Abstract
Background and aims
Several studies indicate that peroxisome proliferator-activated receptor gamma (PPARγ) represses activator protein-1 (AP-1) and nuclear factor kappa B (NF-κB) transcriptional activity and this negative cross-talk occupies an important role in carcinogenesis. The present study evaluated the differential expression profile of AP-1 constituents (c-FOS and phosphorylated-active pc-JUN), p-IκB-α (phosphorylated IκB-α, a signaling intermediate of NF-κB pathway), PPARγ, cyclic AMP-response element binding-binding protein (CBP, a known AP-1, NF-κB, and PPARγ transcriptional coactivator), epidermal growth factor receptor (EGF-R), p53, and COX-2 in normal colonic epithelial cells and colon adenocarcinoma cells.
Materials and methods
Immunohistochemical methodology was performed on formalin-fixed, paraffin-embedded sections from 60 patients with colon adenocarcinomas. A molecular profile was created for each patient and the induction or down-regulation of each pathway from normal to cancer cells was documented. Relationships between transcription factors and downstream molecular targets were evaluated by Spearman’s rho correlation coefficient and validated by nonparametric Kruskal–Wallis test.
Results/findings
P-IκB-α (P<0.001), CBP (P<0.001), c-FOS (P=0.047), pc-JUN (P=0.047), and EGF-R (P<0.001) were up-regulated in colon adenocarcinomas while PPARγ (P<0.001) was concomitantly down-regulated. p-IκB-α, CBP, pc-JUN, EGF-R, and p53 expression all correlated positively with COX-2 while PPARγ expression correlated inversely with COX-2.
Interpretation/conclusion
NF-κB/PPARγ and/or AP-1/PPARγ expressional ‘on/off’ switches are common molecular events during colorectal carcinogenesis. Down-regulation of PPARγ and induction of the CBP transcriptional coactivator can augment NF-κB and AP-1 transcriptional activities leading to up-regulation of COX-2 expression in colon adenocarcinoma cells. p-IκB-α, pc-JUN, and CBP could potentially provide the basis for future molecular-targeted anticancer therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The activator protein-1 (AP-1) transcription factor is a hetero- or homodimeric complex that comprises members of the JUN, FOS, and activating transcription factor (ATF) subfamilies of basic region-leucine zipper (bZIP) DNA-binding proteins [1, 2]. AP-1 constitutes a major target of the mitogen-activated protein kinase (MAPK) signal transduction cascades which are activated in response to a wide variety of stimuli including growth factors, cytokines, neurotransmitters, and environmental stress [3–6]. Transcriptional activation of AP-1 target genes is funneled by recruitment of coactivator proteins such as CBP (cyclic AMP-response element binding-binding protein) which connect AP-1 with the basal transcriptional machinery [7]. Multiple lines of evidence indicate that overexpression of CBP is associated with carcinogenesis [8]. AP-1 can exert both tumor-promoting and tumor-suppressing effects by modulating the expression of genes involved in cellular proliferation, differentiation, apoptosis, tumor invasion, and angiogenesis [9–11]. The exact role of AP-1 in colon cancer remains to be elucidated. Some studies indicate that AP-1 activation is associated with colorectal cancer growth [12, 13] while other reports suggest that AP-1 promotes differentiation and apoptosis [14].
One of the best studied AP-1 regulated genes is cox-2 (cyclooxygenase-2) [15, 16]. Cox-2 behaves as an immediate early gene and its promoter contains transcriptional regulatory elements for various transcription factors including AP-1 and nuclear factor kappa B (NF-κB) [17, 18]. Moreover, in vitro experiments have shown that the histone acetyltransferase activity of CBP is important for AP-1-mediated induction of COX-2 [19, 20].
NF-κB is an inducible transcription factor and a positive regulator of COX-2 expression in response to various cytokines and growth factors [21–23]. NF-κB is retained to the cytoplasm in an inactive state by binding to inhibitory IκB proteins that block its nuclear localization sequences (NLS). Multiple stimuli induce phosphorylation of IκB-α at Ser-32 leading to dissociation of NF-κB from IκB-α, unmasking of its NLS, and stimulation of its transcriptional activity [21]. NF-κB is persistently active in multiple tumors and seems to occupy an important role in carcinogenesis [24].
Mounting evidence indicates that AP-1 and NF-κB transcriptional activities are negatively modulated by peroxisome proliferator-activated receptor gamma (PPARγ) and that this negative cross-talk is implicated in carcinogenesis and inflammation. PPARγ is a member of the nuclear receptor superfamily of ligand-inducible transcription factors and its ligands, namely, polyunsaturated fatty acids, non-steroidal anti-inflammatory drugs (NSAIDs), and thiazolidinediones bear anticolonic cancer properties [25]. It has been demonstrated that activation of PPARγ suppresses AP-1-mediated induction of COX-2 expression in human epithelial cells due to competition of PPARγ with AP-1 for limited amounts of the transcriptional coactivator CBP [26, 27]. Moreover, activation of PPARγ suppresses NF-κB-mediated transcription in Caco2 colon cancer cells [28]. Besides the competition of PPARγ and AP-1 for CBP, multiple molecular mechanisms that explain the negative PPARγ/AP-1 and PPARγ/NF-κB cross-talks have been proposed [29–31].
The primary aim of our study was to investigate the role of NF-κB, PPARγ, AP-1, and CBP in colon adenocarcinomas by evaluating their differential expression profile in normal colonic epithelial cells and colon cancer cells. Moreover, we correlated the expression of NF-κB, PPARγ, AP-1, and CBP with the expression of COX-2 which is known to be up-regulated in colon adenocarcinomas. In the case of AP-1, we examined the expression of c-FOS and pc-JUN (phosphorylated c-JUN). Expression of the epidermal growth factor receptor (EGF-R)—one of the activators of Ras–Raf–MAPK–AP-1 cascade—was also evaluated. To determine the activation of the NF-κB pathway, expression of the phosphorylated form of IκB-α (p-IκB-α) was evaluated. Finally, as p53 has been shown to influence cox-2 gene transcription in vitro [32] and p53 status has been correlated with COX-2 levels in certain neoplasms [33, 34], we also correlated the expression of p53 with COX-2 in colon cancer.
Our study provided novel evidence that p-IκB-α, CBP, and AP-1 are up-regulated in colon adenocarcinomas while PPARγ is concomitantly down-regulated. p-IκB-α, CBP, pc-JUN, EGF-R, and p53 expression all correlated positively with COX-2 while PPARγ expression correlated inversely with COX-2. We pose that NF-κβ/PPARγ and/or AP-1/PPARγ expression ‘on/off’ switches occur in colon adenocarcinomas, which, coupled by induction of the CBP transcriptional coactivator, are associated with up-regulation of COX-2.
Materials and methods
Specimens and clinicopathological data
Sixty cases of colorectal adenocarcinomas surgically resected from 36 men and 24 women were included in our study. The age of the patients ranged from 39 to 90 years (males mean age=71.6 years, SD=12.15 years; females mean age=71.3, SD=9.2; total mean age=71.5, SD=10.98). Colon adenocarcinomas were classified as well (nine cases), moderately (40 cases), and poorly differentiated (11 cases), according to standard pathologic criteria. Staging was performed according to the American Joint Committee on Cancer (AJCC) system (stage I, eight cases; stage II, 23 cases; stage III, 12 cases; and stage IV, 17 cases). Tissue specimens obtained from tumors and adjacent normal colon were fixed in 10% (v/v) buffered formalin and embedded in paraffin. Serial 4-μm sections were obtained for staining with hematoxylin and eosin and for immunohistochemistry.
Immunohistochemical methodology
The eight primary antibodies employed in the present study, their sources, and their characteristics are depicted in Table 1.
Microwave irradiation in 0.01 M citric buffer (pH 6.0) was performed as an antigen retrieval method in all cases except for EGF-R. In the case of EGF-R, enzymatic pretreatment with pepsin (DIGEST-ALL, Zymed Laboratories) was done for 10 min in 37°C.
All primary antibodies were diluted with ChemMate (DakoCytomation) antibody diluent and applied on tissue sections for 30 min at room temperature. The working dilutions are presented in Table 1.
Immunoreactivity was detected employing the EnVision (DakoCytomation) protocol in all cases except for EGF-R and PPARγ. EGF-R immunopositivity was detected using the SuperPicTure Polymer Detection Kit (Zymed Laboratories) while PPARγ immunoreactivity was detected using the PowerVision (ImmunoVision Technologies) protocol. Sections from colon adenocarcinomas, in which the primary antibodies were omitted, were used as negative controls.
Our study evaluated the expression of the aforementioned molecular markers in the invasive ‘front’ of the tumor, in areas rich in non-necrotic tumor glands. After a review of the hematoxylin and eosin-stained sections of all blocks for each case, we carefully selected the blocks that contained both the invasive margin of tumor and normal colonic mucosa. That was possible for 49 cases (in these 49 cases, we were able to select blocks that contained both the invasive margin of tumor and normal colonic mucosa). In these 49 cases, the immunohistochemical expression of the molecular markers in the normal tissue and the tumor was evaluated on the same slide. In the remaining 11 cases, we stained and evaluated two slides per case (for all eight antibodies): one slide from blocks that contained the invasive front of tumor and one slide from blocks that contained normal tissue.
Immunostained sections were graded based on a five-level scale presented in Table 2. A minimum of 1,000 cells was detected in each specimen. Specimens with up to 50% of positive cells were scored purely based on the percentage of positive cells (0, <1%; +1, 1–25%; and +2, 26–50%). Specimens with more than 50% positive cells were scored as (+3) or (+4) according to the intensity of the staining (moderate vs strong, respectively). No cases with weak staining intensity and more than 50% positive cells were detected.
Two independent pathologists (PAK and GPV) evaluated and scored all sections using this scale without prior knowledge of the clinicopathological characteristics of each case. Specimens with interobserver disagreement were reassessed by simultaneous examination by the two pathologists in a double-headed light microscope. There was no interobserver disagreement regarding assessment of tumor differentiation. In terms of immunostaining scoring, there was disagreement in five cases for c-FOS, six cases for pc-JUN, four cases for p-IκB-α, three cases for CBP, five cases for EGF-R, four cases for p53, six cases for PPARγ, and six cases for COX-2. The Cohen’s coefficient of agreement was k=0.88, P<0.01 (nearly perfect as per Landis and Koch criteria).
Statistical analyses
Wilcoxon signed-rank tests were used to compare the level of c-FOS, pc-JUN, CBP, PPARγ, p-IκB-α, and COX-2 expression between normal colonic cells and colon adenocarcinoma cells. The level of expression of all these factors was compared among the three adenocarcinoma differentiation degrees and the four AJCC stages by nonparametric Kruskal–Wallis analysis of variance (ANOVA). The association between transcription factors and downstream molecular targets was graphically presented using boxplots which depict the level of expression of one factor across different levels of expression of the other factor. The direction (positive vs negative) and the strength of each association were evaluated using the Spearman’s rho correlation coefficient which is appropriate for ordinal data and represents the nonparametric version of Pearson correlation coefficient. To further validate the strength and the statistical significance of each association, we compared (for each pair of associated factors) the level of expression of one factor among the different levels of expression of the other factor using nonparametric Kruskal–Wallis ANOVA test. All analyses were performed using SPSS 9.0 for Windows (SPSS, Chicago, IL, USA).
Results
P-IκB-α expression is induced in colon adenocarcinomas and correlates positively with COX-2
The immunohistochemical results for p-IκB-α and COX-2 are presented in Table 3.
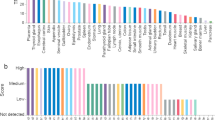
A statistically higher expression in colon adenocarcinomas than in normal colon was detected in the case of p-IκB-α (P<0.001) and COX-2 (P<0.001). The induction of COX-2 and p-IκB-α is shown in Fig. 1 (b and d, respectively). P-IκB-α and COX-2 immunostaining is also shown in Fig. 2 (c and f, respectively), which includes the molecular profile of a 74-year-old female with a well-differentiated colon adenocarcinoma.
a Down-regulation of PPARγ in a moderately differentiated adenocarcinoma as compared to adjacent normal colon (×40). b Induction of COX-2 in a moderately differentiated adenocarcinoma compared to nearby normal colon (×40). c Induction of CBP in a well-differentiated colon adenocarcinoma and dysplastic epithelium as compared to nearby colon (×40). d Induction of p-IκB-α in a moderately differentiated adenocarcinoma (×40). e Induction of c-FOS in a poorly differentiated adenocarcinoma compared to nearby normal colon (×40). f Strong p53 immunostaining in a well-differentiated adenocarcinoma and negative p53 staining in normal colon. g Induction of EGF-R in a moderately differentiated adenocarcinoma. h Equal expression of pc-JUN in normal and nearby dysplastic epithelium
Molecular profile of a 74-year-old female with a well-differentiated colon adenocarcinoma: a CBP (+3) expression, b PPARγ (negative/0) expression, c p-IκB-α (+4) expression, d p53 (+4) expression, e EGF-R (+2) expression, f COX-2 (+4) expression, g pc-JUN (+2) expression, and h c-FOS (1+) expression
Overall, out of the total 60 cases, increased expression in colon adenocarcinomas than in the adjacent normal colon was identified for COX-2 in 52 cases and for p-IκB-α in 49 cases (Table 6).
P-IκB-α expression in colon adenocarcinomas paralleled the expression of COX-2. The boxplot in Fig. 3a presents p-IκB-α expression across different levels of COX-2 expression. P-IκB-α was statistically significantly positively correlated with COX-2 expression (Spearman’s rho=0.513, P<0.001), and p-IκB-α expression was statistically significantly different among the different levels of COX-2 expression (Kruskal–Wallis P<0.001) (Fig. 3a).
a–d Boxplots demonstrating the expression of PPARγ, p-IκB-α, CBP, and pc-JUN across the various levels of COX-2 expression. The number of patients (N) appears also in each boxplot on the x axis. The relationship between each molecular target and COX-2 is evaluated using the Spearman’s rho correlation coefficient. The sign of the coefficient indicates the direction of the association (positive vs negative). Nonparametric Kruskal–Wallis test assesses whether there is an overall statistical difference in the level of expression of PPARγ, p-IκB-α, CBP, and pc-JUN among the various levels of COX-2 expression. In all cases (a–d) PPARγ, p-IκB-α, CBP, and pc-JUN expression was statistically significantly different across the various levels of COX-2 expression. Kruskal–Wallis P is shown for each case
Finally, p-IκB-α and COX-2 expression did not show any correlation with tumor staging and differentiation.
PPARγ expression declines in colon adenocarcinomas and is inversely correlated with COX-2
PPARγ expression was statistically significantly higher in normal colonic epithelium than in colon adenocarcinomas (P<0.001). A reduced expression of PPARγ in colon adenocarcinomas compared to adjacent normal colon was detected in 44 cases; no change was found in 15 cases while increased PPARγ expression (in colon adenocarcinomas compared to normal colon) was found only in one patient. These results are depicted in Table 6, and Fig. 1a shows a case of PPARγ down-regulation.
The comparison of the level of PPARγ expression among different levels of COX-2 expression is graphically presented in the boxplot in Fig. 3b. A nonparametric analysis revealed that there was a statistically significant inverse correlation between PPARγ and COX-2 (Spearman’s rho=−0.412, P=0.001). Further nonparametric analysis using Kruskal–Wallis ANOVA revealed that PPARγ expression was statistically significantly different among the different levels of COX-2 expression (Kruskal–Wallis P=0.002).
It is of importance that we found that the down-regulation of PPARγ was associated with the up-regulation of p-IκB-α expression indicating a NF-κB/PPARγ expression on/off switch. Specifically, a statistically significantly negative correlation was identified between PPARγ and p-IκB-α expression in colon adenocarcinomas (Spearman’s rho=−0.444, P<0.001).
Finally, PPARγ expression did not show any correlation with tumor staging and differentiation.
CBP is overexpressed in colon adenocarcinomas compared to normal colon and correlates positively with COX-2
The immunohistochemistry results for CBP are presented in Tables 4 and 6.
A statistically higher expression of CBP was detected in colon adenocarcinomas than in normal colon (P<0.001). The induction of CBP is shown in Fig. 1c and in Fig. 2a. Overall, out of the total 60 cases, increased expression in colon adenocarcinomas than in the adjacent normal colon was identified for CBP in 30 cases (Table 6).
In Fig. 3c, boxplots of CBP expression across different levels of COX-2 expression are presented. In colon adenocarcinomas, CBP expression correlated positively with COX-2 expression (Spearman’s rho=0.461, P=0.005). Importantly, CBP was different among the different levels of COX-2 expression (Kruskal–Wallis P=0.001 and P=0.002, respectively) (Fig. 3c).
Finally, p-IκB-α and COX-2 expression did not show any correlation with tumor staging and differentiation.
Expression of AP-1 constituents (c-FOS and pc-JUN) is increased in colon adenocarcinomas—pc-JUN expression correlates positively with COX-2
The immunohistochemistry results for c-FOS and pc-JUN are presented in Table 4. The results of the comparison of the level of expression of c-FOS and pc-JUN between normal colon and colon adenocarcinoma cells are depicted in Table 6. Figure 1h shows a case of equal pc-JUN expression in normal and nearby dysplastic epithelium while induction of c-FOS is shown in Fig. 1e. Pc-JUN and c-FOS immunostaining are also shown in Fig. 2 (g and h, respectively), which includes the molecular profile of a 74-year-old female with a well-differentiated colon adenocarcinoma.
Overall, a statistically higher expression in colon adenocarcinomas than in normal colon was detected for c-FOS (P=0.04) and pc-JUN (P=0.04). Nevertheless, there were some adenocarcinoma cases where down-regulation of pc-JUN (13 cases) and c-FOS expression (13 cases) compared to normal colon was detected (Table 6). There were only six cases (10%) where neither AP-1 (c-FOS or pc-JUN) induction nor p-IκB-α induction was noted. Overall, in 90% of all cases (54 cases), either activation of NF-κB (induction of p-IκB-α) or induction of AP-1 (c-FOS or pc-JUN) was found in colorectal adenocarcinomas.
Pc-JUN expression was statistically significantly positively correlated with COX-2 expression (Spearman’s rho=0.444, P<0.001), and pc-JUN expression was statistically significantly different among various levels of COX-2 expression (Kruskal–Wallis P=0.001). Figure 3d presents pc-JUN expression level across different levels of COX-2 expression. On the contrary, c-FOS expression did not correlate with COX-2 in a statistically significant manner.
Finally, there was a statistically significant association (P=0.035) between pc-JUN expression and tumor differentiation, with a tendency for more differentiated tumors to harbor higher levels of pc-JUN. A similar statistically significant association (P=0.006) was identified between pc-JUN expression and tumor stage, with more advanced-stage tumors displaying lower levels of pc-JUN. On the contrary, c-FOS expression did not show any correlation with tumor staging and differentiation.
EGF-R is overexpressed in colon adenocarcinomas compared to normal colon and its expression correlates positively with COX-2
The immunohistochemistry results for EGF-R are presented in Table 5. EGF-R immunostaining is shown in Fig. 1g and Fig. 2e.
A statistically higher expression of EGF-R was noted in colon adenocarcinomas than in normal colon (P<0.001). Overall, out of the total 60 cases, increased expression of EGF-R in colon adenocarcinomas than in the adjacent normal colon was identified in 25 (41.7%) of the cases (Table 6).
EGF-R expression was statistically significantly positively correlated with COX-2 expression (Spearman’s rho=0.429, P<0.001). It is important to note that EGF-R expression was also statistically significantly positively correlated with the downstream c-FOS and pc-JUN expression (Spearman’s rho=0.476, P<0.001 and Spearman’s rho=0.431, P=0.001, respectively), supporting an orchestrated induction of EGF-R, c-FOS, and pc-JUN in colon adenocarcinomas.
EGF-R expression did not show any correlation with tumor staging and differentiation.
p53 correlates positively with COX-2 expression
The immunohistochemical results for p53 are shown in Table 5. P53 immunostaining is shown in Fig. 1f and Fig. 2d.
It is well known that, in tumor cells, high p53 expression is a marker of inactivated and/or mutated p53. The primary antibody used for p53 immunostaining recognizes both wild and mutant p53 under both denaturing and non-denaturing conditions. Therefore, the high expression of p53 that was detected in colon cancer cells reflects the presence of mutated and/or inactivated p53 in these cells.
In colon adenocarcinomas, p53 correlated positively with COX-2 (Spearman’s rho=0.435, P=0.004) and p53 expression was different among the different levels of COX-2 expression (Kruskal–Wallis P=0.001 and P=0.002).
It should be noted that p53 expression was higher in tumors of more advanced stage, and this tendency reached statistical significance (P=0.035) while no statistically significant association was detected between p53 expression and tumor differentiation.
Discussion
The present study represents one of the first systematic morphological investigations of p-IκB-α, pc-JUN, c-FOS—which constitute dynamic markers of NF-κB and AP-1 activation, respectively—PPARγ, and CBP in colon adenocarcinomas. Our analysis demonstrated for the first time a significant induction of p-IκB-α in the vast majority of colon adenocarcinomas, reflecting an important role for p-IκB-α in colorectal carcinogenesis. NF-κB contributes to colorectal carcinogenesis via transcriptional up-regulation of various anti-apoptotic genes and by promotion of metastatic growth responses [35, 36]. Interleukin-1, tumor growth factor-β, lipopolysaccharide, and luminal bacterial components constitute important stimuli that can readily activate NF-κB pathway [21, 22, 37]. Phosphorylation of IκB-α to p-IκB-α is a critical step in the activation of NF-κB pathway and is precisely the point where NSAIDs act to suppress NF-κB signaling [38].
Another important and novel finding of our study was that the reduced expression of PPARγ in colon adenocarcinomas compared to adjacent normal colon was detected in the majority of the patients. PPARγ is a suppressor of colon carcinogenesis, and loss of one PPARγ allele is sufficient to increase sensitivity to chemical carcinogenesis [39]. In this vein, genetic studies have demonstrated that there are heterozygous loss-of-function mutations in the gene encoding PPARγ in approximately 10% of colon cancer patients [40]. Similarly, heterozygous mutations or deletions at the PPARγ locus have been associated with a variety of other malignancies [41, 42]. Inactivation of nuclear receptor coactivators or activation of corepressors or aberrant methylation of the PPARγ gene promoter may also account for the altered expression of PPARγ.
Our study also demonstrated that expression of AP-1 constituents, pc-JUN, and c-FOS was statistically significantly stronger in most colon adenocarcinomas than in normal colonic epithelial cells. Nevertheless, there were some adenocarcinoma cases where down-regulation of pc-JUN (13 cases) and c-FOS expression (13 cases) compared to normal colon was detected. pc-JUN and c-FOS down-regulation was noted mostly in moderately or poorly differentiated adenocarcinomas and adenocarcinomas of advanced stage. As the JNK/pc-JUN pathway has been associated with colonic cell differentiation [14], down-regulation of pc-JUN in these cases may reflect a late loss of differentiation in these adenocarcinomas.
It is important to note that EGF-R expression was increased in colon adenocarcinomas and paralleled both c-FOS and pc-JUN expression. EGF-R activates the membrane-bound GTPase RAS, leading to activation of the ERK and JNK signaling pathways. Our study supports this orchestrated EGF-R, c-FOS, and pc-JUN expression as EGF-R, c-FOS, and pc-JUN were found to be positively correlated to each other. The overexpression of EGF-R in colon carcinomas provides the rationale for the use of targeted therapies against it (i.e., antibodies against EGF-R) or other factors that are downstream of EGF-R in the MAPK pathway.
In accordance with previous data [43], COX-2 overexpression was detected in colon cancer cells in most colon adenocarcinomas. The role of COX-2 in colon carcinogenesis is well established [15]. It has been shown that cox-2 promoter contains NF-κB and cyclic adenosine monophosphate responsive element transcriptional regulatory elements [20]. The positive correlation between p-IκB-α and COX-2 expression and between pc-JUN and COX-2 expression in colon adenocarcinomas indicates that NF-κB and AP-1 are important inducers of cox-2 during colon carcinogenesis. The fact that pc-JUN expression correlated with COX-2 while c-FOS expression did not correlate with COX-2 may reflect the fact that there may be a prevalence of pc-JUN homodimeric complexes comprising active AP-1 responsible for cox-2 up-regulation. CBP paralleled COX-2 expression, suggesting that it may occupy an important role as a transcriptional coactivator of both NF-κB and AP-1 in up-regulation of cox-2. It is important to note also that EGF-R expression correlated positively with COX-2. COX-2 and EGF-R were not expressed in a higher proportion in poorly differentiated tumors, and this reflects the notion that overexpression of these molecules occurs early in colorectal carcinogenesis and remains important throughout the process.
It is notable that an inverse (negative) correlation between p-IκB-α and PPARγ expression and between PPARγ and COX-2 expression was detected in colon adenocarcinomas. A negative cross-talk between PPARγ and NF-κB has already been demonstrated [28, 34]. As PPARγ is down-regulated in colon adenocarcinomas, the negative PPARγ/NF-κB cross talk is abrogated, leading to unopposed NF-κB transcriptional activity and ultimately to up-regulation of COX-2 expression. A negative cross talk between PPARγ and AP-1 has been similarly documented [28, 32, 33]. Therefore, down-regulation of PPARγ in colon adenocarcinomas enhances AP-1 transcriptional activity leading to up-regulation of cox-2 expression. The induction of the CBP transcriptional coactivator further amplifies NF-κB and AP-1 transcriptional activities.
Finally, our finding that p53 expression correlated positively with COX-2 expression has also been documented in other malignancies. Wild type but not mutant p53 markedly suppresses cox-2 transcription by competing with TATA-binding protein for binding to the TATA box [20]. Overexpression of mutant p53 in colon carcinogenesis is associated with induction of COX-2 expression in colon adenocarcinomas, reflecting the fact that the mutant/inactivated p53 fails to down-regulate COX-2 transcription as wild p53 would normally do. It is notable that p53 expression was higher in tumors of more advanced stage and this tendency reached statistical significance.
In conclusion, the present study demonstrated a significant induction of p-IκB-α in colon adenocarcinomas which correlated positively with COX-2 expression. Moreover, overexpression of AP-1 constituents and, particularly, induction of pc-JUN occurred commonly in colorectal carcinogenesis and paralleled COX-2 expression. The down-regulation of PPARγ expression probably attenuates the negative PPARγ/AP-1 and PPARγ/NF-κB cross-talks, leading to strengthening of NF-κB and AP-1 transcriptional activities and up-regulation of cox-2. The induction of CBP transcriptional coactivator further enhances NF-κB and AP-1 transcriptional activities. The present study suggests that p-IκB-α, pc-JUN, and CBP could potentially serve as exciting molecular targets for the design of novel, highly specific anticancer therapies following the paradigm of EGF-R-targeted therapies. The development of PPARγ ligands that selectively inhibit AP-1 or NF-κB activity without stimulating transcription may represent an alternative molecular-targeted strategy against colon carcinogenesis.
References
Shaulian E, Karin M (2001) AP-1 in cell proliferation and survival. Oncogene 20:2390–2400
Karin M, Liu Z, Zandi E (1997) AP-1 function and regulation. Curr Opin Cell Biol 2:240–246
Kyriakis JM, Avruch J (2001) Mammalian mitogen-activated protein kinase signal transduction pathways activated by stress and inflammation. Physiol Rev 81:807–869
Karin M (1995) The regulation of AP-1 activity by mitogen-activated protein kinases. J Biol Chem 270:16483–16486
Whitmarsh AJ, Davis RJ (1996) Transcription factor AP-1 regulation by mitogen-activated protein kinase signal transduction pathways. J Mol Med 74:589–607
Papavassiliou AG, Treier M, Bohmann D (1995) Intramolecular signal transduction in c-Jun. EMBO J 14:2014–2019
Arias J, Alberts AS, Brindle P, Claret FX, Smeal T, Karin M, Feramisco J, Montminy M (1994) Activation of cAMP and mitogen responsive genes relies on a common nuclear factor. Nature 370:226–229
Karamouzis MV, Papadas T, Varakis I, Sotiropoulou-Bonikou G, Papavassiliou AG (2002) Induction of the CBP transcriptional co-activator early during laryngeal carcinogenesis. J Cancer Res Clin Oncol 128:135–140
Shaulian E, Karin M (2002) AP-1 as a regulator of cell life and death. Nat Cell Biol 4:131–136
Eferl R, Wagner EF (2003) AP-1: a double-edged sword in tumorigenesis. Nat Rev Cancer 3:859–868
van Dam H, Castellazzi M (2001) Distinct roles of Jun : Fos and Jun : ATF dimers in oncogenesis. Oncogene 20:2453–2464
Hirano F, Tanada H, Makino Y, Okamoto K, Hiramoto M, Handa H, Makino I (1996) Induction of the transcription factor AP-1 in cultured human colon adenocarcinoma cells following exposure to bile acids. Carcinogenesis 17:427–433
Glinghammar B, Holmberg K, Rafter J (1999) Effects of colonic lumenal components on AP-1-dependent gene transcription in cultured human colon carcinoma cells. Carcinogenesis 20:969–976
Chen A, Davis BH, Bissonnette M, Scaglione-Sewell B, Brasitus TA (1999) 1,25-Dihydroxyvitamin D(3) stimulates activator protein-1-dependent Caco-2 cell differentiation. J Biol Chem 274:35505–35513
Subbaramaiah K, Dannenberg AJ (2003) Cyclooxygenase 2: a molecular target for cancer prevention and treatment. Trends Pharmacol Sci 24:96–102
Dubois RN, Abramson SB, Crofford L, Gupta RA, Simon LS, Van De Putte LB, Lipsky PE (1998) Cyclooxygenase in biology and disease. FASEB J 12:1063–1073
Kosaka T, Miyata A, Ihara H, Hara S, Sugimoto T, Takeda O, Takahashi E, Tanabe T (1994) Characterization of the human gene (PTGS2) encoding prostaglandin-endoperoxide synthase 2. Eur J Biochem 221:889–897
Guo YS, Hellmich MR, Wen XD, Townsend CM (2001) Activator protein-1 transcription factor mediates bombesin-stimulated cyclooxygenase-2 expression in intestinal epithelial cells. J Biol Chem 276:22941–22947
Subbaramaiah K, Norton L, Gerald W, Dannenberg AJ (2002) Cyclooxygenase-2 is overexpressed in HER-2/neu-positive breast cancer: evidence for involvement of AP-1 and PEA3. J Biol Chem 277:18649–18657
Subbaramaiah K, Cole PA, Dannenberg AJ (2002) Retinoids and carnosol suppress cyclooxygenase-2 transcription by CREB-binding protein/p300-dependent and -independent mechanisms. Cancer Res 62:2522–2530
Baeuerle PA, Baltimore D (1996) NF-kappa B: ten years after. Cell 87:13–20
Kojima M, Morisaki T, Izuhara K, Uchiyama A, Matsunari Y, Katano M, Tanaka M (2000) Lipopolysaccharide increases cyclo-oxygenase-2 expression in a colon carcinoma cell line through nuclear factor-kappa B activation. Oncogene 19:1225–1231
Liu W, Reinmuth N, Stoeltzing O, Parikh AA, Tellez C, Williams S, Jung YD, Fan F, Takeda A, Akagi M, Bar-Eli M, Gallick GE, Ellis LM (2003) Cyclooxygenase-2 is up-regulated by interleukin-1 beta in human colorectal cancer cells via multiple signaling pathways. Cancer Res 63:3632–3636
Rayet B, Gelinas C (1999) Aberrant rel/nfkb genes and activity in human cancer. Oncogene 18:6938–6947
Sarraf P, Mueller E, Jones D, King FJ, DeAngelo DJ, Partridge JB, Holden SA, Chen LB, Singer S, Fletcher C, Spiegelman B (1998) Differentiation and reversal of malignant changes in colon cancer through PPARgamma. Nat Med 4:1046–1052
Subbaramaiah K, Lin DT, Hart JC, Dannenberg AJ (2001) Peroxisome proliferator-activated receptor gamma ligands suppress the transcriptional activation of cyclooxygenase-2. Evidence for involvement of activator protein-1 and CREB-binding protein/p300. J Biol Chem 276:12440–12448
Yang WL, Frucht H (2001) Activation of the PPAR pathway induces apoptosis and COX-2 inhibition in HT-29 human colon cancer cells. Carcinogenesis 22:1379–1383
Su CG, Wen X, Bailey ST, Jiang W, Rangwala SM, Keilbaugh SA, Flanigan A, Murthy S, Lazar MA, Wu GD (1999) A novel therapy for colitis utilizing PPAR-gamma ligands to inhibit the epithelial inflammatory response. J Clin Invest 104:383–389
Blanquart C, Barbier O, Fruchart JC, Staels B, Glineur C (2003) Peroxisome proliferator-activated receptors: regulation of transcriptional activities and roles in inflammation. J Steroid Biochem Mol Biol 85:267–273
Law RE, Meehan WP, Xi XP, Graf K, Wuthrich DA, Coats W, Faxon D, Hsueh WA (1996) Troglitazone inhibits vascular smooth muscle cell growth and intimal hyperplasia. J Clin Invest 98:1897–1905
Chung SW, Kang BY, Kim SH, Pak YK, Cho D, Trinchieri G, Kim TS (2000) Oxidized low density lipoprotein inhibits interleukin-12 production in lipopolysaccharide-activated mouse macrophages via direct interactions between peroxisome proliferator-activated receptor-gamma and nuclear factor-kappa B. J Biol Chem 275:32681–32687
Subbaramaiah K, Altorki N, Chung WJ, Mestre JR, Sampat A, Dannenberg AJ (1999) Inhibition of cyclooxygenase-2 gene expression by p53. J Biol Chem 274:10911–10915
Leung WK, To KF, Ng YP, Lee TL, Lau JY, Chan FK, Ng EK, Chung SC, Sung JJ (2001) Association between cyclo-oxygenase-2 overexpression and missense p53 mutations in gastric cancer. Br J Cancer 84:335–339
Ristimaki A, Sivula A, Lundin J, Lundin M, Salminen T, Haglund C, Joensuu H, Isola J (2002) Prognostic significance of elevated cyclooxygenase-2 expression in breast cancer. Cancer Res 62:632–635
Luo JL, Maeda S, Hsu LC, Yagita H, Karin M (2004) Inhibition of NF-kappaB in cancer cells converts inflammation-induced tumor growth mediated by TNFalpha to TRAIL-mediated tumor regression. Cancer Cell 6:297–305
Din FV, Dunlop MG, Stark LA (2004) Evidence for colorectal cancer cell specificity of aspirin effects on NF kappa B signalling and apoptosis. Br J Cancer 91(2):381–388
Lu T, Burdelya LG, Swiatkowski SM, Boiko AD, Howe PH, Stark GR, Gudkov AV (2004) Secreted transforming growth factor beta2 activates NF-kappaB, blocks apoptosis, and is essential for the survival of some tumor cells. Proc Natl Acad Sci U S A 101:7112–7117
Yin MJ, Yamamoto Y, Gaynor RB (1998) The anti-inflammatory agents aspirin and salicylate inhibit the activity of I(kappa)B kinase-beta. Nature 396:77–80
Girnun GD, Smith WM, Drori S, Sarraf P, Mueller E, Eng C, Nambiar P, Rosenberg DW, Bronson RT, Edelmann W, Kucherlapati R, Gonzalez FJ, Spiegelman BM (2002) APC-dependent suppression of colon carcinogenesis by PPARgamma. Proc Natl Acad Sci U S A 99:13771–13776
Sarraf P, Mueller E, Smith WM, Wright HM, Kum JB, Aaltonen LA, de la Chapelle A, Spiegelman BM, Eng C (1999) Loss-of-function mutations in PPAR gamma associated with human colon cancer. Mol Cell 3:799–804
Smith WM, Zhou XP, Kurose K, Gao X, Latif F, Kroll T, Sugano K, Cannistra SA, Clinton SK, Maher ER, Prior TW, Eng C (2001) Opposite association of two PPARG variants with cancer: overrepresentation of H449H in endometrial carcinoma cases and underrepresentation of P12A in renal cell carcinoma cases. Hum Genet 109:146–151
Zhou XP, Smith WM, Gimm O, Mueller E, Gao X, Sarraf P, Prior TW, Plass C, von Deimling A, Black PM, Yates AJ, Eng C (2000) Over-representation of PPARgamma sequence variants in sporadic cases of glioblastoma multiforme: preliminary evidence for common low penetrance modifiers for brain tumour risk in the general population. J Med Genet 37:410–414
Soslow RA, Dannenberg AJ, Rush D, Woerner BM, Khan KN, Masferrer J, Koki AT (2000) COX-2 is expressed in human pulmonary, colonic, and mammary tumors. Cancer 89:2637–2645
Acknowledgements
We thank H. Nikolopoulou, N. Mpeka, and F. Chrysanthopoulos, technicians at the Pathology Department of Aeghion General Hospital, for their help and enthusiastic work. P. A. Konstantinopoulos and G. P. Vandoros contributed equally to this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Konstantinopoulos, P.A., Vandoros, G.P., Sotiropoulou-Bonikou, G. et al. NF-κB/PPARγ and/or AP-1/PPARγ ‘on/off’ switches and induction of CBP in colon adenocarcinomas: correlation with COX-2 expression. Int J Colorectal Dis 22, 57–68 (2007). https://doi.org/10.1007/s00384-006-0112-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-006-0112-y