Abstract
In hereditary nonpolyposis colorectal cancer (HNPCC) syndrome, more than 90% of the carcinomas show microsatellite instability (MSI) due to a loss of mismatch repair (MMR) function. Although adenomas are very common in HNPCC and demonstrate an accelerated adenoma–carcinoma sequence, data about the prevalence and development of MSI in these early neoplastic lesions are lacking. To determine whether MSI and loss of MMR-protein expression are already present in early stages of tumorigenesis and could therefore be used as a screening tool to identify HNPCC patients before they develop an invasive carcinoma, we analyzed 71 adenomas of 36 HNPCC patients during a 5-year follow-up study. These 36 patients were part of a cohort of 122 HNPCC patients who were investigated at the Institute of Pathology, Klinikum Kassel, as part of the multicentric German HNPCC Consortium, which currently serves more than 2,880 registered families. The diagnosis of HNPCC was based either on the detection of a pathogenic germline mutation in the MSH2, MLH1, or MSH6 genes or in cases where a pathogenic mutation was not found; diagnosis of HNPCC was made, because all patients fulfilled the Amsterdam or Bethesda criteria and revealed a high degree of MSI (MSI-H) as well as loss of one of the MMR proteins by IHC in the cancer tissue. We found that most adenomas (58/71) were MSI-H and had loss of MMR-protein expression. Of the 71 adenomas, 3 were MSI-H with expression of all MMR proteins, and 3 out of 71 displayed loss of a MMR protein with the microsatellites being classified as microsatellite stable (MSS). However, 7 of the 31 adenomas that were located more than 5 cm away from the carcinoma revealed an MSS status (n=6) or low in MSI (n=1) and expressed all MMR proteins. In summary, a significant percentage of HNPCC-associated adenomas (7/31, 22.6%) developing at a distance of more than 5 cm from the corresponding carcinoma did not show the MSI-H MMR-deficient phenotype and expressed all MMR genes. To our knowledge, this is the first study that shows that in most HNPCC patients, the mutator pathway is already detectable in adenomas, but MMR-proficient adenomas can also be found. Therefore, screening for MMR deficiency should not be applied routinely in adenomas with the goal to identify HNPCC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Abnormal growth is one characteristic of cancer that is caused by an imbalance between cell proliferation and cell death. During tumorigenesis of colorectal cancer, a stepwise inactivation of tumor suppressor genes and activation of oncogenes drive the progression from a dysplastic lesion to invasive cancer, which manifests grossly as a polyploid or flat tumor with subsequent invasion and metastasis.
Hereditary nonpolyposis colorectal cancer (HNPCC) is a highly penetrant, autosomal dominant disorder that accounts for approximately 2–4% of all colorectal carcinomas [1–4]. In HNPCC, the underlying defect has been identified as mutations in the DNA mismatch repair (MMR) system. So far, pathogenic mutations have been found in the MMR genes MLH1, MSH2, PMS2, and MSH6 [5–9]. Lack of MMR results in the so-called “mutator phenotype,” which leads to increased mutation rates, accumulation of mutations in tumor suppressor genes and oncogenes, and ultimately genomic instability [10]. More than 90% of HNPCC carcinomas show a high degree of microsatellite instability (MSI-H), in contrast to only 10–15% of sporadic colorectal cancers [11–13]. The latter become MMR deficient usually through MLH1 promoter methylation [14].
Both clustering of malignant tumors in a single family and early onset of disease are highly suggestive of a hereditary condition and can be used as clinical criteria to screen for patients at risk. Identification of patients with a hereditary cancer predisposition provides a possibility to detect tumors at an early stage or even to offer prophylactic surgery before the onset of invasive cancer growth [3, 5].
Because MSI-H is the molecular hallmark of cancers in HNPCC patients, the identification of an MSI-H status in carcinomas has a high impact for recognition as well as management of the individual patient [15–17]. Additional immunohistochemical staining for MMR proteins is recommended to pinpoint the gene that is most probably mutated. In case of a mutation, the nuclear staining pattern is typically negative or less intense [18–22].
Ideally, the diagnosis of HNPCC should be made before the development of an invasive tumor and should be accompanied by a rigorous surveillance program and possibly prophylactic surgery. However, although adenomas are very common in HNPCC and demonstrate an accelerated progression to carcinoma, data about the prevalence and development of MSI-H in these early neoplastic lesions are lacking [23–26]. The aim of the study was therefore to investigate, whether MSI-H and absence of MMR proteins are already detectable in adenomas of MMR-deficient patients and whether these assays could help to identify HNPCC patients before the onset of fully developed invasive carcinomas.
Materials and methods
Patients and tumors
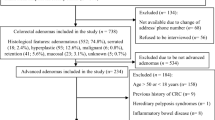
This study is based on 122 index patients presenting with invasive cancers, who were investigated by the Pathology Reference Center, Klinikum Kassel, within the German Multicenter Study Group for HNPCC supported by the Deutsche Krebshilfe (German Cancer Aid). After resection of the cancer, each patient was followed-up over a period of up to 5 years (median 3.1 years). All cancers and precancerous lesions obtained either via surgery or via colonoscopy during surveillance were recorded, staged, and graded according to the recommendations of the WHO [27]. Of 122 patients, 36 were found to harbor additional adenomas either synchronously or metachronously.
For all 36 patients, a mutation search in MSH2, MLH1, and MSH6 was done. A pathogenic germline mutation was found in 14 patients. The other 22 patients were classified as HNPCC because they fulfilled the Amsterdam/Bethesda criteria and revealed MSI-H as well as immunohistochemical loss of MMR-protein expression in the tumor. In case of loss of MLH1-protein expression, only cases with a strong family history were included in the study to exclude sporadic tumors lacking MLH1 due to promoter hypermethylation. All tumor specimens and blood samples were analyzed after obtaining informed consent.
Adenomas were divided into three groups with regard to their location and occurrence related to the corresponding carcinoma; “group 1” consisted of adenomas contiguous with the carcinoma (carcinoma ex adenoma); “group 2” adenomas were located less than 5 cm away from the carcinoma and all detected at the same time as the cancer; “group 3” adenomas developed at a distance of more than 5 cm away from the cancer either synchronously (a) or metachronously (b).
Microdissection and DNA extraction
Five-micron sections were cut from paraffin-embedded carcinoma, adenoma, and corresponding normal tissue, mounted on glass slides, and stained with hematoxylin and eosin (H & E) or periodic acid Schiff (PAS) reagent. Areas of interest containing at least 80% of neoplastic cells were selected by a pathologist for adenoma and carcinoma, respectively. These regions were then scraped off the slide and underwent proteinase K digestion at a final concentration of 2 μg/ml (Qiagen, Hilden, Germany). Normal DNA was extracted from microdissected normal mucosa. DNA was extracted with the QIAamp DNA Mini Kit (Qiagen) according to the manufacturer’s recommendations and purified with the PCR Template Preparation Kit (Roche, Mannheim, Germany).
Additionally, laser microdissection was performed on all adenomas. Sections of the same paraffin blocks as before were mounted onto a polyethylene membrane attached to a glass slide with rubber cement (Fixogum, Marabuwerke, Tamm, Germany). Slides were deparaffinized in xylole, rehydrated in descending alcohols, and stained with H & E. Laser microdissection was performed using a Leica AS LMD system (Leica Microsystems GmbH, Wetzlar, Germany). About 100–200 epithelial cells were harvested for each analysis. Cell lysis was performed by dispensing 20 μl lysis buffer into each cap. The buffer consisted of 2 μg/ml proteinase K (Roche), 0.5% Tween 20 (Merck, Darmstadt, Germany), and 1× Taq PCR Buffer (Roche). After digestion for 18 h at 50°C, proteinase K was inactivated by incubation at 94°C for 10 min.
Analysis of MSI
In accordance with the recommendations by the National Cancer Institute (NCI) and the ICG-HNPCC [28–30], five microsatellite loci were used in all tumor lesions both for manual and laser-based dissection to detect MSI: two loci with mononucleotide runs (BAT25, BAT26) and three loci with CA dinucleotide repeats (D2S123, D5S346, D17S250). In addition, samples obtained by laser microdissection were also tested for instability at BAT40. The primer sequences of these microsatellite loci have been reported elsewhere [17]. PCR amplifications were performed in an Eppendorf Mastercycler Gradient (Eppendorf, Hamburg, Germany). Primers were 5'-labeled with HEX, FAM, or TET (PE Applied Biosystems, Foster City, CA). DNA was amplified in a standard reaction mix with cycling conditions using AmpliTaq Gold (PE Applied Biosystems). PCR products were run on an ABI PRISM 310 Genetic Analyzer (PE Applied Biosystems) according to the manufacturer’s instructions, and the microsatellite status was analyzed using the GeneScan fragment analysis software (GeneScan, PE Applied Biosystems). Only cases showing distinct additional peaks or shifted peaks in tumor tissue DNA compared with normal tissue DNA were interpreted as MSI.
The microsatellite status of each sample was determined based on the percentage of instable loci, with MSI-H being defined as 30% or more instable markers and MSI-low (MSI-L) as less than 30% of markers exhibiting instability. A sample was classified as microsatellite stable (MSS) when no MSI was found.
Immunohistochemistry
As described previously [31], sections were stained with primary antibody for 4 h at room temperature. Antibodies were diluted with Antibody Diluent (DAKO, Hamburg, Germany) and applied overnight using the Tecan Immunostainer Genesis RSP 200 as follows: MLH1 (clone G 168-15, Pharmingen, San Diego, CA) 1:100, MSH2 (clone AB-2, Calbiochem, La Jolla, CA) 1:50, MSH6 (clone 44, Becton-Dickinson, San Jose, CA) 1:50, and PMS2 (clone A16-4, Pharmingen) 1:25. After incubation with 120 μl anti-mouse EnVision HRP (DAKO) for 30 min, detection was done with 120 μl/slide DAB solution (DAKO; 1:50 dilution in substrate buffer) for 10 min. The reaction was stopped with 100 μl PBS/Tween for 20 min, followed by washing with 1,400 μl PBS/Tween for 7 min. Slides were counterstained briefly with hematoxylin.
Only slides with distinct positive nuclear staining in the basal crypt cells of normal mucosa, stromal, as well as inflammatory cells were evaluated. Loss of MMR-protein expression within the neoplastic lesions was defined as complete if less than 10% of tumor cells were stained. Incomplete loss (10–50% stained cells) or only focal staining (cohesive nests of stained tumor cells) was recorded as positive (+) [31].
Results
Number and type of adenomas
Seventy-one adenomas were found in 36 patients. During the follow-up period, 22 patients developed only one adenoma, 9 patients had two adenomas, and 5 patients were found to have three or more adenomas. Of these 71, 59 were synchronous with the cancer and 12 developed metachronously. The histological types were tubular (56/71), tubulo-villous (14/71), and serrated adenoma (1/71).
Twelve adenomas were contiguous with the carcinoma (carcinoma ex adenoma; group 1); 28 of the synchronous adenomas were less than 5 cm away but were clearly separate from the carcinoma (group 2). Of 31 adenomas at a distance of more than 5 cm from the carcinoma, 19 were synchronous (group 3a) and 12 were metachronous (group 3b).
MSI in adenomas and corresponding carcinomas
All (12/12) group 1 adenomas (100%) were MSI-H, as were the corresponding carcinomas that arose from the adenomas. Of the 28 group 2 adenomas, 25 (89.3%) were MSI-H, as were the carcinomas of these patients. The remaining 3 adenomas were MSS, which was confirmed by laser microdissection.
Sixteen out of 19 group 3a adenomas (84.2%) and 8 out of 12 group 3b adenomas (66.7%) were MSI-H. The remaining 3 and 4 adenomas from these groups, respectively, were MSS. These results were also confirmed by laser microdissection.
MMR-protein expression in adenomas and corresponding carcinomas
All (12/12) group 1 adenomas showed loss of the same MMR protein as the corresponding carcinomas. In addition, all (28/28) group 2 adenomas displayed loss of the same MMR proteins as the corresponding carcinomas.
Ten out of 19 group 3a adenomas and 8 out of 12 group 3b adenomas showed loss of the same MMR protein as the corresponding carcinomas. The remaining 9 group 3a and 4 group 3b adenomas stained positive for all examined MMR proteins, indicating the presence of wild-type protein.
Combined MSI and MMR-protein expression status in adenomas and corresponding carcinomas
Overall, the microsatellite status and immunohistochemical profile of group 1 and 2 adenomas were identical to their corresponding cancers. However, there were three cases in group 2 that showed loss of the same MMR protein as the corresponding tumor in spite of an MSS status. This finding would still be viewed as in indication of MMR deficiency in these adenomas (Fig. 1).
However, 3/19 group 3a adenomas and 4/12 group 3b adenomas showed no evidence of MMR deficiency (Fig. 1). All of these lesions expressed the MMR proteins. The 3 group 3a adenomas and 4 group 3b adenomas were MSS, and 1 group 3b adenoma there was MSI-L. Of note, 2 of these MMR-proficient adenomas were found in patients who had other MMR-deficient adenomas (patients 8 and 22, Table 1), and two patients had proven MMR gene mutations (patients 15 and 22, Table 1; Fig. 2).
Results of the immunohistochemical staining of two adenomas of one HNPCC patient. The synchronous cancer is negative for MSH2 and shows MSI-H (data not shown); the synchronous adenoma shows the same expression pattern, whereas the metachronous adenoma stains positive for all MMR proteins and shows no MSI
Discussion
Adenomas are well established as precursor lesions of colorectal cancer. In HNPCC, an earlier onset of adenomas and a faster progression to cancer have been described [32, 33]. The present study attempts to assess the diagnostic value of MSI testing and immunohistochemical analysis of MMR-protein expression for the detection of HNPCC in precancerous lesions in a well-characterized cohort of HNPCC patients.
As expected, in patients with an MMR deficiency, the vast majority of HNPCC patients display MSI-H and loss of one of the MMR proteins by IHC even in the precancerous adenoma stage. This finding indicates that the MMR deficiency is an early event in the molecular carcinogenesis of tumors that follow the mutator pathway.
Three adenomas in group 2 had loss of expression of one of the MMR proteins, even though microsatellite analysis revealed no instability. This finding points to an MMR-protein deficiency not yet fully manifested as MSI-H. We reported previously that early or low-grade adenomas may only show MSS or MSI-L, especially when they are not laser-microdissected [31, 34]. However, we were able to confirm the MSS status after laser microdissection in these cases. All three of these adenomas were low grade (classified with dysplasia grade 1 or 2; patients 11, 16, and 36). It can be assumed that these adenomas, had they not been removed, would have ultimately developed MSI-H.
Surprisingly, we observed that a significant percentage of adenomas (7/31 in groups 3a and 3b, 22%) differ from the carcinoma in their microsatellite status and MMR-protein expression profile. We found that they were microsatellite stable and revealed no evidence of a loss or reduction in MMR gene expression. Again, we used laser capture microdissection instead of manual microdissection [31, 34] to rule out the possibility of false-negative MSI results due to intralesional heterogeneity [31].
Interestingly, two of these apparently MMR-proficient adenomas (patients 8 and 22, Table 1) were found in patients who had other MMR-deficient adenomas that had the same MSI and IHC results as the carcinoma. Two patients with apparently MMR-proficient adenomas had germline mutations of an MMR gene (patients 15 and 22, Table 1). Even though it is possible that these lesions would manifest the hallmarks of MMR deficiency later as they progress, especially as most of them were classified with dysplasia grade 1 or 2, it seems reasonable to assume that HNPCC patients can also develop adenomas that do not follow the mutator pathway [35].
Concluding from our studies, we emphasize that immunohistochemical analysis is a powerful tool in the assessment of MMR, especially in early lesions [36–38], as exemplified in three of our group 2 cases that were MSS but revealed a loss of MMR-protein expression. This phenomenon is most likely due to evolving instability in only a few cell clones particularly in early adenomas [31].
At the same time, we further conclude that exclusive use of immunohistochemical staining to identify patients at risk for HNPCC seems to be insufficient. Six adenomas in group 3 showed normal MMR-protein expression, even though they were MSI-H. One possible explanation in these cases would be a mutation that results in expression of a nonfunctional or of a truncated MMR protein that can still be detected by IHC.
In summary, the identification of HNPCC-associated adenomas is still difficult and, hence, needs analyses and interpretation from specialized centers that interpret the results of the histological and molecular analyses in the context of the patient’s medical history and family history.
For patient management, it is essential to include all HNPCC-associated carcinomas as well as the adenomas for the correct interpretation of the family history. False-positive results may lead to overtreatment and unnecessary psychological stress not only for the individual but also for the family, not to mention the fact that they are time-consuming and costly. More importantly, false-negative results may lead to the exclusion of an HNPCC patient from the more rigorous surveillance program and, consequently, may result in failure to detect cancer development at an early stage.
Our study clearly demonstrates that for detection of HNPCC patients, MSI and IHC results obtained from adenomas must be interpreted very cautiously. A negative MSI test result or presence of all MMR proteins in an adenoma should not be used to exclude a patient from intensified clinical cancer screening programs if there is any clinical suspicion for HNPCC, based on age at presentation, medical history, or family history. In conclusion, we support the recommendation in the revised Bethesda guidelines to exclude predictive MSI testing of adenomas as a reliable tool to screen for HNPCC patients [30].
References
Aaltonen LA, Salovaara R, Kristo P, Canzian F, Hemminki A, Peltomäki P, Chadwick RB, Kääriäinen H, Eskelinen M, Järvinen H, Mecklin JP, Chapelle de la A et al (1998) Incidence of hereditary nonpolyposis colorectal cancer and the feasibility of molecular screening for the disease. N Engl J Med 338:1481–1487
Evans DG, Walsh S, Jeacock J (1997) Incidence of hereditary non-polyposis colorectal cancer in a population-based study of 1137 consecutive cases of colorectal cancer. Br J Surg 84:1281–1285
Lynch HT, Chapelle de la A (2003) Hereditary colorectal cancer. N Engl J Med 348:919–932
Salovaara R, Loukola A, Kristo P, Kääriäinen H, Ahtola H, Eskelinen M, Härkönen N, Julkunen R, Kangas E, Ojala S, Tulikoura J, Valkamo E, Järvinen H, Mecklin JP, Aaltonen LA, de la Chapelle A (2000) Population-based molecular detection of hereditary nonpolyposis colorectal cancer. J Clin Oncol 11:2193–2200
Aarnio M, Sankila R, Pukkala E, Salovaara R, Aaltonen LA, de la Chapelle A, Peltomäki P, Mecklin JP, Jarvin HJ (1999) Cancer risk in mutation carriers of DNA-mismatch-repair genes. Int J Cancer 8:214–218
Holmberg M, Kristo P, Chadwicks RB, Mecklin JP, Jarvinen H, de la Chapelle A, Nystrom-Lahti M, Peltomaki P (1998) Mutation sharing, predominant involvement of the MLH1 gene and description of four novel mutations in hereditary nonpolyposis colorectal cancer. Mutations in brief no. 144. Hum Mutat 1:482–486 (online)
Mangold E, Pagenstecher C, Friedl W, Mathiak M, Buettner R, Engel C, Loeffler M, Holinski-Feder E, Muller-Koch Y, Keller G, Schackert HK, Kruger S, Goecke T, Moeslein G, Kloor M, Gebert J, Kunstmann E, Schulmann K, Ruschoff J, Propping P (2004) Spectrum and frequencies of mutations in MSH2 and MLH1 identified in 1721 German families suspected of hereditary nonpolyposis colorectal cancer. Int J Cancer 116(5):692–702
Plaschke J, Krüger ST, Pistorius ST, Theissig F, Saeger HD, Schackert HK (2002) Involvement of hMSH6 in the development of hereditary and sporadic colorectal cancer revealed by immunostaining is based on germline mutations, but rarely on somatic inactivation. Int J Cancer 97:643–648
Peltomäki P (2001) Deficient DNA mismatch repair: a common etiologic factor for colon cancer. Hum Mol Genet 10:735–740
Loeb LA (1991) Mutator phenotype may be required for multistage carcinogenesis. Cancer Res 51:3075–3079
Thibodeau SN, Bren G, Schaid D (1993) Microsatellite instability in cancer of the proximal colon. Science 260:816–819
Peltomäki P (2001) Deficient DNA mismatch repair: a common etiologic factor for colon cancer. Hum Mol Genet 10:735–740
Ionov Y, Peinado MA, Malkhosyan S, Shibata D, Perucho M (1993) Ubiquitous somatic mutations in simple repeated sequences reveal a new mechanism for colonic carcinogenesis. Nature 363:558–561
Cunningham JM, Christensen ER, Tester DJ, Kim CY, Roche PC, Burgart LJ, Thibodeau SN (1998) Hypermethylation of the hMLH1 promoter in colon cancer with microsatellite instability. Cancer Res 58:3455–3460
Lamberti C, Kruse R, Ruelfs C, Caspari R, Wang Y, Jungck M, Mathiak M, Malayeri HR, Friedl W, Sauerbruch T, Propping P (1999) Microsatellite instability—a useful diagnostic tool to select patients at high risk for hereditary non-polyposis colorectal cancer: a study in different groups of patients with colorectal cancer. Gut 44:839–843
Loukola A, Eklin K, Laiho P, Salovaara R, Kristo P, Järvinen H, Mecklin JP, Launonen V, Aaltonen LA (2001) Microsatellite marker analysis in screening for hereditary nonpolyposis colorectal cancer (HNPCC). Cancer Res 61:4545–4549
Rüschoff J, Bocker T, Schlegel J, Stamm G, Hofstaedter F (1995) Microsatellite instability: new aspects in the carcinogenesis of colorectal carcinoma. Virchows Arch 426:215–222
Lanza G, Gafà R, Maestri I, Santini A, Matteuzzi M, Cavazzini L (2002) Immunohistochemical pattern of MLH1/MSH2 expression is related to clinical and pathological features in colorectal adenocarcinomas with microsatellite instability. Mod Pathol 15:741–749
Jass JR (2000) hMLH1 and hMSH2 immunostaining in colorectal cancer. Gut 47:315–316
Müller W, Burgart LJ, Krause-Paulus R, Thibodeau SN, Almeida M, Bocker Edmonston T, Boland CR, Sutter C, Jass JR, Lindblom A, Lubinski J, MacDermot K, Sanders DSA, Morreau H, Müller A, Oliani C, Orntoft T, Ponz De Leon M, Rosty C, Rodriguez-Bigas M, Rüschoff J, Ruszkiewicz A, Sabourin J, Salovaara R, Möslein G; ICG-HNPCC (2001) The reliability of immunohistochemistry as a prescreening method for the diagnosis of hereditary nonpolyposis colorectal cancer (HNPCC)—results of an international collaborative study. Fam Cancer 1:87–92
Thibodeau SN, French AJ, Roche PC, Roche PC, Cunningham JM, Tester DJ, Lindor NM, Moslein G, Baker SM, Liskay RM, Burgart LJ, Honchel R, Halling KC (1996) Altered expression of hMSH2 and hMLH1 in tumors with microsatellite instability and genetic alterations in mismatch repair genes. Cancer Res 56:4836–4840
Gryfe R, Gallinger S (2001) Microsatellite instability, mismatch repair deficiency, and colorectal cancer. Surgery 130:17–20
Aaltonen LA, Peltomäki P, Mecklin JP, Jarvinen H, Jass JR, Green JS, Lynch HT, Watson P, Tallqvist G, Juhola M (1994) Replication errors in benign and malignant tumors from hereditary nonpolyposis colorectal patients. Cancer Res 54:1645–1648
Loukola A, Salovaara R, Kristo P, Moisio A-L, Kääriäinen H, Ahtola H, Eskelinen M, Härkönen N, Julkunen R, Kangas E, Ojala S, Tulikoura J, Valkamo E, Järvinen H, Mecklin J-P, de la Chapelle A, Aaltonen LA (1999) Microsatellite instability in adenomas as a marker for hereditary nonpolyposis colorectal cancer. Am J Pathol 155:1849–1853
Young J, Leggett B, Gustafson C, Ward M, Searle J, Thomas L, Buttenshaw R, Chenevix-Trench G (1993) Genomic instability occurs in colorectal carcinomas but not in adenomas. Hum Mutat 2:351–354
Jacoby RF, Marshall DJ, Kailas S, Schlack S, Harms B, Love R (1995) Genetic instability associated with adenoma to carcinoma progression in hereditary nonpolyposis colon cancer. Gastroenterology 109:73–82
Hamilton SR, Aaltonen LA (eds) (2000) Pathology and genetics of tumours of the digestive system. World health organization classification of tumours. IARC Press, Lyon
Vasen HFA, Watson P, Mecklin J-P, Lynch HT, the ICG-HNPCC (1999) New clinical criteria for hereditary nonpolyposis colorectal cancer (HNPCC, Lynch syndrome) proposed by the international collaborative group on HNPCC. Gastroenterology 116:1453–1456
Boland CR, Thibodeau SN, Hamilton SR, Sidransky D, Eshleman JR, Burt RW, Meltzer SJ, Rodriguez-Bigas MA, Fodde R, Ranzani GN, Srivastava S (1998) A National Cancer Institute workshop on microsatellite instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res 58:5248–5257
Umar A, Boland CR, Terdiman JP, Syngal S, Chapelle de la A, Rüschoff J, Fishel R, Lindor NM, Burgart LJ, Hamelin R, Hamilton SR, Hiatt RA, Jass J, Lindblom A, Lynch HT, Peltomaki P, Ramsey SD, Rodriguez-Bigas MA, Vasen HFA, Hawk ET, Barett JC, Freedman AN, Srivastava S (1999) New clinical criteria for Hereditary nonpolyposis colorectal cancer (HNPCC, Lynch syndrome) proposed by the international collaborative group on HNPCC. Gastroenterology 116:1453–1456
Müller A, Giuffre G, Bocker Edmonston T, Mathiak M, Roggendorf B, Heinmöller E, Brodegger T, Tuccari G, Mangold E, Buettner R, Rüschoff J; German HNPCC Consortium, German Cancer Aid (Deutsche Krebshilfe) (2004) Challenges and pitfalls in HNPCC screening by microsatellite analysis and immunohistochemistry. J Mol Diagn 6:308–315
Jass JR, Stewart SM, Stewart J, Lane MR (1994) Hereditary non-polyposis colorectal cancer: morphologies, genes and mutations. Mutat Res 290:125–133
Rijcken FE, Hollema H, Kleibeuker JH (2002) Proximal adenomas in hereditary non-polyposis colorectal cancer prone to rapid malignant transformation. Gut 50:382–386
Heinmöller E, Renke B, Beyser K, Dietmaier W, Langner C, Rüschoff J (2001) Pitfalls in diagnostic molecular pathology—significance of sampling error. Virchows Arch 439:504–511
Giuffre G, Müller A, Brodegger T, Bocker Edmonston T, Gebert J, Kloor M, Dietmaier W, Kullmann F, Büttner R, Tuccari G, Rüschoff J; German HNPCC Consortium (2005) Microsatellite analysis of hereditary nonpolyposis colorectal cancer-associated colorectal adenomas by laser-assisted microdissection: correlation with mismatch repair protein expression provides new insights in early steps of tumorigenesis. J Mol Diagn 7:160–170
Wahlberg SS, Schmeits J, Thomas G, Loda M, Garber J, Syngal S (2002) Evaluation of microsatellite instability and immunohistochemistry for the prediction of germ-line MSH2 and MLH1 mutations in hereditary nonpolyposis colon cancer families. Cancer Res 62:3485–3492
Lanza G, Gafà R, Maestri I, Santini A, Matteuzzi M, Cavazzini L (2002) Immunohistochemical pattern of MLH1/MSH2 expression is related to clinical and pathological features in colorectal adenocarcinomas with microsatellite instability. Mod Pathol 15:741–749
Pedroni M, Sal E, Scarselli A, Borghi F, Menigatti M, Benatti P, Percesepe A, Rossi G, Foroni M, Losi L, DiGregorio C, De Pol A, Nascimbeni R, Di Betta E, Salerni B, Ponz de Leon M, Roncucci L (2001) Microsatellite instability and mismatch-repair protein expression in hereditary and sporadic colorectal carcinogenesis. Cancer Res 61:896–899
Acknowledgements
This work was supported by the German Cancer Aid (Deutsche Krebshilfe) to J.R. and R.B. (grant 70-2401-Rü), the Deutsche Forschungsgemeinschaft to R.B. (Bu 672/10-1, 10-2), the German Ministry for Education and Research (BMBF) to J.R. (grant AN 020113007601).
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
An invited commentary on this paper is available at http://dx.doi.org/10.1007/s00384-005-0081-6
See Appendix A for a list of the members of this consortium.
Appendix
Appendix
The German HNPCC Consortium consists of the following centers (in alphabetical order): clinical centers in Bochum (in addition to the following authors: Jörg T. Epplen, Stefan Hahn, Erdmute Kunstmann, Christian Pox, and Jörg Willert), Bonn (in addition to the following authors: Elisabeth Mangold, Constanze Pagenstecher, Waltraut Friedl, Holger Lauschke, Andreas Hirner, Christof Lamberti, Peter Propping, and Tilman Sauerbruch), Düsseldorf (in addition to author PD G. Möslein, M.D.), Dresden (in addition to the following authors: Daniela E. Aust, Friedrich Balck, Ruth Höhl, Friedmar R. Kreuz, Stefan Krüger, Steffen R. Pistorius, and Jens Plaschke), Heidelberg (in addition to author Prof. Magnus von Knebel-Döberitz), München-Regensburg (in addition to the following authors: Wolfgang Dietmaier, Reinhard Kopp, Peter Lohse, Michael Muders, Yvonne Müller-Koch, and Holger Vogelsang), center for reference pathology Kassel (in addition to author Thomas Brodegger), and center for documentation and biometry in Leipzig (in addition to the following authors: Christoph Engel, Jochen Forberg, Marlies Herold, and Markus Löffler).
Rights and permissions
About this article
Cite this article
German HNPCC Consortium., Müller, A., Beckmann, C. et al. Prevalence of the mismatch-repair-deficient phenotype in colonic adenomas arising in HNPCC patients: results of a 5-year follow-up study. Int J Colorectal Dis 21, 632–641 (2006). https://doi.org/10.1007/s00384-005-0073-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-005-0073-6