Abstract
Background
Jejunal atresia with short bowel syndrome is an unusual type of jejunoileal atresia. They present with jejunal atresia near the ligament of Treitz and a foreshortened small bowel. In this paper, we report our preliminary experience to emphasize the advantages and feasibility of enteroplasty for intestinal lengthening and primary anastomosis with an anterior flap in jejunal atresia with short bowel syndrome in neonates.
Methods
Between January 2014 and December 2014, four neonates with jejunal atresia and short bowel syndrome were submitted to this procedure in our hospital. Enteroplasty for intestinal lengthening procedures was accomplished in all the neonates by laparoscopic-assisted procedure. The procedure was manually performed after exteriorization of the atretic bowel via the slightly enlarged umbilical port site incision.
Results
The mean operative time was 80 min (range 65–110 min). Blood loss was minimal. There was no mortality or surgical complication so far. The median follow-up duration was 14.5 months (range 9–20 months). In all the cases, the autonomy for oral/enteric feeding was obtained within 1 month after surgery. One neonate was readmitted because of associated cholestasis 1 month after the operation, and was cured by conservative therapy.
Conclusions
Enteroplasty for intestinal lengthening and primary anastomosis with an anterior flap is a safe and feasible technique that could allow increased tolerance to oral/enteric feeding, thereby improves their chances for quality survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infants born with jejunoileal atresia have considerable dilatation of the intestine proximal to the obstruction, and the distal segment of intestine is collapsed. With the large size discrepancy between the proximal and distal segments and the primary dysmotility of the dilated loop, a primary anastomosis often does not function well [1]. Most neonates with jejunal atresia are left with a significant loss of bowel length due to in utero resorption of infracted gut [2]. The neonate with the short bowel syndrome is a major catastrophe and a difficult long-term management problem for the family and the carers.
In 2013, Onofre et al. [3] reported enteroplasty for intestinal lengthening and primary anastomosis with an anterior flap in a neonate with apple-peel intestinal atresia. Using this technique, they simultaneously managed a tailoring procedure that promotes intestinal lengthening and primary anastomosis without a significant loss of the absorptive area. Between January 2014 and December 2014, four cases of jejunal atresia with short bowel syndrome were managed using this technique in our hospital. In this paper, we report our preliminary experience to emphasize the advantages and feasibility of this procedure in neonates.
Materials and methods
Four neonates of jejunal atresia complicated with short bowel syndrome who underwent enteroplasty for intestinal lengthening with an anterior flap between January 2014 and December 2014 were reviewed. The procedures were carried out by a single surgical team. Ethics approval from the Ethics Committee of the Huai’an women and children’s hospital (Jiangsu, China) was obtained. Written informed consents were obtained from the parents preoperatively.
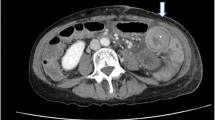
Three male neonates and one female neonate with persistent vomit after birth were referred to our department. Dilated intestinal loops were detected by prenatal ultrasound studies in three of the cases and by postnatal ultrasonographic study in the remaining one patient, with polyhydramnios in two of the patients. Plain abdominal radiographs (Fig. 1) revealed much dilated loops of bowel with no air in the distal intestine, and a subsequent Hypaque enema demonstrated a microcolon with reflux of contrast into the terminal ileum, but not into the proximally dilated bowel. No prenatal interventions were performed. Their age ranged from 1 to 3 days. One neonate had type IIIa jejunal atresia with multiple atresia in the distal segment. Three patients had type IIIb jejunal atresia and one complicated with meconium peritonitis. Microcolon was seen in all the four patients by contrast enema post-partum, colonic atresia could be excluded, and definitive diagnosis of intestinal atresia was made.
The babies were resuscitated with intravenous fluids, nasogastric decompression was done, urethral catheter was placed, and intravenous antibiotics (cefotaxime) and metronidazole were given. The patient was placed supine on the table. The anesthetic machine and the anesthetists were stationed at the head of the patient. Two screens were placed on both sides of the patient. A 5-mm vertical midline umbilical incision was made. A 5-mm 30° laparoscope was inserted through the camera port. Carbon dioxide pneumoperitoneum was established with the pressure at 6–8 mmHg. A 3-mm conventional laparoscopic instrument was inserted through an extra working port, which was placed at the right lower side of the abdomen. The abdominal contents were inspected; the proximal dilated loops and decompressed distal segments were clearly obvious. The two blind ends, or the atretic segments, were guided and pulled towards the umbilical port with the 3 mm forceps. The camera and the umbilical port were removed, the umbilical port incision was enlarged to about 2.5–3 cm longitudinally, and the atretic segments were exteriorized through the umbilical port incision.
Case 1 A girl weighing 3.20 kg was born at 39 weeks gestation. Laparoscopy revealed a type IIIa intestinal atresia. The atretic segments were exteriorized through the slightly enlarged umbilical port incision. The dilated proximal bowel segment from the duodenal junction to the site of atresia measured 30 cm in length and 5 cm in diameter. Multiple jejunal diaphragmatic atresias (three sites) were identified within 30 cm proximal part of the jejunum by intraluminal injection of saline water.
After resection of the distal atretic segment, the distal small bowel segment to the ileocecal valve was measured approximately 20 cm in length. A flap on the antimesenteric border was created from the dilated blind proximal segment of intestine. This flap of the proximal intestinal segment measured 10 cm in length and was turned down to the lower segment and tubularized that leads to the anastomotic opening with a diameter of about 1.5 cm (Fig. 2). An end-to-oblique anastomosis was performed from the tubularized proximal segment to the distal intestinal segment using single-layer running sutures (Fig. 3). Any mesenteric defect is closed. The total intestine was increased from 50 to 60 cm finally.
Case 2 A male neonate weighing 2.60 kg with a gestational age of 37 weeks was admitted with a diagnosis compatible with intestinal obstruction. Laparoscopic-assisted procedure revealed a type IIIb intestinal atresia, with the length of the proximal atretic segment of 30 cm, and the diameter of 4 cm. The remaining distal segment was 25 cm with ileocecal valve. The atretic segments were exteriorized and enteroplasty for intestinal lengthening with an anterior flap was accomplished. The total intestine was increased from 55 to 63 cm finally.
Case 3 A male neonate weighing 2.40 kg was born at 36 weeks gestation. Postnatal X-ray was indicative of an intestinal obstruction. A type IIIb intestinal atresia was confirmed by laparoscopic-assisted surgery. The length of the proximal atretic segment was 35 cm, and the diameter was 4 cm. The remaining distal segment was 30 cm with intact ileocecal valve. The total intestine was increased from 65 to 75 cm by intestinal lengthening with an anterior flap.
Case 4 A male neonate weighing 2.50 kg was born at 38 weeks gestation. At laparoscopic-assisted surgery, a type IIIb jejunal atresia 25 cm from the dudenojejunal flexure with meconium peritonitis and multiple distal type I atresias was found and resected. The remaining distal segment was 35 cm. A primary anastomosis was performed; the length of the total intestine increased from 60 to 68 cm by the intestinal lengthening procedure.
The line diagrams, showing the essence of the procedure, refer to Figs. 4, 5, 6, and 7.
Results
All the four patients were operated using the slightly enlarged umbilical laparoscopic port incision without conversions. The age at the time of operation was 2, 1, 3, 2 days, respectively (Table 1). The mean operative time was 80 min (range 65–110 min). Blood loss was minimal. No blood transfusion was required. There was no mortality or surgical complication so far. No other surgical procedures were required. Feeding was started on post-operative days 7–11, outside the hospital on post-operative days 12–16. The patients remained on parenteral nutrition until full enteral feeding was achieved. In all the cases, the autonomy for oral/enteric feeding was obtained within 1 month after surgery. Patient A was readmitted because of the associated cholestasis 1 month after the operation, and was resolved on conservative therapy. Other patients recovered uneventfully. Up to now, the patients have completed 9–20 months of follow-up visit. The median follow-up duration was 14.5 months, the weight was 12.5, 10.5, 7.6, 7.0 kg, respectively, the length was 84, 81, 70, 66 cm, respectively, and two children received health nutrition guidance. Electrolytes of the patients were normal before discharge. No mortality or morbidity of anastomostic leakage, anastomotic stenosis, intestinal obstruction, wound infection, and wound dehiscence/hernia was encountered. The cosmetic outcomes were superior to that of our conventional open surgery in patients with intestinal atresia.
Discussion
The etiology of jejunoileal atresia is related to intrauterine mesenteric vascular insults, such as volvulus, internal hernia, or constriction secondary to tight gastroschisis [4, 5]. Short bowel syndrome is the most frequent cause of intestinal failure in the pediatric population, where it occurs after the loss of a major segment of the small intestine secondary to congenital or acquired neonatal disorders [6]. Jejunoileal atresia is one of the major causes of neonatal short bowel syndrome, especially in the more complicated type IIIB (apple peel) and type IV (multiple) atresia. Most neonates with jejunal atresia were left with significant loss of bowel length due to in utero resorption of infarcted gut. Many surgical options have been used, but the optimal method of repairing remains unclear. The treatment is based on a multidisciplinary approach involving pediatricians, pediatric surgeons, and nutritionists.
The proximal atretic segment developed significant dilatation from chronic obstruction. With the large size discrepancy between the proximal and distal segments and the primary dysmotility of the dilated loop, a primary anastomosis often did not function well. Several surgical procedures exist to lengthen the residual small intestine of jejunal atresia.
Some authors use as a definition of an SBS if the intestinal length is less than 25 % of the normal length for age. The intestinal length of a term baby could be 250–300 cm. The view of some experts is that if the length of the intestine of a term baby is less than 75 cm, SBS could be defined. In our four cases, the intestinal length was 50–65 cm.
In 2013, Onofre et al. first presented the correction of apple-peel intestinal atresia through enteroplasty using a flap on the antimesenteric border from the dilated blind proximal segment of intestine for intestinal lengthening and primary anastomosis. In his report, the length of the flap was one-third of the length of the dilated proximal intestinal segment, and its base measured half the diameter of the dilated segment.
This procedure is based on the application of the technique initially described by J. Ten Kate to correct long gap esophageal atresia in 1952 [7]. He showed the possibility to lengthen the dilated proximal stump and decrease anastomotic tension.
This enteroplasty technique enabled to increase the length of the short bowel by the length of dilated proximal atretic segment, promoted tailoring to avoid functional obstruction, and enabled anastomosis with adequate calibers to the distal intestinal segment. The total intestine was increased about 10 cm finally; an anterior flap was reversed and tubularized. Reversed bowel peristalsis should prolong the time of food in the intestine; it was on the benefits of the absorption of nutrients. Furthermore, enteroplasty with a flap from the antimesenteric border could be performed on any length of the proximal intestinal segment. In our four cases, the increased intestinal length was about 8–10 cm.
Compared with ileum, jejunum has a relatively wide diameter and a thick intestinal wall, and is rich in blood vessels, especially to the dilated and thickened blind end of jejunal atresia. Furthermore, the base of the intestinal flap is relatively wide, and so the intestinal vascular network flap has good blood circulation. There was no impairment of vascularization of the flap after the procedure in the four cases. However, special care should be paid to the blood supply of the reversed intestinal segment. Had there been an ischemic segment of the flap, part of the flap would have been resected before the tubulization [3].
If the recovery of gastrointestinal function is slow, gastrointestinal series will be carried out a week or so postoperatively to see how the peristalsis functions in these segments. It is beneficial to determine the peristalsis, and the high osmotic pressure of meglumine diatrizoate could promote the recovery of gastrointestinal function.
Minimally invasive surgery is being performed for an expanding list of indications in neonates [8]. Laparoscopy-assisted surgery for neonatal intestinal atresia has been performed in more than 80 cases in our hospital [9]. Onofre et al. first presented the procedure of enteroplasty using a flap with open surgery. We believe that the laparoscopic-assisted procedure confers numerous benefits to the patients, including shorter recovery times and shorter hospitalization, less pain, and less adhesion formation and scarring and worth introduced.
References
Oliveira C, de Silva N, Wales PW (2012) Five-year outcomes after serial transverse enteroplasty in children with short bowel syndrome. J Pediatr Surg 47(5):931–937
Lee SH, Cho YH, Kim HY et al (2012) Clinical experience of complex jejunal atresia. Pediatr Surg Int 28(11):1079–1083
Onofre LS, Maranhão RF, Martins EC et al (2013) Apple-peel intestinal atresia: enteroplasty for intestinal lengthening and primary anastomosis. J Pediatr Surg 48(6):E5–E7
Burjonrappa S, Crete E, Bouchard S (2011) Comparative outcomes in intestinal atresia: a clinical outcome and pathophysiology analysis. Pediatr Surg Int 27(4):437–442
Dalla Vecchia LK, Grosfeld JL, West KW (1998) Intestinal atresia and stenosis: a 25-year experience with 277 cases. Arch Surg 133(5):490–496
Lourenço L, Campos M, Monteiro J et al (2012) Serial transverse enteroplasty (STEP): intermediate outcomes in children with short bowel syndrome. Eur J Pediatr 171(8):1265–1268
Gough MH (1980) Esophageal atresia—use of an anterior flap in the difficult anastomosis. J Pediatr Surg 15(3):310–311
Abhyankar A, Mukhtar Z (2011) Laparoscopy-assisted surgery for neonatal intestinal atresia: single-center experience. Asian J Endosc Surg 4(2):90–93
Li B, Chen WB, Wang SQ et al (2012) Laparoscopy-assisted surgery for neonatal intestinal atresia and stenosis: a report of 35 cases. Pediatr Surg Int 28(12):1225–1228
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Li Bing and other co-authors have no conflict of interest.
Additional information
Authors Li Bing and Ye-bo Wang contributed equally and are co-first authors.
Rights and permissions
About this article
Cite this article
Li, B., Xia, Sl., Chen, Wb. et al. Laparoscope-assisted intestinal lengthening using an anterior flap in jejunal atresia. Pediatr Surg Int 31, 1183–1187 (2015). https://doi.org/10.1007/s00383-015-3803-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-015-3803-z