Abstract
Objective
To investigate the effects of probiotics on bacterial translocation in the obstructive common bile duct with comparison to an enteral product containing arginine and glutamine.
Material and method
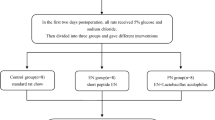
In our study, 40 Sprague–Dawley rats each weighing 250–300 g were used. Animals in Group 1 (sham) were laparatomized and fed standard chow supplemented with physiologic saline at daily doses of 2 ml through orogastric tube for 7 days. Common bile ducts of the animals in the other groups were ligated with 3/0 silk sutures. Group 2 (control group) was fed standard chow supplemented with daily doses of 2 ml physiologic saline. Group 3 (probiotic group) was fed standard chow supplemented with a probiotic solution (Acidophilus plus) containing strains of Lactobacillus acidophilus, Bifidobacterium bifidum and Lactobacillus bulgaricus at a daily doses of 2 × 109 colony forming units (CFU). Group 4 (formula group) was fed only an enteral solution (Stresson Multi Fiber) containing glutamine, arginine and a medium-chain fatty acid at daily doses of 2 g/kg. At the end of the 7th day, all animals were relaparatomized, and to determine bacterial translocation, aerobic, and anaerobic cultures were obtained from the specimens of mesenteric lymph nodes, intestinal mucosa, and blood samples. Smear cultures prepared from caecum were examined to determine the number of CFU. Finally, for histological examination specimens were excised from terminal ileum, and oxidative damage was assessed in liver tissues. Afterwards all animals were killed.
Results
Moderately lesser degrees of bacterial translocation, and mucosal damage were seen in Groups 3, and 4 relative to Group 2 (p < 0.05). In Group 4, any difference was not seen in the number of cecal bacteria relative to baseline values, while in Group 3, significant decrease in cecal colonization was seen. Among all groups, a significant difference between levels of malondialdehyde, and glutathione was not observed.
Conclusion
At the end of our study, we have concluded that both probiotics, and enteral diets which contain immunomodulators such as glutamine, and arginine alleviate bacterial translocation, and impairment of intestinal mucosa.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bacterial translocation is the passage of bacteria through mucosal barrier, and then from gastrointestinal system into mesenteric lymph nodes, liver, spleen, etc. This passage does not occur under normal conditions. Disruption of integrity, and barrier function of intestinal mucosa, in cases of burn injuries, starvation, trauma, surgery, intestinal, and biliary tract occlusion, increases absorption and extrusion of bacteria with their resultant translocation into other organs [1–7].
Obstruction of the biliary flow into the duodenum, and accumulation of bile salts in the liver cells, and biliary tract is known as cholestasis. As a result of cholestasis, some pathological changes occur in the organism. Some of the predominant ones include reticuloendothelial system dysfunction, suppression of the immune system, structural, and functional changes in the intestinal mucosa, oxidative damage of the intestinal wall, blockade of the antibacterial, and detergent effects of bile salts secondary to their impaired enterohepatic circulation, bacteremia, and endotoxemia [1, 8–11].
Clinical and experimental studies have been, and will be conducted to disclose, and prevent the emergence of the mechanisms involving in bacterial translocation. Probiotics are non-pathogenic microorganisms which maintain, and promote microbial balance with ensuing enrichment of the flora. It has been reported that via their host protective impact on antimicrobial activity, resistance to bacterial colonization, stimulation of the immune system, and enzymatic activity, probiotic bacteria exert favorable effects on mucosal lining of oral cavity, gastrointestinal, upper respiratory tract, and urogenital system, and eventually flourish well-being, and decrease the risk of contracting a disease. Especially their effects on intestinal mucosa and immunity indicate the protective role of probiotics in conditions which might induce bacterial translocation [12–17].
Use of enteral products (also termed as immunomodulators) containing glutamine, arginine, nucleotides, and short-chain fatty acids which protect, and support immune functions of the intestine, decreases the rate of bacterial translocation [2, 18–22].
In the present study, we aimed to investigate the effects of probiotics on bacterial translocation, alterations in intestinal mucosa, and formation of free radicals induced by choledocal obstruction in comparison with those of an enteral product containing glutamine, and arginine.
Materials and methods
Our experimental study was performed in Istanbul University, Institute of Experimental Medicine, Research, and Application Center (DETAE). In this study, 40 Sprague–Dawley rats each weighing 250–300 g were used. All of the experimental animals were kept in metal cages without restricting their movements, and fed with water, and standard pellets under constant ambient conditions.
Under ketamine (100 mg/kg) plus xylazine (15 mg/kg) anesthesia, incision site was disinfected with povidone–iodine, and through a midline incision, the abdominal cavity was entered.
Group 1 (Sham group): After exposure of the common bile duct during laparotomy, the rats fed standard chow and received physiologic saline through an orogastric tube for 7 days at daily doses of 2 ml.
Common bile ducts of the animals in the other groups were ligated with 3/0 silk sutures.
Group 2 (control group) was fed standard chow supplemented with physiologic saline through an orogastric tube for 7 days at daily doses of 2 ml.
Group 3 (probiotic group) was fed standard chow supplemented with a probiotic mixture (Acidophilus plus, Pharmadass, Harrow, UK) containing strains of Lactobacillus acidophilus (2 × 109 CFU/capsule), Bifidobacterium bifidum (1 × 109 CFU/capsule) and Lactobacillus bulgaricus (1 × 109 CFU/capsule) at a daily doses of 2 × 109 CFU via an orogastric tube [23–25].
Group 4 (formula group) was fed with only an enteral solution (Stresson Multi Fiber, Nutricia, Istanbul, Turkey) containing 1,344 mg glutamine, 889 mg arginine, 1.5 g medium-chain fatty acid in each 100 ml of the diet solution at daily doses of 2 g/kg.
At the end of the 7th day, all rats were relaparatomized under ketamine plus xylazine anesthesia. In all animals, aerobic, and anaerobic cultures were performed in specimens of mesenteric lymph nodes (MLNs), and intestinal (terminal ileal) mucosa, and blood samples to determine bacterial translocation (BT). Smear cultures prepared from caecum were examined to determine the number of CFU. Finally, for histological examination specimens were excised from terminal ileum, and also oxidative damage was assessed to measure malondialdehyde (MDA) and glutathione (GSH) levels in liver tissue samples. Afterwards all animals were killed.
Microbiological analysis
Cecal samples were inoculated on Carry-Blair transport culture media, while specimens of mesentery, and ileum were placed in sterile Petri dishes. Blood samples were inoculated on the blood culture media. Samples other than blood were inoculated on agar culture media mixed with sheep blood for aerobic, and on Schaedler media for anaerobic bacteria. As a liquid culture media, a Schaedler bouillon made oxygen-free by boiling for 10 min was used. Burri–Wright method was employed to provide anaerobic conditions in this liquid media. All culture media were incubated at 35–37 °C for at least 24–48 h. For anaerobic cultures, inoculated culture media were placed in GASPAK jars to provide anaerobic conditions. Petri dishes were examined 24 h later for the growth of aerobic microorganisms. Colonies in Petri dishes with bacterial growth were firstly stained with Gram dyes, and then bacterial identification was performed using routine classical methods. Presence of catalase-negative Gram-positive cocci, and DNAases, effect of Gram-negative cocci on various carbohydrates, and various enzymes were investigated. Forty-eight hours after incubation anaerobic growth on Petri dishes, and liquid medium were evaluated. From turbid liquid culture media priorly inoculations onto aerobic (blood agar), and anaerobic (Schaedler agar) media were performed, and then Petri dishes were incubated under suitable conditions.
For the identification of the species of anaerobic bacteria, in consideration of their Gram staining characteristics, antibiotic discs were used; then, they were inoculated on bile agar. Blood samples were inoculated on media used for hemoculture. From bottles demonstrating bacterial growth, inoculations were made on aerobic and anaerobic media for the identification of isolates.
Biochemical analysis
Determination of lipid peroxide and glutathione (GSH) levels in liver tissue
The livers of the animals were rapidly removed, washed in 0.9 % NaCl solution, and kept in ice. Liver tissue was homogenized in ice-cold 0.15 M KCl (10 %; w/v) solution. To assess lipid peroxidation, MDA levels were determined using thiobarbituric acid according to the method of Ohkawa et al. [26]. The breakdown (degradation) product of 1,1,3,3-tetraethoxypropane was used as a standard, and the results were expressed as nmol MDA/g tissue. GSH levels were measured in the homogenates by the method of Beutler et al. [27]. The method is based upon the development of a relatively stable yellow color when 5,5′-dithiobis-(2-nitrobenzoic acid) (DTNB) is added to sulfhydryl compounds. After precipitation with metaphosphoric acid, supernatants were reacted with DTNB. Absorbance was read spectrophotometrically at 412 nm [27, 28].
Histopathological analysis
Small bowel specimens were fixed in buffered 10 % formaldehyde. After routine tissue treatments, 5–7 micron sections cut from the prepared paraffin blocks were stained with hematoxylin–eosin (HE), and periodic acid schiff (PAS) dyes, examined, and evaluated under light microscope. Pathological changes in the terminal ileum were interpreted according to Chiu classification [29]: Stage 0: normal mucosa (Fig. 1); Stage 1: subepithelial space, and capillary congestion (Fig. 2); Stage 2: subepithelial space was enlarged leading to moderate detachment of epithelial layer from lamina propria (Fig. 3); Stage 3: extensive detachment of epithelial layer from lamina propria (Fig. 4); Stage 4: loss of villi, capillary dilatation, hypercellularity in lamina propria (Fig. 5); Stage 5: areas of ulceration, bleeding, and destruction on lamina propria.
Statistical evaluation
For the assessment of bacterial translocation Fisher’s Chi-square, Mann–Whitney U tests, and for the estimation of histological scores Mann–Whitney U test were used. For the evaluation of biochemical test results, one-way ANOVA test, and for multiple comparisons Tukey HSD test were preferred.
Results
Ten rats in each group amounting to a total of 40 animals were used in the study. During the study period none of the animals died.
Rates of bacterial translocation into blood, and MLNs categorized in groups are shown in Table 1. Rates of BT in Groups 3 and 4 were significantly lower relative to Group 2 (p < 0.05).
Mean number of colonies in the cecal specimens are shown in Table 2. Mostly E. coli was exposed to translocation. Significantly lesser number of cecal intraluminal bacteria was found in Group 3. Comparison of the number of colonies in the cecum differed significantly between the probiotic, control and formula groups (p < 0.05).
Distribution of histopathologic stages among groups is shown in Table 3. Any statistically significant difference between Groups 3, and 4 was not (p = 0.34) observed, while when results in both groups were compared with those of the Group 2 (control group), mucosal damage was seen less frequently in the Group 3 and 4 (p < 0.05) (Fig. 6).
When measurements of GSH, and MDA to determine oxidative damage in the liver tissue were compared, a statistically significant difference was not observed between groups (Table 4).
Discussion
Burn injury, starvation, surgical trauma, intestinal obstruction, shock, antibiotherapy result in intestinal mucosal damage, suppression of the immune system, altered balance among intestinal flora, and translocation of bacteria into tissues outside the gastrointestinal system [3, 4, 7, 30–35].
The mechanism of the bacterial translocation is not fully known. Disequilibrium between intestinal microflora, and host defense mechanisms (mucosal barrier, immunological defense, gastric acidity, and gastrointestinal motility) is thought to have a major role in bacterial translocation [36].
Cholestasis which occurs as a consequence of common bile duct obstruction leads to suppression of immune system, reticuloendothelial system dysfunction, oxidative damage of the intestinal wall, structural, and functional impairment of the guts resulting in bacterial translocation out of bowels [8, 9, 11].
Increased frequencies of bacterial translocation in obstructive jaundice have been clearly demonstrated in animal studies. Attenuation of immune functions and inflammatory response is the main etiological factor in the development of infectious complications in cases with obstructive jaundice [36].
In a study performed by Parks et al. [11], development of morphological alterations in mucosal layers of the terminal ileum, and increased rate of bacterial translocation were demonstrated in the bacterial cultures of blood samples, and specimens of MLN, liver, and spleen harvested 1 week after induction of obstructive cholestasis when compared with the control group.
In our study, we have also observed increased bacterial growth in blood, and MLN cultures of the animals with ligated common bile ducts relative to only laparatomized group. Rates of bacterial translocation into blood and MLN were found to be 100 and 70 %, respectively.
In animal models of experimentally induced cirrhosis, antibiotherapy administered to prevent bacterial infections, and to suppress aerobic intestinal flora was found to be effective. However, especially in patients under long-term prophylaxis, gradually increasing resistance against antibiotics was observed. For this reason, probiotics which contain live microorganisms have been introduced into clinical practice. These probiotics are included in the category of functional nutrients, and defined as physiologically active ingredients which apart from their main nutritional characteristics, they stabilize the balance between intestinal flora, and exert beneficial effects on the health state [25].
Probiotics are microorganisms which flourish the characteristics of the endogenous microflora so as to demonstrate favorable effects on the health state of the host. It has been reported that probiotics exert indirect and direct effects on intestinal physiology, stimulate immune system, influence gastrointestinal system, upper respiratory tract, and urogenital system mucosa, improve health state, and have a potential to decrease risk of contracting disease. Probiotic bacteria demonstrate antagonistic and resistive effects against bacterial colonization, and also have immunologic, antimutagenic, and antigenotoxic effects which all influence intestinal microflora favorably [13, 14, 36].
Chiva et al. [25] investigated the effects of Lactobacillus johnsonii La1 strains and antioxidants on patients with experimentally induced cirrhosis, and demonstrated decreased rates of bacterial translocation and endotoxemia in the group of animals fed with probiotics alone or in combination with an antioxidant.
Bauer et al. [24] disclosed relatively lower bacterial translocation rates in the group of rats with CCL4-induced cirrhosis fed with a strain of Lactobacillus.
We also observed extremely decreased bacterial translocation in blood samples, and mesenteric lymph node specimens, and markedly lower number of bacterial colonies in the caecum of the rats fed with a probiotic solution (Acidophilus Plus) containing strains of L. acidophilus, B. bifidum and L. bulgaricus. Besides, histopathologic examination revealed reduced levels of mucosal damage when compared with the control group.
Intestines require glutamine, arginine, nucleotides, and medium-chain fatty acids for the maintenance of their normal immune functions. Therefore, many enteral solutions are prepared so as to contain these ingredients. Use of these immunomodulator diets decrease rates of bacterial translocation [29, 37]. Glutamine is a more important source of energy for enterocytes, and colonocytes than glucose. In animal experiments, glutamine has been shown to enhance intestinal mucosal functions, repair, and development. Conditions like sepsis, trauma, surgery, and shock induce decreases in blood glutamine levels. Clinical studies have demonstrated ameliorating effects of glutamine supplementation on clinical outcomes in catabolic patients [18, 20, 38–40].
Erbil et al. investigated the effects of deoxycholate, lactulose, and glutamine on induced bacterial translocation in cases with obstructive common bile duct. All of three products demonstratedly decreased bacterial translocation, being most prominent in the glutamine group. The authors also revealed decreased malondialdehyde, and myeloperoxidase activity in the glutamine group [41].
In a study performed by Schimple et al. [42], rats with experimentally induced obstructive jaundice, and chronic portal hypertension were fed with glutamine, allopurinol, glutamine + allopurinol, and decreased rates of bacterial translocation, and malondialdehyde, and myeloperoxidase activity were demonstrated in the allopurinol and glutamine groups.
We also observed significantly lower bacterial translocation rates in blood, and MLN samples, and also decreased intestinal mucosal damage in Group 4 fed with Stresson Multi Fiber diet which contains glutamine, arginine, and medium-chain fatty acids. Cecal bacterial growth was not different from that of the control group. However, favorable changes were not seen in the levels of MDA, and GSH.
In comparisons between the probiotic, and the formula groups, a statistically significant difference was not observed as for their ameliorating effects on rates of bacterial translocation, and intestinal mucosal injury. Though probiotics significantly decreased the number of bacterial colonies in the cecum, any relevant effects of enteral products containing glutamine, and arginine were not seen. In our study, in all groups, any significant difference was not observed between hepatic levels of MDA, and GSH which are indicators of oxidative damage.
At the end of our study, we have concluded that both probiotics, and immuno-modulating diets prevent bacterial translocation, and intestinal damage occurring following obstructive cholestasis, and they can be used in the treatment of conditions which might induce bacterial translocation.
References
Albillos A, Hera A (2002) Multifactorial gut barrier failure in cirrhosis and bacterial translocation: working out the role of probiotics and antioxidants. J Hepatol 37:523–526
Alexander JW, Boyce ST, Babcock GF, Gianotti L, Peck MD, Dunn DL, Pyles T, Childress CP, Ash SK (1990) The process of microbial translocation. Ann Surg 212(4):496–510
Barber AE, Jones WG 2nd, Minei JP, Fahey TJ 3rd, Lowry SF, Shires GT (1991) Bacterial overgrowth and intestinal atrophy in the etiology of gut barrier failure in the rat. Am J Surg 161(2):300–304
Başaran UN, Celayir S, Eray N, Oztürk R, Senyüz OF (1998) The effect of an H2-receptor antagonist on small bowel colonization and bacterial translocation in newborn rats. Pediatr Surg Int 13:118–120
Duffy LC (2000) Interactions mediating bacterial translocation in the immature intestine. J Nutr 130:432–436
Saadia R, Schein M, MacFarlane C, Boffard KD (1990) Gut barrier function and the surgeon. Br J Surg 77(5):487–492
Ziegler TR, Smith RJ, O’Dwyer ST, Demling RH, Wilmore DW (1988) Increased intestinal permeability associated with infection in burn patients. Arch Surg 123:1313–1319
Ding JW, Anderson R, Stenham U, Lunderquist A, Bengmark S (1992) Effect of biliary decompression on reticuloendothelial function in jaundiced rats. Br J Surg 79:648–652
Kimmings AN, van Deventer SJH, Obertop H, Rauws EA, Gouma DJ (1995) Inflammatory and immunologic effects of obstructive jaundice: pathogenesis and treatment. J Am Coll Surg 181:567–581
Lorenzo-Zùniga V, Bartolí R, Planas R, Hofmann SF, Vinado B, Hagey LR, Hernández JM, Mané J, Alvarez MA, Ausina V, Gassull MA (2003) Oral bile acids reduce bacterial overgrowth, bacterial translocation and endotoxemia in cirrhotic rats. Hepatology 37:551–557
Parks RW, Stuart Cameron CH, Gannon CD, Pope C, Diamond T, Rowlands BJ (2000) Changes in gastrointestinal morphology associated with obstructive jaundice. J Pathol 192:526–532
Ishibashi N, Yamazaki S (2001) Probiotics and safety. Am J Clin Nutr 73:465–470
Isolauri E (2001) Probiotics in human disease. Am J Clin Nutr 73:1142–1146
Kopp-Hoolihan L (2001) Prophylactic and therapeutic uses of probiotics: a review. J Am Diet Assoc 101(2):229–238
Molin G (2001) Probiotics in foods not containing milk or milk constituents, with special reference to Lactobacillus plantarum 299v. Am J Clin Nutr 73:380–385
Reid G (2002) Safety of Lactobacillus strains as probiotic agents. Clin Infect Dis 35:349–350
Rolfe RD (2000) The role of probiotic cultures in the control of gastrointestinal health. J Nutr 130:396–402
Buchman LA (1996) Glutamine: is it a conditionally required nutrient for the human gastrointestinal system? J Am Coll Nutr 15(3):199–205
Kennedy JA, Parks RW, Clements WDB, Rowlands BJ (1995) Failure of macrophage activation in experimental obstructive jaundice: association with bacterial translocation. Br J Surg 82:1433–1434
McAnena OJ, Moore FA, Jones TN, Parsons P (1991) Selective uptake of glutamine in the gastrointestinal tract: confirmation in a human study. Br J Surg 78:480–482
Salvalaggio PRO, Campos ACL (2002) Bacterial translocation and glutamine. Nutrition 18:435–436
Tenenhaus M, Hansbrough JF, Zapata-Sirvent RL, Ohara M, Nyhan W (1994) Supplementation of an elemental enteral diet with alanyl-glutamine decreases bacterial translocation in burned mice. Burns 20(3):220–225
Adawi D, Ahrné S, Molin G (2001) Effects of different probiotic strains of Lactobacillus and Bifidobacterium on bacterial translocation and liver injury in an acute liver injury model. Int J Food Microbiol 70(3):213–220
Bauer TM, Fernández J, Navasa M, Vila J, Rodés J (2002) Failure of Lactobacillus spp. to prevent bacterial translocation in a rat model of experimental cirrhosis. J Hepatol 36(4):501–506
Chiva M, Soriano G, Rochat I, Peralta C, Rochat F, Llovet T, Mirelis B, Schiffrin EJ, Guarner C, Balanzó J (2002) Effect of Lactobacillus johnsonii La1 and antioxidants on intestinal flora and bacterial translocation in rats with experimental cirrhosis. J Hepatol 37:456–462
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxidase in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358
Beutler E, Duran O, Kelly BM (1963) Improved method for the determination of blood glutathione. J Lab Clin Med 61(5):882–888
Deleve LD, Kaplowitz N (1991) Glutathione metabolism and it is role in hepatotoxicity. Pharmacol Ther 52:287–305
Chiu CJ, McArdle AH, Brown R, Scott HJ, Gurd FN (1970) Intestinal mucosal lesion in low flow states. Arch Surg 101:478–483
Akın ML, Erenoglu C, Dal A, ErdemElbuken E, Batkin A (2001) Hyperbaric oxygen prevents bacterial translocation in rats with obstructive jaundice. Dig Dis Sci 46(8):1657–1662
Jones WG 2nd, Minei JP, Barber AE, Rayburn JL, Fahey TJ 3rd, Shires GT 3rd, Shires GT (1990) Bacterial translocation and intestinal atrophy after thermal injury and burn wound sepsis. Ann Surg 211:399–405
Parks RW, Clements WDB, Pope C, Halliday MI, Rowlands BJ, Diamond T (1996) Bacterial translocation and gut microflora in obstructive jaundice. J Anat 189:561–565
Salman FT, Buyruk N, Gürler N, Çelik A (1992) The effect of surgical trauma on the bacterial translocation from the gut. J Pediatr Surg 27:802–804
Spaeth G, Berg RD, Specian RD, Deitch EA (1990) Food without fiber promotes bacterial translocation from the gut. Surgery 108:240–246
Tadros T, Traber DL, Heggers JP, Herndon DN (2003) Effects of interleukin-1 alfa administration on intestinal ischemia and reperfusion injury, mucosal permeability and bacterial translocation in burn and sepsis. Ann Surg 237(1):101–109
Nieuwenhuijs VB, Dijk JE, Gooszen HG, Akkermans LM (2000) Obstructive jaundice, bacterial translocation and interdigestive small bowel motility in rats. Digestion 62:255–261
Braga M, Gianotti L, Cestari A, Vignali A, Pellagatta F, Dolci A, Di Carlo V (1996) Gut function and immune and inflammatory responses in patients perioperatively fed with supplemented enteral formulas. Arch Surg 131:1257–1265
Chen K, Nezu R, Sando K, Haque SM, Iiboshi Y, Masunari A, Yoshida H, Kamata S, Takagi Y, Okada A (1996) Influence of glutamine supplemented parenteral nutrition on intestinal aminoacid metabolism in rats after small bowel resection. Jpn J Surg 26:618–623
Farges MC, Berard MP, Raul F, Cézard JP, Joly B, Davot P, Vasson MP, Cynober L (1999) Oral administration of glutamine enriched diet before or after endotoxin challenge in aged rats has limited effects. J Nutr 129(10):1799–1806
MacFie J, McNaught C (2003) Glutamine and gut barrier function. Nutrition 18(5):433–434
Erbil Y, Berber E, Ozarmağan S, Sever R, Eminoglu L, Calis A, Olgaç V, Gürler N (1999) The effects of sodium deoxycholate, lactulose and glutamine on bacterial translocation in common bile duct ligated rats. Hepatogastroenterology 46:2791–2795
Schimple G, Pesendorfer P, Steinwender G, Feierl G, Ratschek M, Höllwarth ME (1996) Allopurinol and glutamine attenuate bacterial translocation in chronic portal hypertensive and common bile duct ligated growing rats. Gut 39:48–53
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sarac, F., Salman, T., Gun, F. et al. Effect of probiotic supplementation on bacterial translocation in common bile duct obstruction. Pediatr Surg Int 31, 155–161 (2015). https://doi.org/10.1007/s00383-014-3643-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-014-3643-2