A., Ece, I. Comparison of the Keystone flap and the Limberg flap technique in the surgical treatment of pilonidal sinus disease. Updates Surg 73, 2341–2346 (2021). https://doi.org/10.1007/s13304-021-01153-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-021-01153-w