Abstract
Background/Aims
Mortality in mesenteric ischaemia can be reduced by an optimised extent of resection. Up to now, no technique supplementing a surgeon's experience has achieved clinical acceptance. Besides a qualitative interpretation, the new technique of computer-assisted laser-fluorescence videography affords quantification of staining intensities. The aim of this study was to investigate the scientific value of this technique in mesenteric ischaemia in a rabbit model of controlled mesenteric ischaemia and reperfusion.
Methods
We used an established rabbit model of mesenteric ischaemia (group I, n=6) and reperfusion (group II, n=6). In each animal, three loops (each of 10 cm) of the small intestine were clamped (group I, 40 min; group II, 60 and 20 min reperfusion). For further evaluation, all loops were divided into five segments of 2×2 cm (total number of investigated areas, n=180). Measurement of vascular patency was performed by laser-fluorescence videography (pixel intensity per second). As standard, we used radioactive microspheres (impulse per minute per gram). In addition, the extent of ischaemic tissue damage was identified by histological examination. Statistical data were analysed by using regression analysis to define the regression coefficient r.
Results/Findings
Laser-fluorescence videography and the microsphere technique demonstrated a close and linear correlation: ischaemic segments, r=0.90±0.07; reperfusion segments, r=0.85±0.02; overall, r=0.92±0.07. There was no reproducible correlation to cellular damage in histology.
Interpretation/Conclusion
Computer-assisted laser-fluorescence videography is a feasible, reliable, and valid experimental method for the detection of mesenteric blood supply and intestinal microcirculation. Clinical application is conceivable in mesenteric ischaemia and infarction as well as the operative transposition of intestine. As limiting values to identify the irreversible necrosis are not yet defined, further studies have to analyse the clinical impact more precisely.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mesenteric ischaemia still is a challenging entity in diagnostics and therapy. Despite technical progress, current studies persistently reveal high rates of mortality ranging from 24 to 96% [1–3].
Besides a prompt diagnosis, an optimised extent of intestinal resection can reduce mortality. However, defining the limits of resection still depends to a high degree on the surgeon's experience. Various techniques supplementing the clinical diagnosis have been suggested, but none has achieved widespread clinical acceptance [4–12].
The measurement of regional blood flow by fluorescence angiography derives from the 1930s [13]. In brief, the technique relies on the fluorescence of viable, perfused tissue when exposed to ultraviolet or laser light after injection of fluorescein dye. Although it is a well-established technique in ophthalmology, various studies investigated its use in the determination of intraoperative intestinal viability [14]. Due to a consistently subjective interpretation of fluorescent images, results from the literature remain conflicting. Sensitivities of 88–100% were described [15–17], but other study groups reported an accuracy of judgement below 60% and less [18, 19].
Laser-fluorescence videography consists of two-dimensional imaging including variable areas up to 20×40 cm. Besides the observer's qualitative interpretation, staining intensities can be quantified through the use of a computer. The aim of this study was to evaluate the scientific use of computer-assisted laser-fluorescence videography in mesenteric microcirculation in a rabbit model of controlled mesenteric ischaemia and reperfusion. For validation, we used radioactive microspheres representing the gold standard in imaging of vascular patency [11, 18, 20–22].
Materials and methods
Animal model
The study was performed in adherence to the National Institutes of Health guidelines for the use of experimental animals (reference number 50.203.2 AC 18, 1/02 Bezirksregierung Cologne, Germany) and the National Decrees for Radiation Protection. We used the animal model for mesenteric ischaemia in rabbits as described by Ando et al. [19]. Experiments were performed on 12 female rabbits (New Zealand White) weighing 3.7–4.3 kg. Anaesthesia was introduced by subcutaneous injection of a mixture of 0.3 ml/kg medetomidine, 0.2 ml/kg 10% ketamine, and 0.2 ml/kg diazepam. An arterial catheter (Leader Cath 20G, Vygon, Aachen, Germany) was placed in the auricular vein and a 2-ml blood sample was taken for routine laboratory workup. All animals were intubated, but respired spontaneously. Anaesthesia was maintained by intravenous titration of 0.3 ml/kg medetomidine and 0.2 ml/kg 10% ketamine. After typical median laparotomy, a catheter was placed in the descending aorta. Afterwards, four loops of the small intestine (each of 10 cm) were isolated (Fig. 1). In three of them, ischaemia was induced by mesenteric clamping. The fourth segment served as control. For all further investigations (fluorescence angiography, microspheres, histology), all loops were divided into five segments of 2×2 cm (see below). Animals were randomised and divided into two groups. In group I (n=6), ischaemia was maintained for 40 min. In group 2 (n=6), ischaemia was carried out for 60 min followed by reperfusion for 20 min. Blood gas samples were registered after introduction of the arterial catheter, at the beginning of clamping, and at the end of ischaemia–reperfusion (ABL 700, Radiometer, Copenhagen, Denmark). At the end of ischaemia (group I) or reperfusion (group II), microbiologic smears were taken from the surface of all intestinal loops to evaluate bacterial transmigration. The intestinal blood flow was measured firstly by laser-fluorescence angiography, and secondly by microspheres. Finally, all animals were killed by an overdose of pentobarbital and the intestinal loops were excised for further investigations.
Laser-fluorescence videography
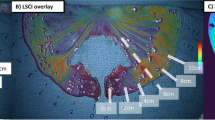
The dynamic laser-fluorescence videography system (IC-VIEW system, Pulsion Medical Systems, Munich, Germany) consists of a digital video camcorder and a laser light (NIR light) and is about the size of a conventional camcorder. After intravenous bolus injection of 2 ml indocyanine green solution (50 mg indocyanine green/100 ml glucose 5%), the situs was illuminated by a laser (energy 0.16 W, wavelength 780 nm). Digital videos were recorded showing the uptake, steady-state distribution, and clearance of the dye-marked blood (Fig. 2a–c). The recorded fluorescence served as a function of tissue perfusion. All videos were viewed in real time and stored in a notebook. For further quantitative evaluation, we used the IC-CALC program (Pulsion Medical Systems). All intestinal loops were equally divided into five regions of interest (ROIs) of 2×2 cm and named A to E clockwise. With the assistance of a computer, the ROIs were painted by hand. The increment of fluorescence (pixel intensity) in the ROIs was measured as steepness of the curve of light emission (pixel intensity per second). The perfusion of the control loop was set as 100% (reference region) (Fig. 3). In total, 120 ROIs were analysed in each group. The results were presented graphically as the percentage of pixel intensity of an ROI compared to the reference region (perfusion index).
Radioactive microspheres
As control, we used the radioactive microsphere technique introduced by Bartrum et al. [20] and established in the measurement of intestinal blood supply in multiple animal models [21, 22]. Directly after recording laser fluorescence, the microspheres were injected intra-arterially into the descending aorta. According to the supplier's instructions, we used 404,000/mg cerium-141 NEN-TRAC microspheres with a diameter of 15 μm (ca. 3.7 MBq, NEM-022A, PerkinElmer, Boston, MA, USA). Through a bur hole, a gamma camera detected the impulse rate per minute of all 2×2-cm samples. Samples from blood and kidneys served as internal controls. After half-time correction, results were recorded as impulse per minute per gram. Finally, the measurements were expressed as the percentage of impulse rate of the ischaemic segments compared to the control loop (reference region).
Light microscopy
After passing the radiation survey, the extent of ischaemic tissue damage was determined by histological examination. A part of each tissue sample was fixed in 10% buffered formalin, embedded in paraffin, and sections (4 μm) were stained with haematoxylin and eosin. For the quantification of ischaemic damage, we used the classification of intestinal mucosal lesions as introduced by Park et al. [23]. In each sample, five sections were evaluated.
Statistics
All data were expressed as mean value and standard deviation if not otherwise stated. In each individual ischaemic segment including the controls, the percentage of impulse rate (microspheres) was compared to the percentage of pixel intensity (fluorescence angiography). Statistical data were analysed by regression analysis. Regression coefficients were calculated for each individual animal as well as for the whole group. To compare laser fluorescence and microspheres in ischaemia and reperfusion, we used Student t test for statistical evaluation. Assessing the histological damage with a semiquantitative score, we analysed differences of the ordinal data by the Mann–Whitney U test for non-parametric parameters. A p value of less than 0.05 was considered significant.
Results
Laser-fluorescence videography
The perfusion videos revealed the typical time-course of upstream, distribution, and clearance of the dye-marked blood (Fig. 2a–c). The mesenteric architecture and the microcapillaries of the bowel wall could easily be identified. Perfused tissue demonstrated a strong fluorescence. Conversely, tissues that were not perfused did not fluoresce. The grossly qualitative (macroscopic) interpretation included information about the speed of upstream fluorescence as well as the homogeneity of fluorescence.
Quantitative evaluation of the segments by means of the IC-CALC program showed a broad range (Fig. 4). Regarding all segments, the perfusion index varied from 0 to 234% (mean 83.09±43.63%). On average, the reperfusion group II (mean 97.94±46.87%, range 0–234%) showed higher values compared to the ischaemia group I (mean 68.24±34.44%, range 11–170%). The differences were significant (p<0.05).
In addition, the results revealed a remarkable rate of intra- and interindividual variability. The animals' circulatory function influenced the microcirculation measured by fluorescence. A generally depressed circulation led to a decreased tide of indocyanine green in all loops, whereas a stable circulation induced a distinct fluorescence (Fig. 4). In addition, we found discrepancies in the blood supply when comparing the loops intra-individually. Single animals simultaneously showed loops with a strong fluorescence as well as pale loops.
Regarding the individual segments A–E (Fig. 5), group I (ischaemia) showed the lowest indices of perfusion in the middle segments (C), representing the greatest distance to the skeletonised margin. Congruently, the perfusion index consequently increased in the marginal segments A and E. Animals of group II (reperfusion) generally demonstrated more stable values. Among the segments A–E, we did not find considerable differences. Generally, the fluorescence was strongly influenced by the blood flow in the neighbouring segments. Thus, regions of the lowest fluorescence were not exclusively located in the centre of the loop but were also found next to low perfused segments elsewhere.
Microspheres
The measurement of the segments' radioactivity repeated the broad range mentioned above (Fig. 4). Evaluating all segments, the impulse rates ranged from 2 to 285% (mean 86.29±50.46%). Again, the reperfusion group II (mean 99.93±59.38%, range 2–285) showed higher average values compared to the ischaemia group I (mean 72.65±34.91%, range 22–240). Again, the differences were significant (p<0.05).
Congruently to the laser fluorescence, we found the same intra- and interindividual variability in impulse rates (Fig. 4). A circulatory insufficiency decreased the impulse rate, whereas a more stable situation during the experiment led to higher radioactivity in all samples of the individual animals. In addition, the microcirculation of the intestinal loops varied in single animals.
Analysis of the impulse rates of the individual segments A–E revealed results similar to that of the fluorescence videography (Fig. 5). Group I (ischaemia) showed the lowest impulse rates in the C segments with the greatest distance to the skeletonised margin. Again, the values increased in both marginal segments (A and E). As the impulse rates measured in group II (reperfusion) were widely stable, we did not find considerable differences when comparing the segments A–E. In parallel to the measured fluorescence, the segments' radioactivity was obviously influenced by the vascular patency of their neighbours.
Validation analysis
Statistical analysis of the results obtained from the laser-fluorescence videography and the microsphere technique demonstrated a close linear correlation. Comparing the intra-individual results animal per animal, the coefficient of correlation (r) ranged from 0.82 to 0.99 (mean 0.92±0.07). Mean r in the ischaemic animals was 0.87±0.05, whereas mean r in the reperfusion animals was 0.96±0.05. Regarding the segments A to E in the individual animals, r varied from 0.88 to 1.0 in ischaemic segments (mean 0.90±0.07) and from 0.82 to 0.88 in reperfusion segments (mean 0.85±0.02). Comparing all segments in group I (ischaemia), r was 0.86 (Fig. 6). Regarding all reperfusion segments (group II), r was 0.86 (Fig. 7). The overall r of all investigated segments was 0.92±0.07.
Histology
In general, the rate of cellular damage in the ischaemic loops was low. Referring to the classification of Park et al. [23], none of the samples reached a grading higher than stadium 2. Figure 8 demonstrates a typical example with an expanded Gruenhagen's space and a moderate lifting of the epithelium from the lamina propria. Corresponding to our results from the laser fluorescence and microspheres, the rate of cellular damage could not be derived from the segments' distance to the margin of dissection. Although the segments with a major loss of blood circulation could be identified by a grossly higher rate of damage, we did not find a reproducible correlation to either the laser-fluorescence videography or the microsphere technique.
Laboratory findings and microbiology
The results from the laboratory workup did not show a considerable correlation to the measurements of laser fluorescence and microspheres. Corresponding to the time of ischaemia, serum lactate grossly tended to higher values at the end of the ischaemic periods. In accordance, the following reperfusion in group II led to a decrease in lactate. However, the differences were not significant in both groups. The blood gas analyses, mainly to analyse the arterial oxygen and carbon dioxide pressure, were not influenced by the time of ischaemia or reperfusion and were undisturbed.
None of the microbiologic smears taken of all ischaemic loops revealed a bacterial translocation.
Discussion
Two-dimensional laser-fluorescence videography, including computer-assisted quantitative evaluation of perfusion indices, can be regarded as a feasible, reliable, and valid technique for the measurement of mesenteric blood flow.
By embolization of the capillary bed, microspheres portray the microcirculation one to one. Correspondingly, the method still represents the gold standard in the experimental measurement of regional blood flow [20, 24, 25]. All results of the laser fluorescence revealed a close linear correlation to the microsphere method. Covering a broad range of vascular patencies, the high correlation could be observed in physiological perfusion as well as in ischaemia or reperfusion of the small intestine. Thus, the computer-assisted interpretation of the fluorescence pattern turned out to be a useful and valid supplement.
In addition, the reliability of the fluorescence videography even reflects the varieties in collateral blood supply of individual loops and segments. Besides circulatory disorders, this represents the high rates of anastomoses and arcades of the intestinal vasa recta. As known in animals as well as in humans, especially the angioarchitecture of the small intestine contains multiple collateral vessels [26–30]. Evaluating this individual microcirculation could be of special importance in cases of extensive resections, which often reduce the remaining length of the gut to a life-threatening degree.
Finally, the practical application of laser-fluorescence videography facilitates its use in a surgeon's daily routine. As the system only contains a portable video camera including a laser luminous source and a laptop, it can be used in any operating room. Furthermore, the intravenous application of indocyanine green is harmless to humans, and repeated measurements are feasible, even though with a delay of approximately 30 min due to washout effects. On the basis of its clinical utility, laser-fluorescence videography is thus superior to the more experimental character of the microsphere method.
Despite valid and reliable quantitative results, the new technique of laser-fluorescence videography also has technical pitfalls and limits that cannot be diminished by the computer-assisted evaluation.
Due to physical characteristics, quantitative measurements of light and energy emission from sloped layers lead to summation effects. Thus, loops in sloped position could present high fluorescence intensities, which falsely represent high rates of microcirculation. Consequently, intestinal loops measured by the laser fluorescence should be displayed in an almost planar position.
In addition, any overlapping should be avoided. However, this concerns not only an uncovered position of the region of interest. As two-dimensional laser-fluorescence videography of the intestine images a three-dimensional tube as a plane layer, the filling of the intestine influences the rate of fluorescent emission. In case of an empty gut, the posterior intestinal wall will at least partly contribute to the total emission, although the penetration depth of the laser light is limited by the first fluorescing layer. In contrast, a full intestine could reduce the fluorescence by covering the posterior wall. Consequently, one should aim for standardised intestinal fillings in the ideal case.
Finally, limiting values in laser-fluorescence videography representing irreversible necrosis are not yet defined. In both groups (ischaemia–reperfusion), the histological examination showed only moderate rates of cellular damage. Grossly, regions with a major loss of blood circulation could be identified by a higher rate of damage. Nevertheless, we did not find a general correlation either to the laser fluorescence or to the microspheres. This widely agrees with our non-correlating results from the laboratory workup. Thus, our experimental setting could not completely reflect the time-course of the human intestine from ischaemia to necrosis. A too short experimental time schedule must be regarded as the main cause [19]. Obviously, the time of ischaemia used in our experimental setting did not suffice to induce a considerable rate of irreversible cellular damage. Similar results in histology are reported in various models from the literature [17, 31–33]. Nevertheless, the steadily increasing rate of mortality during the course of mesenteric ischaemia limits the technical possibilities in experimental settings.
Conclusion
Computer-assisted laser-fluorescence videography is a feasible method for the detection of mesenteric blood supply and intestinal microcirculation. Compared to the gold standard of the microsphere technique, its results are reliable and valid in mesenteric ischaemia as well as in reperfusion. Individual varieties in the angioarchitecture can be reproduced and its simple technique is applicable in a surgeon's daily routine. Clinically, the application of computer-assisted laser-fluorescence videography is conceivable not only in mesenteric ischaemia and infarction but also in the perfusion measurement of gastrointestinal anastomoses or transpositioned intestine. However, technical pitfalls have to be avoided and repetitive measurements need a certain delay. Even more important, limiting values to identify the irreversible necrosis need to be defined in order to outline relevant disorders in circulation from broad anatomical varieties. Further studies have to investigate longer periods of intestinal ischaemia and necrosis to analyse the clinical impact of laser-fluorescence videography on gastrointestinal surgery more precisely.
References
Schneider TA, Longo WE, Ure T et al (1994) Mesenteric ischemia. Acute arterial syndromes. Dis Colon Rectum 37:1163–1174
Eckstein HH (2003) Acute mesenteric ischemia. Resection or reconstruction. Chirurg 74:419–431
Endean ED, Barnes SL, Kwolek CJ et al (2001) Surgical management of thrombotic acute intestinal ischemia. Ann Surg 233:801–808
Billings PJ, Foster ME, Leaper DJ (1986) A clinical and experimental study of colostomy blood flow and healing after closure. Int J Colorectal Dis 1:108–112
Thompson JS, Bragg LE, West WW (1990) Serum enzyme levels during intestinal ischemia. Ann Surg 211:369–373
Kurland B, Brandt LJ, Delaney HM (1992) Diagnostic tests for intestinal ischemia. Surg Clin North Am 72:85–106
Mizock BA, Falk JL (1993) Lactic acidosis in critical illness. Crit Care Med 20:80–93
Sailer M, Debus ES, Fuchs KH (2000) Comparison of anastomotic microcirculation in coloanal J-pouches versus straight and side-to-end coloanal reconstruction: an experimental study in the pigs. Int J Colorectal Dis 15:114–117
Caglayan F, Caglayan O, Gunel E et al (2002) Intestinal ischemia–reperfusion and plasma enzyme levels. Pediatr Surg Int 18:255–257
Pargger H, Staender S, Studer W et al (1997) Occlusive mesenteric ischemia and its effects on jejunal intramucosal pH, mesenteric oxygen consumption, and oxygen tensions from surface of the jejunum in anesthetized pigs. J Intensive Care Med 23:91–99
Brandt LJ, Boley SJ (2000) AGA technical review on intestinal ischemia. American Gastrointestinal Association. Gastroenterology 118:954–968
Sato A, Kuwabara Y, Sugiura M et al (1999) Intestinal energy metabolism during ischemia and reperfusion. J Surg Res 82:261–267
Lange K, Boyd LJ (1934) The technique of the fluorescein test to determine the adequacy of circulation in peripheral vascular diseases, the circulation time, and capillary permeability. Bull N Y Med Coll Flower 5fth Ave Hosp 6:78–81
McGinty JJ, Hogle N, Fowler DR (2002) Laparoscopic evaluation of intestinal ischemia using fluorescein and ultraviolet light in a porcine model. Surg Endosc 17:1140–1143
Gorey T (1980) The recovery of intestine after ischemic injury. Br J Surg 67:699–702
Pearce W, Jones D, Warren G et al (1987) The use of infrared photoplethysmography in identifying early intestinal ischemia. Arch Surg 122:308–310
Bulkley GB, Zuidema GD, Hamilton SR et al (1981) Intraoperative determination of small intestinal viability following ischemic injury. Ann Surg 193:628–637
Ballard LJ, Stone WM, Hallett JW et al (1993) A critical analysis of adjuvant techniques used to assess bowel viability in acute mesenteric ischemia. Am Surg 59:309–311
Ando M, Ito M, Nihei Z et al (2000) Assessment of intestinal viability using a non-contact laser tissue blood flowmeter. Am J Surg 180:176–180
Bartrum RJ, Berkowitz DM, Hollenberg NK (1974) A simple radioactive microsphere method for measuring regional blood flow and cardiac output. Invest Radiol 9:126–132
Appleyard CB, Willimas JL, Hathaway CA et al (1999) Temporal patterns of colonic blood flow and tissue damages in an animal model of colitis. Dig Dis Sci 44:431–438
Sparrow R, Conolly HM (1988) Blood flow to the rat rectum: its intramural distribution and the response to injury. J Anat 159:73–82
Park PO, Haglund U, Bulkley G et al (1990) The sequence of development of intestinal tissue injury after strangulation ischemia and reperfusion. Surgery 107:574–580
Gervais M, Demolis P, Domergue V et al (1999) Systemic and regional hemodynamics assessment in rats with fluorescent microspheres. J Cardiovasc Pharmacol 33:425–432
Juel IS, Solligard E, Lyng O et al (2004) Intestinal injury after thoracic aortic cross-clamping in the pig. J Surg Res 117:283–295
Eisberg HB (1924) Intestinal arteries. Anat Rec 28:227
Lang J, Heichele J (1982) Vessels of the small bowel. Morphol Med 2:207–216
Hansen HH, Stelzner F (1975) Surgical anatomy of the blood supply of the colon. Langenbecks Arch Chir 340:63–74
Premen AJ, Banchs V, Womack WA et al (1987) Importance of collateral circulation in the vascularly occlude feline intestine. Gastroenterology 92:1215–1219
Grandison AS, Yates J, Shields R (1981) Capillary blood flow in the canine colon and other organs at normal and raised portal pressure. Gut 22:223–227
Tollefson DF, Wright DJ, Reddy DJ et al (1995) Intraoperative determination of intestinal viability by pulse oxymetry. Ann Vasc Surg 9:357–360
MacDonald PH, Dinda PK, Bech IT et al (1993) The use of oxymetry in determining intestinal blood flow. Surg Gynecol Obstet 176:451–458
Cooperman M, Pace WG, Martin EW et al (1978) Determination of viability of ischemic intestine by Doppler ultrasound. Surgery 83:705–710
Author information
Authors and Affiliations
Corresponding author
Additional information
C. Toens and C.J. Krones contributed equally to this work.
Rights and permissions
About this article
Cite this article
Toens, C., Krones, C.J., Blum, U. et al. Validation of IC-VIEW fluorescence videography in a rabbit model of mesenteric ischaemia and reperfusion. Int J Colorectal Dis 21, 332–338 (2006). https://doi.org/10.1007/s00384-005-0017-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-005-0017-1