Abstract
Aim
To review our practice of Meckel’s Tc-99m pertechnetate scans over 18 years with regard to indications for the test, sensitivity and specificity in our particular referral patients’ population.
Materials and methods
This is a retrospective review of Meckel’s scans performed in two paediatric tertiary care teaching hospitals from April 1993 to March 2011 and followed up till October 2011. The scan was performed according to published international guidelines. 183 patients were included in this study. We classified the patients into two groups: group 1, which included 77 patients (42 %) presenting with painless per rectum bleeding, and group 2, which included 106 patients (58 %) presenting with other non-specific symptoms (e.g. abdominal pain, possibly associated with nausea and/or vomiting, failure to thrive). Data were analysed using Chi square test, considering P value less than 0.05 as significant. The age of the patients ranged from 4 days to 16.5 years (median 3 years).
Results
161 of the total 183 children on the study (88 %) had a negative Meckel’s scan, and 22 children (12 %) had a positive scan. In the group with a positive Meckel’s scan (22 children), all patients underwent surgical exploration and ectopic gastric mucosa was found in 17 cases (77 %, true positives). In the remaining 5 cases (23 %), there was no evidence of ectopic gastric mucosa (false positives). Within the group with a negative scan, 8 children (5 %) underwent surgery; only 1 child had a ectopic gastric mucosa detected following surgery (false negative). In other 52 children (32 %) of the group with a negative Meckel’s scan, an endoscopy was done, which showed a normal result in 21 children and was abnormal in 31 children. Of the remaining 101 (63 %) children with a negative Meckel’s scan, 74 children (46 %) improved without any further intervention. In 13 cases (8 %), other pathologies were identified. The sensitivity and specificity of the Meckel’s scan for ectopic gastric mucosa were 94 and 97 %, respectively. The Meckel’s scan was positive in 26 % of the patients of group 1 and in only 2 % patients of group 2. The difference between the two groups was highly significant [P < 0.0001 (Yates-corrected Chi square); odds ratio 18 (Woolf-logit method 95 % CI)].
Conclusion
The Meckel’s scan retains a high diagnostic accuracy in children for detecting a Meckel’s diverticulum with ectopic gastric mucosa within it, when performed according to the recommended guidelines. The test yields its highest positive result in children presenting with significant per rectum bleeding.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Meckel’s diverticulum (MD) is the most common congenital anomaly of the gastrointestinal tract in children, with an incidence of about 2 % [1–3] in the general population. In the majority of patients, the MD is asymptomatic. Ectopic gastric mucosa is present in about 20 % of MD [4, 5]. The lifetime risk of developing complications from a MD is about 4 % [6]. In 1933, Charles Mayo wrote: “The Meckel’s diverticulum is frequently suspected, often looked for, and seldom found” [7]. Eighty years on, the preoperative diagnosis of MD is still challenging.
The Tc-99m-pertechnetate Meckel’s scan has long been an important test in the diagnostic work up of patients with suspected MD. It is a non-invasive test with a low radiation burden and it is easy to do. Some specialized expertise is however necessary to acquire and interpret the images, and appropriate guidelines to help perform a high quality scan have been published [8]. In recent years, some reports have questioned the value of Tc-99m pertechnetate in detecting ectopic gastric mucosa [3]. Therefore, we decided to undertake this retrospective study to review the indications and the diagnostic accuracy of the Meckel’s scan in our patients’ population.
Materials and methods
This is a retrospective study of the Tc-99m pertechnetate Meckel’s scans performed in two paediatric tertiary care teaching hospitals between April 1993 and March 2011. The cases were followed up till October 2011. In preparation for the scan, every child received pre-medication with cimetidine or ranitidine for 2 days before the scan and the morning of the scan. An activity of Tc-99m pertechnetate scaled from 150 MBq according to body weight was injected intravenously. A dynamic acquisition (one frame per minute over 60 min) of the abdomen and pelvis was obtained immediately after tracer injection with the child supine on the gamma camera couch. Static images of the abdomen and pelvis after bladder emptying were subsequently acquired. Further delayed imaging after change of position, and possibly SPECT, was occasionally performed. All the Meckel’s scans were reported by two experienced nuclear medicine consultants. The scan results were classified into five categories. The scans considered negative for ectopic gastric mucosa were classified as 1–3 (1 = negative for ectopic gastric mucosa, 2 = probably negative for ectopic gastric mucosa, 3 = equivocal for ectopic gastric mucosa). The scans considered positive for ectopic gastric mucosa were classified as 4 and 5 (4 = probably positive for ectopic gastric mucosa, 5 = definitely positive for ectopic gastric mucosa). Clinically, the patients were classified into two groups: group 1 included patients whose main complaint was painless per rectum (PR) bleeding; group 2 included patients who presented with other non-specific symptoms (e.g. abdominal pain, possibly associated with nausea and/or vomiting, failure to thrive, etc.). The results of the Meckel’s scans in these two groups were compared using the Yates-corrected Chi square test and the Woolf-logit method. A P value of less than 0.05 was considered as significant.
Results
Out of the total number of 192 Meckel’s scans performed during the study period of 18 years, 9 cases were excluded (as the Meckel’s scan reports were not found in 4 cases, the scan acquisition was unsatisfactory in 3 cases, and no surgical follow-up was available in 2 cases). Hence, a total of 183 Meckel’s scans in 183 different patients were included in this study. The median age was 3 years (4 days–16.5 years) and the median follow up period (post-scan) was 2 years (0.2-10 years). Presenting symptoms were painless PR bleeding (group 1) in 77 out of 183 patients (42 %), and other non-specific symptoms (group 2) in 106/183 patients (58 %). The Meckel’s scan was positive for ectopic gastric mucosa in 22 patients (12 %) and negative in 161 patients (88 %).
In the group of patients with a positive Meckel’s scan (n = 22) (Table 1), all patients underwent surgical exploration and ectopic gastric mucosa was found in 17 patients (77 %; true positive cases). Examples of positive Meckel’s scans are shown in Figs. 1 and 2. In 5 patients (23 %), there was no evidence of ectopic gastric mucosa at surgery and in them the Meckel’s scan was considered falsely positive. In these patients, the surgical exploration demonstrated tubular duplication in one case, intussusception in another case, nothing of note in two cases, a Meckel’s diverticulum with only small bowel mucosa but no evidence of ectopic gastric mucosa in one case.
An 18-month-old boy presenting with PR bleeding (2 episodes 8 months apart). A Meckel’s scan is displayed, with sequential imaging of the abdomen and pelvis in anterior projection during 1 h. The scan shows a focal area of abnormally increased tracer uptake in the right lumbar region. Laparoscopic surgery identified a MD, which was resected. Histopathology confirmed ectopic gastric mucosa with acid secreting parietal cells
10-month-old boy, who presented with PR bleeding. The initial dynamic acquisition over 1 h. a Focal area of abnormally increased tracer uptake in the upper abdomen just to the right of the midline, clearly seen in some frames but lost on others. Delayed images at 5 h after micturition. b Clearly confirm the abnormal uptake, in keeping with a MD positive scan. This child underwent surgery and histopathology confirmed ectopic gastric mucosa within a MD
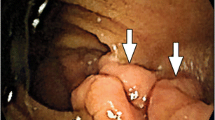
In the group of patients with a negative Meckel’s scan (n = 161) (Table 2), 160 cases were true negatives and 1 case was false negative. An example of a true negative scan is shown in Fig. 3. Eight patients (5 %) underwent surgery anyway. The operative findings in them demonstrated a negative exploration in three cases, mesenteric adenitis in one case, angiodysplasia requiring right hemicolectomy in one case, intussusception in one case, a polyp at the splenic flexure in one case and a MD with ectopic gastric mucosa in one case (this was a false negative Meckel’s scan). In 52 out of these 161 patients (32 %) with a negative Meckel’s scan, endoscopies were performed, which showed normal findings in 21 patients and abnormal findings in 31 patients (details described in Table 2), 13 patients (8 %) were diagnosed with other pathology (details in Table 2). In 74 patients (46 %) symptoms improved and no further intervention was required. In 14 patients (9 %) with a negative Meckel’s scan, the final outcome was not available, as they were finally lost to follow-up.
In summary, we had 17 true positive Meckel’s scans, 5 false positives, 160 true negatives and 1 false negative. The sensitivity and the specificity of the Meckel’s scan for ectopic gastric mucosa in our series were 94 and 97 %, respectively (Table 3). Interestingly, the Meckel’s scan was positive in 26 % (20/77) of the patients presenting with PR bleeding (group 1) and in only 2 % (2/106) of the patients presenting with other non-specific symptoms (group 2). The difference between these two groups was significant [P < 0.0001 (Yates-corrected Chi square); Odds ratio 18.24 (Woolf-logit method 95 % CI)].
Discussion
The Meckel’s isotope scan using Tc-99m pertechnetate has been a well-established technique to diagnose MD for over three decades [9]. The uptake of Tc-99m-pertechnetate by ectopic gastric mucosa depends on the presence of an active Na Iodide symporter system in the parietal as well as the adjacent mucosal cells [10]. The reported sensitivity of the Meckel’s scan varies from 60 to 90 % [2, 9, 11–14]. Similarly, the specificity varies from 90 to 98 % [2, 11, 13, 14]. The sensitivity (94 %) and specificity (97 %) of the Meckel’s scan in our series compare with the best published reports in literature. Our series of patients reflects the referral pattern of two major paediatric tertiary referral centres. The prevalence of a MD with ectopic gastric mucosa is probably low in our series and this is clearly a limitation of our study in testing the diagnostic accuracy of the Meckel’s scan. Pre-medication with histamine-2 blockers (e.g. ranitidine) has been reported to increase the diagnostic yield by inhibiting the excretion of isotope into the bowel lumen, and hence causing its increased concentration in the parietal cells [15]. We have consistently used pre-medication in our patients.
We note that many (161 out of 183) of our Meckel’s scans were negative. In eight of these patients with a negative Meckel’s scan, surgery was performed anyway; in one of these patients a MD with ectopic gastric mucosa was found, which had been missed on the Meckel’s scan (false negative case). In the other patients with a negative Meckel’s scan the presenting clinical symptoms improved without further investigations (in 46 % of the patients) and no further diagnostic tests for a MD were performed. Endoscopy was performed in 52 out of 161 cases (32 %), and this revealed abnormal findings in about 31 out of 52 (children (60 %). We think that in this group of children, who present with non-specific symptoms, an endoscopy should be the preferred investigation rather than the Meckel’s scan. Our median follow-up duration was 2 years and none of the patients with a negative Meckel’s scan re-presented with symptoms suggestive of a MD after their Tc-99m-pertechnetate scan. Therefore, we believe that our negative Meckel’s scans reflect reasonably accurately (from what is possible to ascertain from the clinical context) the absence of a MD with a significantly large area of ectopic gastric mucosa within it. Clearly, if the area of ectopic gastric mucosa is very small this can be missed on the Meckel’s scan (but significant PR bleeding with a drop in haemoglobin would be unlikely to occur). Alternatively, if there is profuse bleeding, the radioisotope can be washed out and the result of the scan can be falsely negative [16]. Our false positive rate was 23 % (5 out 22 scans). False positive results of the Meckel’s scan are well described in the literature. Various conditions can give rise to false positive results such as duodenal and jejunal duplication cysts, intussusception, volvulus, inflammatory bowel disease and post-operative patients [17–19].
Interestingly, we found a positive Meckel’s scan in 20 out of 77 patients (26 %), who presented mainly with PR bleeding. However, only 2 out of 106 children (2 %), who presented with other non-specific symptoms (group 2) had a positive Meckel’s scan. The difference between these two groups was statistically significant. In this patients’ population with abdominal pain but without PR bleeding, the prevalence of MD with ectopic gastric mucosa is very low. In retrospect, we wonder whether a Meckel’s pertechnetate scan was clinically useful in all these patients. In our opinion, a more focussed pattern of referrals, i.e. doing Meckel’s scan initially only in patients who present with PR bleeding (even more so if there is an associated drop in haemoglobin levels) would be more useful. Possibly an endoscopy in the first instance in patients with other non-specific symptoms might be beneficial to reach a diagnosis more rapidly.
Conclusion
The Meckel’s scan retains a high diagnostic accuracy in detecting MD with ectopic gastric mucosa when performed according to the published guidelines. The clinical scenario where this test yields its highest positive result is in patients presenting with painless PR bleeding with a significant drop in haemoglobin. Patients presenting with other non-specific symptoms (such as abdominal pain, possibly associated with nausea and/or vomiting) may be better served with an endoscopy in first instance.
References
Chan KW, Lee KH, Mou JW, Cheung ST, Tam YH (2008) Laparoscopic management of complicated Meckel’s diverticulum in children: a 10 years review. Surg Endosc 22:1509–1512
Levy AD, Hobbs CM (2004) Meckel diverticulum: radiologic features with pathologic correlation. Radiographics 24:565–568
Menezes M, Tareen F, Saeed A, Khan N, Puri P (2008) Symptomatic Meckel’s diverticulum in children: a 16-year review. Pediatr Surg Int 24:575–577
Das PC, Rao PL, Radhakrishna K (1992) Meckel’s diverticulum in children. J Postgrad Med 38:19–20
Cserni G (1996) Gastric pathology in Meckel’s diverticulum review of cases resected between 1965 and 1995. Am J Clin Pathol 106:782–785
Soltero MJ, Bill AH (1976) The natural history of Meckel’s diverticulum and its relation to incidental removal. A study of 202 cases of diseased Meckel’s diverticulum found in King County, Washington, over a fifteen year period. Am J Surg 132:168–173
DeBartolo HM Jr, van Heerden JA (1976) Meckel’s diverticulum. Ann Surg 183:30–33
Ford PV, Bartold SP, Fink-Bennett DM, Jolles PR, Lull RJ, Maurer AH, Seabold JE (1999) Procedure guideline for gastrointestinal bleeding and Meckel’s diverticulum scintigraphy. Society of nuclear medicine. J Nucl Med 40:1226–1232
Sfakianakis GN, Haase GM (1982) Abdominal scintigraphy for ectopic gastric mucosa: a retrospective analysis of 143 studies. Am J Roentgenol 138:7–12
Luckier LS, Dohan O, Li Y, Chang CJ, Carrasco N, Dadachova E (2004) Kinetics of perrhenate uptake and comparative biodistribution of perrhenate, pertechnetate and iodide by NaI symporter-expressing tissues in vivo. J Nucl Med 45:500–507
Poulsen KA, Qvist N (2000) Sodium pertechnetate scintigraphy in detection of Meckel’s diverticulum: is it usable? Eur J Pediatr Surg 10:228–231
Tseng Y, Yang Y (2009) Clinical and diagnostic relevance of Meckel’s diverticulum in children. Eur J Pediatr 168:1519–1523
Cooney DR, Duszynski DO, Camboa E, Karp MP, Jewett TC Jr (1982) The abdominal technetium scan (a decade of experience). J Pediatr Surg 17:611–619
Mariani G, Pauwels EK, AlShaarif A, Marchi S, Boni G, Barreca M, Bellini M, Grosso M, de Bortoli N, Mumolo G, Costa F, Rubello D, Strauss HW (2008) Radionuclide evaluation of the lower gastrointestinal tract. J Nucl Med 49:776–787
Rerksuppaphol S, Hutson JM, Oliver MR (2004) Ranitidine enhanced 99mtechnetium pertechnetate imaging in children improves the sensitivity of identifying heterotopic gastric mucosa in Meckel’s diverticulum. Pediatr Surg Int 20:323–325
Sagar J, Kumar V, Shah DK (2006) Meckel’s diverticulum: a systematic review. J R Soc Med 99:501–505
Kumar R, Tripathi M, Chandrashekar N, Agarwala S, Kumar A, Dasan JB, Malhotra A (2005) Diagnosis of ectopic gastric mucosa using 99Tcm-pertechnetate: spectrum of scintigraphic findings. Br J Radiol 78:714–720
Omar AM, Al-Saee’d TA, Elgazzar A (1998) Scintigraphic pattern of intestinal duplication on a Meckel’s diverticulum scan. Clin Nucl Med 23:708–709
McKevitt EC, Baerg JE, Nadel HR, Webber EM (1999) Laparoscopy as a cause of a false-positive Meckel’s scan. Clin Nucl Med 24:102–104
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sinha, C.K., Pallewatte, A., Easty, M. et al. Meckel’s scan in children: a review of 183 cases referred to two paediatric surgery specialist centres over 18 years. Pediatr Surg Int 29, 511–517 (2013). https://doi.org/10.1007/s00383-013-3270-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-013-3270-3