Abstract
Purpose
Autologous skin substitutes to cover large skin defects are used since several years. Melanocytes, although essential for solar protection and pigmentation of skin, are not yet systematically added to such substitutes. In this experimental study, we reconstructed melanocyte-containing dermo-epidermal skin substitutes from donor skins of different skin pigmentation types and studied them in an animal model. Features pertinent to skin color were analyzed and compared in both skin substitutes and original donor skin.
Methods
Keratinocytes, melanocytes, and fibroblast were isolated, cultured, and expanded from skin biopsies of light- and dark-pigmented patients. For each donor, melanocytes and keratinocytes were seeded in different ratios (1:1, 1:5, 1:10) onto collagen gels previously populated with autologous fibroblasts. Skin substitutes were then transplanted onto full-thickness wounds of immuno-incompetent rats. After 8 weeks, macroscopic and microscopic analyses were conducted with regard to skin color and architecture.
Results
Chromameter evaluation revealed that skin color of reconstructed light- and dark-pigmented skin was very similar to donor skin, independent of which melanocyte/keratinocyte ratio was added. Histological analyses of the skin analogs confirmed these findings.
Conclusion
These data suggest that adding autologous melanocytes to bioengineered dermo-epidermal skin analogs can sustainably restore the patients’ native skin color.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One promising approach to cover large full-thickness skin defects is tissue engineering of skin [1]. Several laboratories worldwide, including our own research group, have been working on this ambitious project and have made substantial progress over the last years [2–5].
At our center, we first used simple autologous cultured epidermal autografts (CEA) for burn and reconstructive surgery [6, 7]. However, they did not fulfill the expectations in that they showed inconsistent CEA take as well as inconsistent functional and esthetic results. Consequently, we invested several years on the development of a near natural dermo-epidermal skin equivalent, based on the hypothesis that a skin substitute closely resembling native skin might ultimately produce more satisfactory clinical results [8–10]. Then, we managed to bioengineer capillaries in vitro in order to prevascularize [11]. Also, we looked at numerous options to strengthen the dermal compartment for better surgical handling and are now successfully working with a compressed hydrogel that serves as dermal template [12]. Finally, and with clinical application in mind, we developed a system to produce large scale (7.5 × 7.5 cm) skin analogs that were favorably tested in a large animal model (pig) [2, 3].
Most recently, we directed our work also at pigmentation that, for obvious reasons, is a crucial issue since it plays a fundamental functional role in terms of skin protection against ultraviolet (UV) radiation, and, in addition, it has a paramount cosmetic impact for the patient. If melanocytes, the cells responsible for skin pigmentation, are missing in skin analogs, the grafts appear unnaturally white like vitiligo-affected areas [13]. Therefore, we have designed a project with the principal goal to provide our autologous human skin analogs with appropriate pigmentation matching as closely as possible the native color present at the presumptive site of transplantation. To achieve this goal, we added human melanocytes in different ratios to the epidermal compartment of laboratory-engineered, human dermo-epidermal skin analogs, tested these in a rat model, and compared the obtained pigmentation features to those of the original donor skin.
Materials and methods
Human skin samples
The study was conducted according to the “Declaration of Helsinki Principles” and after permission by the ethic commission of the Canton Zurich. Parents or patients gave informed consent to use skin samples. The human foreskins used were obtained from light and dark skin pigmentation types from patients 1–16 years of age. The skin samples were used for the isolation of human epidermal keratinocytes, melanocytes, and dermal fibroblasts. Tissues samples for histological examinations were embedded in OCT compound (Sakura Finetek, Switzerland) and kept at −30 °C, or prepared for paraffin sections.
Isolation and culturing of primary cells
Keratinocytes and fibroblasts were isolated and cultured as described in Pontiggia et al. [10], and melanocytes as specified in Böttcher-Haberzeth et al. [8].
Preparation of tissue engineered skin analogs
The skin analogs were prepared as previously described [10]. Briefly, rat collagen type I was mixed with 1 × 105 human dermal fibroblasts (passage 1) and placed in cell culture inserts with membranes of 3.0 μm pore-size (all BD Falcon, Germany). These dermal equivalents were grown in Dulbecco’s modified Eagle’s medium (DMEM, Invitrogen, Switzerland) for 6 days to allow for gel contraction. On each dermal equivalent 5 × 105 keratinocytes and melanocytes (passage 1) of the corresponding donor skin were seeded in different ratios (melanocytes:keratinocytes 1:1, 1:5, or 1:10). The skin analogs were cultured for 1 week in a 1:1 mix of keratinocyte medium (SFM, Invitrogen, Switzerland) and melanocyte growth medium (Promocell, Germany), and subsequently transplanted (Table 1).
Transplantation of tissue engineered skin analogs
The surgical protocol was approved by the local Committee for Experimental Animal Research (permission number 76/2011). Immuno-incompetent female nu/nu rats, 8–10 weeks old (Harlan Laboratories, Netherlands), were prepared and anesthetized as previously described [14, 15]. Skin analogs were transplanted onto full-thickness skin defects created surgically on the backs of the rats. To prevent wound closure from surrounding rat skin and to protect the skin analogs, surgical steel rings (26 mm in diameter) were sutured to the skin defects using non-absorbable polyester sutures (Ethibond®, Ethicon, USA). The skin analogs were covered with a silicone foil (Silon-SES, BMS, USA), a polyurethane sponge (Ligasano, Ligamed, Austria), and a tape as wound dressing. Dressing changes and photographic documentations were performed once per week. After 8 weeks, the transplanted skin analogs were excised in toto and processed for cryo- and paraffin sections and electron microscopy.
Chromameter measurements
The International Commission on Illumination (Commission internationale de l’Eclairage, CIE) principles of 1976 describes a uniform, three-dimensional color space (L*a*b*) because color vision is trichromatic. The L value correlates to perceived lightness. It can range from absolute black (0) to absolute white (+100). As it is the most sensitive of the trichromatic values to skin analog color change, only the L value (mean ± SD) of the reflectance spectroscopy used to measure the visible spectrum of light reflected from the patients’ foreskins and skin analogs was recorded in this study. The spectroscopy was conducted by employing a Chromameter CR-200 (Minolta, Osaka, Japan).
Histological analysis
Paraffin sections (5 μm) were stained with hematoxylin and eosin (Sigma, Switzerland) to assess the histological morphology and with the Fontana Masson technique to visualize melanin [16] in the transplanted skin analogs.
Immunohistochemical staining
Immunofluorescence staining was performed as described in Böttcher-Haberzeth et al. [8, 15]. To detect melanosomes, an anti-melanosome antibody was used (HMB-45, 1:50, Dako, Switzerland). To visualize the basement membrane, a staining against laminin-5 was performed (clone P3H9-2, 1:100, Santa Cruz, Germany). Pictures of immunofluorescence stainings were taken with a DXM1200F digital camera connected to a Nikon Eclipse TE2000-U inverted microscope. The device is equipped with Hoechst 33342-, FITC-, and TRITC-filter sets (Nikon AG, Switzerland; Software: Nikon ACT-1 vers. 2.70). Images were processed with Photoshop 7.0 (Adobe Systems Inc, Germany).
Electron microscopy
For transmission electron microscopy analyses, tissue blocs (approximately 1 mm3) were prefixed in 0.1 M cacodylate buffer (Merck, Germany), pH 7.3 containing 2.5 % glutaraldehyde for 2 h, washed in cacodylate buffer, postfixed with an aqueous solution of 1 % OsO4 and 1.5 % K4Fe(CN)6 for 1 h, dehydrated, and finally embedded in EPON 812 (Catalys AG, Switzerland). Ultrathin sections (approximately 50–70 nm) were collected on copper grids, contrasted with 4 % uranyl acetate and 3 % lead citrate, and examined with a CM 100 transmission electron microscope (Philips, The Netherlands). All reagents were from Sigma unless mentioned otherwise.
Statistical analysis
Melanocytes in the basal layer of the donor skin and of the skin analogs were evaluated by counting HMB-45 positive cells and cell nuclei (Hoechst staining) four times in each of five representative sections from each skin sample. The results were calculated (Microsoft Excel) to display the mean ± SD graphically.
Results
Macroscopic appearance and color measurement of transplants
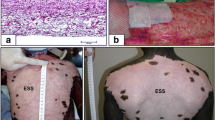
Eight weeks after transplantation, the reconstructed human skin analogs from light- and dark-pigmented donor skin showed a strong resemblance to the latter regarding color and structure, independent of which melanocyte/keratinocyte ratio was used (Fig. 1). Pigmentation was very homogenous and even throughout the entire transplant of all specimens. The chromameter evaluation (L value) of the reconstructed light skin showed a mean deviation from the native light skin of 4.33 % (SD 1.91 %) for the constructs with a 1:1 melanocyte/keratinocyte ratio, of 3.68 % (SD 0.63 %) for the constructs with a 1:5 melanocyte/keratinocyte ratio, and of 1.91 % (SD 3.27 %) for the constructs with a 1:10 melanocyte/keratinocyte ratio. The chromameter evaluation of the reconstructed dark skin showed a mean deviation from the native dark skin of 2.04 % (SD 0.96 %) for the constructs with a 1:1 melanocyte/keratinocytes ratio, of 3.26 % (SD 7.94 %) for the constructs with a 1:5 melanocyte/keratinocyte ratio, and of 0.71 % (SD 5.55 %) for the constructs with a 1:10 melanocyte/keratinocyte ratio.
Macroscopic view of light and dark donor skin and its corresponding tissue engineered skin analogs 8 weeks after transplantation. a Light and b dark donor skin before tissue preparation for cell isolation; c, e, g tissue engineered skin analogs of light skin with a melanocyte/keratinocyte ratio of 1:1, 1:5, and 1:10; d, f, h tissue engineered skin analogs of dark skin with a melanocyte/keratinocyte ratio of 1:1, 1:5, and 1:10. All analogs show a similar color to its donor skin, independent of which melanocyte/keratinocyte ratio was used initially
Epidermal structure
The epidermis of the constructs was comparable to the histology of the donor skin with regard to epidermal stratification, cellular differentiation, and absence of parakeratotic cells (Fig. 2). Results were very similar in both light and dark skin. A noticeable difference between the two was the heavily pigmented basal layer of the dark skin. An obvious difference between the analogs and the donor skin was the absence of rete ridges in the engineered skin.
Histological evaluation of light and dark donor skin and of excised corresponding tissue engineered skin analogs 8 weeks after transplantation (hematoxylin and eosin staining). a Light and b dark donor skin; c, e, g tissue engineered skin analogs of light skin with a melanocyte/keratinocyte ratio of 1:1, 1:5, and 1:10; d, f, h tissue engineered skin analogs of dark skin with a melanocyte/keratinocyte ratio of 1:1, 1:5, and 1:10. All analogs show a well developed, stratified epidermis very comparable to the corresponding donor skin structure. In the dark skin analogs, the heavily pigmented basal layer can easily be detected. Scale bars 50 µm
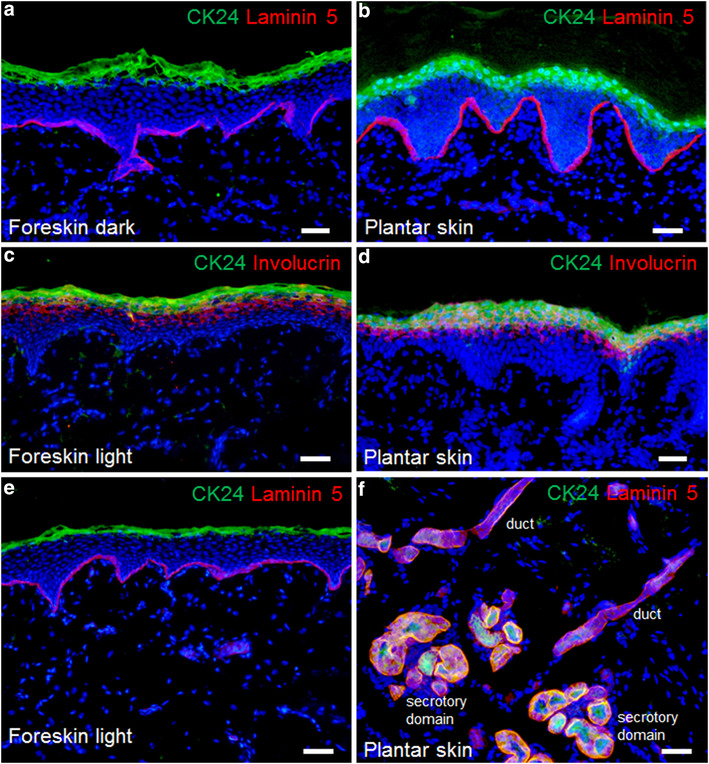
Melanocytes and melanogenesis
HMB-45 staining visualized the melanocytes in the epidermis of the constructs (arrowheads Fig. 3). They resided in a physiologic position in the basal layer with contact to the basal membrane and projected dendrites into the upper layers of the epidermis (arrows Fig. 3). Fontana Masson staining demonstrated the typical melanin distribution within epidermal cells (supranuclear melanin cap) (Fig. 4). There were distinct differences between the light- and dark-pigmented constructs: there was more melanin in dark constructs and, in contrast to light constructs, melanin was found in all epidermal layers. Generally, the engineered constructs showed similar melanin quantities and distribution to the donor skin, independent of which melanocyte/keratinocyte seeding ratio was used.
Melanocyte position in light and dark tissue engineered skin analogs 8 weeks after transplantation. a Representative image of a light tissue engineered skin analog, b representative image of a dark tissue engineered skin analog. Melanocytes are stained with HMB-45 (green), the basement membrane with Laminin-5 (red), cell nuclei are stained with Hoechst (blue). Melanocytes are distributed throughout the basal layer (arrowheads) on the basement membrane. Dendrites can be seen projecting to the upper layers of the epidermis (white arrows). Scale bars 50 µm
Fontana Masson staining of light and dark donor skin and of the excised corresponding tissue engineered skin analogs 8 weeks after transplantation. a Light and b dark donor skin; c, e, g tissue engineered skin analogs of light skin with a melanocyte/keratinocyte ratio of 1:1, 1:5, and 1:10; d, f, h tissue engineered skin analogs of dark skin with a melanocyte/keratinocyte ratio of 1:1, 1:5, and 1:10. Melanin granules stain black. Melanin quantity and distribution in skin analogs is very comparable to the corresponding donor skin, however, much more pronounced in dark skin analogs. Melanin is physiologically arranged as supranuclear caps in all transplants. Scale bars 50 µm
By transmission electron microscopy, the melanosomes inside melanocytes and their dendrites as well as melanin inside keratinocytes was analyzed more in detail (Fig. 5): in the light skin analogs, melanocytes produced less melanin and lighter melanin granules in the melanosomes, whereas melanocytes in the dark skin analogs produced more melanin and darker melanin granules in the melanosomes. The keratinocytes of the light skin constructs contained less pigment than the ones of the dark skin constructs. In both analogs, melanin was arranged in a supranuclear position (supranuclear cap).
Ultrastructural evaluation of light and dark tissue engineered skin analogs 8 weeks after transplantation. a Melanocyte in light tissue engineered skin analog, b melanocyte in dark tissue engineered skin analog, c keratinocyte in light tissue engineered skin analog, d keratinocyte in dark tissue engineered skin analog. Melanocytes (M) are located in the basal layer of the epidermis on the basement membrane (dotted line). The adjacent dermis (D) can be identified by its collagen fibers. Melanin (white arrows) is clearly more pronounced in melanocytes (M) and keratinocytes (K) of the dark skin analog. Dendrites (black arrowheads) can be detected between cells. Scale bars 2 µm
Melanocyte density
The melanocyte/keratinocyte ratio in the basal layer of all analogs was very similar to that in the corresponding donor skin. Results in both, the light- and dark-pigmented skin analogs, were independent of which melanocyte/keratinocyte ratio had been added initially (Fig. 6).
Discussion
This is an experimental study looking at the question whether the original, i.e. “constitutive”, skin color of a patient can be reproduced when melanocytes are added to tissue engineered full-thickness skin analogs. In particular, we looked at the results of reconstructed light- and dark-pigmented skin types when all cell types used (keratinocytes, melanocytes, and fibroblasts) were taken from the same donor skin and melanocytes were added in different ratios. Generally speaking, this study demonstrates that providing bioengineered skin analogs with melanocytes does in fact result in a skin color that is not only subjectively (photographic documentation) but also objectively (chromameter evaluation) almost identical to the color of the native donor skin. A number of aspects call for a detailed comment.
The fact that normal skin color is restored in our skin substitutes indicates that all sophisticated and often multi-step maneuvers from removal of the skin biopsy to cell isolation and culture, to assemblage of the substitutes, to transplantation, to middle-term maturation of the human transplanted skin in a rat model, do not seem to alter the involved cells (keratinocytes, melanocytes, and fibroblasts) in any measurable way. These cells apparently maintain their inherent programs enabling them to communicate and interact with each other and work as a functional epidermal melanin unit (EMU) [17, 18].
Interestingly, the above mentioned color production is independent of the original number of melanocytes added to the constructs. Even a significant deviation from the physiological 1:5 ratio of melanocytes to keratinocytes in the basal layer toward a higher (1:1) and a lower ratio (1:10) of melanocytes to keratinocytes does not result in any measurable color difference. It is known that a minimum density of melanocytes is required to restore pigmentation completely [13]. In our analogs, this minimum number of melanocytes necessary to enable pigmentation of the skin was used.
On a histological level, the macroscopic findings were precisely reflected. Particularly relevant is the fact that melanogenesis and the distribution of melanin transferred to keratinocytes very closely resembled the well-documented pattern known from physiological EMUs [19–21]. Also, the typical differences between light- and dark-pigmented skin types [21, 22] such as poorly pigmented supranuclear melanosomes and melanosome-free upper epidermis in light skin as well as heavily pigmented melanosomes throughout the cytoplasm of keratinocytes and melanosome presence throughout the entire epidermis in dark skin were largely replicated in our skin analogs.
Taken together, there is compelling evidence that adding melanocytes to bioengineered skin substitutes results in an almost physiological restoration of those cellular and molecular processes usually involved in the complex dynamics of skin pigmentation.
The importance of using all three cell types (keratinocytes, melanocytes, and fibroblasts) from the same donor skin must also be highlighted. It is known that keratinocytes, melanocytes, and fibroblasts are highly interactive and communicate with each other via cell/cell contacts and secreted factors to regulate skin phenotype and functionality [21]. In this context, it is crucial to underline the importance of using these three key player cells from the same donor skin sample (as shown here) to reproduce the original skin color in bioengineered skin analogs. Interestingly, combining keratinocytes and melanocytes from one skin pigment type with fibroblasts from another skin pigment type results in disparate skin colors of engineered skin substitutes [22]. Clearly, for clinical applications, the requirement for fully autologous skin substitutes is indispensable for obvious reasons.
With regard to skin physiology, the novel possibility to provide tissue engineered skin analogs with a near natural color represents a significant progress not only in general terms of cosmesis, but especially in terms of cancer prevention and the potential to correct stigmatizing pigmentation defects [23, 24].
This study, however, does not address all important issues regarding this topic. First, we did not generate any data demonstrating that tissue engineered EMUs possess the ability to appropriately react to UV radiation. Definitely, the well-documented up- and down-regulation processes (e.g. PAR-2 receptor expression, melanin production) must be studied in this context [25–28]. Secondly, this study does not provide long-term data. Although the results shown here are amazingly physiological and although there are no obvious reasons why this functional capability should significantly change over time, formal long-term studies must address the question whether hypo- or hyperpigmentation may occur over time [13, 29]. Finally, the evergreen-issue of whether manipulating melanocytes is associated with an increased risk of eventual melanoma-formation must be mentioned. Even though our study period is definitely not sufficiently long to answer these questions and even though we have not looked in detail at markers used for melanoma diagnostic work-up (e.g. S100, Melan A, Ki67), we have not found any irritating histological features indicative of melanocyte dysplasia such as epidermal cluster-formation or dermal compartment invasion.
In conclusion, this is, to the best of our knowledge, the first study demonstrating that adding autologous melanocytes to tissue engineered full-thickness skin analogs allows the so reconstructed skin to produce a near normal skin color almost identical to the native color present in the donor skin. It appears crucial that all three cell types originate from the same donor skin. These findings have significant clinical implications in that transplanting a skin analog containing functional EMUs is much more physiological, protects against harmful UV radiation, and improves cosmetic outcome.
References
Böttcher-Haberzeth S, Biedermann T, Reichmann E (2010) Tissue engineering of skin. Burns 36(4):450–460
Braziulis E, Biedermann T, Hartmann-Fritsch F, Schiestl C, Pontiggia L, Böttcher-Haberzeth S, Reichmann E, Meuli M (2011) Skingineering I: engineering porcine dermo-epidermal skin analogues for autologous transplantation in a large animal model. Pediatr Surg Int 27(3):241–247
Schiestl C, Biedermann T, Braziulis E, Hartmann-Fritsch F, Böttcher-Haberzeth S, Arras M, Cesarovic N, Nicolls F, Linti C, Reichmann E, Meuli M (2011) Skingineering II: transplantation of large scale laboratory-grown skin analogs in a new pig model. Pediatr Surg Int 27(3):249–254
MacNeil S (2007) Progress and opportunities for tissue-engineered skin. Nature 445(7130):874–880
Boyce ST (2001) Design principles for composition and performance of cultured skin substitutes. Burns 27(5):523–533
Gobet R, Raghunath M, Altermatt S, Meuli-Simmen C, Benathan M, Dietl A, Meuli M (1997) Efficacy of cultured epithelial autografts in pediatric burns and reconstructive surgery. Surgery 121(6):654–661
Meuli M, Raghunath M (1997) Burns (Part 2). Tops and flops using cultured epithelial autografts in children. Pediatr Surg Int 12(7):471–477
Böttcher-Haberzeth S, Biedermann T, Pontiggia L, Braziulis E, Schiestl C, Hendriks B, Eichhoff OM, Widmer DS, Meuli-Simmen C, Meuli M, Reichmann E (2012) Human eccrine sweat gland cells turn into melanin-uptaking keratinocytes in stratifying dermo-epidermal skin substitutes. J Invest Dermatol. doi:10.1038/jid.2012.290
Biedermann T, Pontiggia L, Böttcher-Haberzeth S, Tharakan S, Braziulis E, Schiestl C, Meuli M, Reichmann E (2010) Human eccrine sweat gland cells can reconstitute a stratified epidermis. J Invest Dermatol 130(8):1996–2009
Pontiggia L, Biedermann T, Meuli M, Widmer D, Böttcher-Haberzeth S, Schiestl C, Schneider J, Braziulis E, Montaño I, Meuli-Simmen C, Reichmann E (2009) Markers to evaluate the quality and self-renewing potential of engineered human skin substitutes in vitro and after transplantation. J Invest Dermatol 129(2):480–490
Montaño I, Schiestl C, Schneider J, Pontiggia L, Luginbühl JF, Böttcher-Haberzeth S, Biedermann T, Braziulis E, Meuli M, Reichmann E (2010) Formation of human capillaries in vitro: the engineering of pre-vascularized matrices. Tissue Eng Part A 16(1):269–282
Braziulis E, Diezi M, Biedermann T, Pontiggia L, Schmucki M, Hartmann-Fritsch F, Luginbühl J, Schiestl C, Meuli M, Reichmann E (2012) Modified plastic compression of collagen hydrogels provides an ideal matrix for clinically applicable skin substitutes. Tissue Eng Part C Methods 18(6):464–474
Swope VB, Supp AP, Boyce ST (2002) Regulation of cutaneous pigmentation by titration of human melanocytes in cultured skin substitutes grafted to athymic mice. Wound Repair Regen 10(6):378–386
Schneider J, Biedermann T, Widmer D, Montano I, Meuli M, Reichmann E, Schiestl C (2009) Matriderm versus Integra: a comparative experimental study. Burns 35(1):51–57
Böttcher-Haberzeth S, Biedermann T, Schiestl C, Hartmann-Fritsch F, Schneider J, Reichmann E, Meuli M (2012) Matriderm® 1 mm versus Integra® single layer 1.3 mm for one-step closure of full thickness skin defects: a comparative experimental study in rats. Pediatr Surg Int 28(2):171–177
Weiner L, Han R, Scicchitano BM, Li J, Hasegawa K, Grossi M, Lee D, Brissette JL (2007) Dedicated epithelial recipient cells determine pigmentation patterns. Cell 130(5):932–942
Jimbow K, Quevedo WC Jr, Fitzpatrick TB, Szabo G (1976) Some aspects of melanin biology: 1950–1975. J Invest Dermatol 67(1):72–89
Fitzpatrick TB, Breathnach AS (1963) The epidermal melanin unit system. Dermatol Wochenschr 147:481–489
Yamaguchi Y, Hearing VJ (2009) Physiological factors that regulate skin pigmentation. Biofactors 35(2):193–199
Nordlund JJ (2007) The melanocytes and the epidermal melanin unit: an expanded concept. Dermatol Clin 25:271–281
Yamaguchi Y, Brenner M, Hearing VJ (2007) The regulation of skin pigmentation. J Biol Chem 282(38):27557–27561
Yoshida Y, Hachiya A, Sriwiriyanont P et al (2007) Functional analysis of keratinocytes in skin color using a human skin substitute model composed of cells derived from different skin pigmentation types. FASEB J 21(11):2829–2839
Masnari O, Landolt MA, Roessler J, Weingaertner SK, Neuhaus K, Meuli M, Schiestl C (2012) Self- and parent-perceived stigmatisation in children and adolescents with congenital or acquired facial differences. J Plast Reconstr Aesthet Surg. doi:10.1016/j.bjps.2012.06.004
Landolt MA, Buehlmann C, Maag T, Schiestl C (2009) Brief report: quality of life is impaired in pediatric burn survivors with posttraumatic stress disorder. J Pediatr Psychol 34(1):14–21
Hearing VJ (2011) Determination of melanin synthetic pathways. J Invest Dermatol 131(E1):E8–E11
Miyamura Y, Coelho SG, Wolber R, Miller SA, Wakamatsu K, Zmudzka BZ, Ito S, Smuda C, Passeron T, Choi W, Batzer J, Yamaguchi Y, Beer JZ, Hearing VJ (2007) Regulation of human skin pigmentation and responses to ultraviolet radiation. Pigment Cell Res 20(1):2–13
Boissy RE (2003) Melanosome transfer to and translocation in the keratinocyte. Exp Dermatol 12(Suppl 2):5–12
Seiberg M (2001) Keratinocyte-melanocyte interactions during melanosome transfer. Pigment Cell Res 14(4):236–242
Boyce ST, Kagan RJ, Yakuboff KP, Meyer NA, Rieman MT, Greenhalgh DG, Warden GD (2002) Cultured skin substitutes reduce donor skin harvesting for closure of excised, full-thickness burns. Ann Surg 235(2):269–279
Acknowledgments
This work was financially supported by the EU-FP6 project EuroSTEC (soft tissue engineering for congenital birth defects in children: contract: LSHB-CT-2006-037409) by the EU-FP7 project EuroSkinGraft (FP7/2007-2013: grant agreement no 279024), by the EU-FP7 (MultiTERM, grant agreement nr 238551), and by the University of Zurich. We are particularly grateful to the Foundation Gaydoul and the sponsors of “DonaTissue” (Thérèse Meier and Robert Zingg) for their generous financial support and interest in our work.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Böttcher-Haberzeth, S., Klar, A.S., Biedermann, T. et al. “Trooping the color”: restoring the original donor skin color by addition of melanocytes to bioengineered skin analogs. Pediatr Surg Int 29, 239–247 (2013). https://doi.org/10.1007/s00383-012-3217-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-012-3217-0