Abstract
Purpose
Dermal templates, such as Matriderm® and Integra®, are widely used in plastic and reconstructive surgery, often as two-step procedures. A recent development is the application of thin dermal templates covered with split thickness skin grafts in one-step procedures. In this experimental study, we compare the two thin matrices Matriderm® 1 mm and Integra® Single Layer in a one-step procedure with particular focus on neodermis formation.
Methods
Matriderm® 1 mm and Integra® Dermal Regeneration Template—Single Layer (1.3 mm) were compared in a rat model. In three groups of five animals each, a full thickness wound was covered with (a) Matriderm® 1 mm and neonatal rat epidermis, (b) Integra® Single Layer and neonatal rat epidermis, or, (c) neonatal rat epidermis only (control). Histological sections 2 weeks post transplantation were analyzed with regard to take of template and epidermis, neodermal thickness, collagen deposition, vascularization, and inflammatory response.
Results
Take of both templates was complete in all animals. The Matriderm®-based neodermis was thinner but showed a higher cell density than the Integra®-based neodermis. The other parameters were similar in both matrices.
Conclusion
The two templates demonstrate a comparable biological behavior early after transplantation. The only difference was found regarding neodermal thickness, probably resulting from faster degradation of Matriderm®. These preliminary data suggest that both dermal templates appear similarly suitable for transplantation in a one-step procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dermal substitutes are widely used in plastic, reconstructive, and burn surgery since many years [1–8]. Most templates are relatively thick and thus involve a two-step procedure with an interval of several weeks between dermal matrix implantation and skin grafting. Consequently, valuable time is lost and cost increases. Several years ago, a company producing Matriderm® (Matriderm) (Dr. Suwelack Skin & Health Care AG), which is an acellular lyophilized collagen and elastin based biomatrix, introduced a thin (1 mm) dermal template. It has been successfully used in one-step procedures in combination with split thickness skin grafts (STSG) [9–19]. More recently, Integra Life Sciences also developed a thin version, namely Integra® Dermal Regeneration Template Single Layer (Integra Single Layer), an acellular, permanently cross-linked collagen and glycosaminoglycan based biomatrix (1.3 mm). In contrast to the well-established bilayered Integra® Dermal Regeneration Template [3–6, 20, 21], it only consists of a thin dermal regeneration template. Obviously, Integra Single Layer lends itself ideally to also be used in one-stage procedures in combination with STSG, just like Matriderm.
The aim of this experimental study (rat model) was to compare these two thin matrices used in a one-step procedure with a particular focus on neodermis formation.
Methods
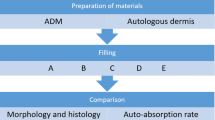
Study design
Matriderm and Integra Single Layer were compared in a one-step procedure on immuno-incompetent rats. In three groups of five animals each, a full thickness skin wound was created and covered with either (a) Matriderm 1 mm and neonatal rat epidermis, (b) Integra Single Layer 1.3 mm and neonatal rat epidermis, or (c) coverage with neonatal rat epidermis only (control). Two weeks later, the transplants were excised and processed for histology.
Materials and methods
Matriderm (thickness 1 mm) (Dr. Suwelack Skin & Health Care AG, Billerbeck, Germany) and Integra Single Layer (thickness 1.3 mm, [7]) (Integra Life Sciences Corporation, Plainsboro, NJ, USA) were cut into round pieces with a diameter of 2.5 cm to exactly fit the transplantation devices (modified Fusenig chambers [22]), and soaked in DMEM (Dulbecco modified Eagle medium, Invitrogen, Carlsbad, CA, USA) for 10 min immediately before implantation.
The surgical protocol was approved by the local committee for experimental animal research (permission number 65/2009). Immuno-incompetent female nu/nu rats, 8–10 weeks old (Harlan Laboratories, The Netherlands), were prepared and anesthetized as previously described [23]. To protect the implant and to prevent wound closure from the surrounding skin, Teflon rings with a diameter of 2.6 cm were sutured into full-thickness skin defects created on the backs of the rats, using non-absorbable polyester sutures (Ethibond®, Ethicon, Piscataway, NJ, USA). In experimental animals, the matrices were inserted into the rings and then covered with neonatal rat epidermis devoid of any dermal elements, so as to avoid potential interference of such dermal remnants with neodermis formation. In control animals, neonatal epidermis was applied directly onto full-thickness defects. The transplants were then covered with a silicone foil (Silon-SES, BMS, Allentown, PA, USA), a polyurethane sponge (Ligasano, Ligamed, Innsbruck, Austria), and a tape as wound dressing. Dressing changes and photographic documentations were performed after 7 and 14 days. The above procedures have been previously described in detail [23].
Analyses of the transplants
After 14 days, the transplant areas were generously excised and processed for cryosections (12 μm thick) as well as for paraffin sections (8 μm thick). Paraffin sections were deparaffinized, stained with haematoxylin and eosin (Sigma, St. Louis, MO, USA), and thereafter mounted within Eukitt® (Fluka, Buchs, Switzerland). This allowed us to assess take of template and epidermal coverage, cell density, and neodermal thickness.
The thickness of the neodermal compartment was measured using the graphic program Image J (http://rsb.info.nih.gov). Repetitive measures from the basal layer of the epidermis to the subcutaneous tissue were taken in different sections from each sample (approximately 50 per sample). The results were analyzed using VassarStats® online software (http://faculty.vassar.edu/lowry/VassarStats.html) performing unpaired Student’s t test. A p < 0.05 was considered significant.
To assess collagen deposition and distribution, paraffin sections were deparaffinized and Masson’s trichrome staining applied. The procedure was performed according to the manufacturer’s description (Kit Sigma-Aldrich HT15).
Vascularization of the neodermis and inflammatory response against the matrix were analyzed by immunostaining. Antibodies against the following cell types were used on cryosections according to the manufacturer’s description: Vascular endothelial cells (anti-CD31, BD Pharmingen), macrophages (anti-Integrin αM, Santa Cruz), and granulocytes (HIS48, Santa Cruz). As a secondary antibody we used TRITC-conjugated polyclonal goat F(ab’)2 fragments directed to mouse or rabbit immunoglobulins (Dako, Baar, Switzerland). Cryosections were fixed and permeabilized in acetone for 5 min at −20°C, air-dried, washed 3× in phosphate-buffered saline (PBS, Invitrogen), and blocked in PBS containing 2% bovine serum albumin (Sigma, Buchs, Switzerland) for 30 min. Incubation with the diluted antibodies was performed in blocking buffer for 1 h at room temperature. Slides were washed three times for 5 min in PBS and blocked for additional 15 min before the second antibody was added. Finally, the slides were incubated for 5 min in PBS containing 1 μg/ml Hoechst 33342 (Sigma, Buchs, Switzerland), washed twice for 5 min in PBS, and mounted with Dako mounting solution (Dako, Baar, Switzerland) containing 25 mg/ml of DABCO anti-quenching agent (Sigma, Buchs, Switzerland).
Pictures of immunofluorescence staining were taken with a DXM1200F digital camera connected to a Nikon Eclipse TE2000-U inverted microscope. The device is equipped with Hoechst 33342, FITC, and TRITC filter sets (Nikon AG, Egg, Switzerland; Software: Nikon ACT-1 vers. 2.70). Images were processed with Photoshop 7.0 (Adobe Systems Inc, Munich, Germany).
Results
Take of templates and epidermal coverage
Two weeks after transplantation we observed a complete take of both templates, Matriderm and Integra Single Layer, in all animals. The substitutes were fully integrated into the rat tissue, as evidenced by complete colonization of the neodermis with rat cells. Cell density was higher in Matriderm-derived neodermis than in Integra Single Layer derived neodermis (Fig. 1). Epidermal take was seen macroscopically and histologically, but was inconsistent in all animals of all three groups (Fig. 1).
Histological evaluation of the excised transplants 14 days after one-step procedure (haematoxylin and eosin staining). a Matriderm, b Integra Single Layer, c control. All transplants show a developed epidermis (between markers), a neodermis formation (M Matriderm-derived neodermis, I Integra Single Layer-derived neodermis, C neodermis of control group), and a populated neodermis. The remaining scaffold elements cannot be discerned. Scale bars 100 μm
Neodermal thickness
In the Matriderm group, neodermal thickness showed a range from 0.47 to 0.60 mm, with a mean thickness of 0.49 mm (SD 0.03 mm). In the Integra Single Layer group, it ranged from 0.59 to 0.85 mm, with a mean thickness of 0.67 mm (SD 0.015 mm). In the control group, it was from 0.10 to 0.34 mm, with a mean thickness of 0.27 mm (SD 0.036 mm). The two template-derived neodermises were significantly thicker than the scar-like neodermis in the control group (Matriderm-derived neodermis p = 0.0029, Integra Single Layer-derived neodermis p = 0.0004). Regarding the template-derived thickness, the Matriderm-derived neodermis was less thick than the Integra Single Layer-derived neodermis, but the difference did not reach statistical significance (p = 0.05).
Collagen deposition
Staining with Masson’s trichrome revealed a beginning, but still scant, collagen deposition in the Matriderm-derived and similarly also in the Integra Single Layer-derived neodermis. The collagen deposition in the control specimen was more pronounced and more homogeneous (Fig. 2).
Masson’s trichrome staining 14 days after one-step transplantation. a Matriderm, b Integra Single Layer, c control. The insert depicts normal rat skin. Collagen stains blue. There is scant collagen deposition in the template-derived neodermises (a and b), while the collagen deposition in the control (c) is more pronounced and more homogenous, but still distinctly less than in normal rat skin (insert of c). Scale bars 100 μm
Vascularization
Staining with CD 31 demonstrated a neodermal capillary network present in a similar way in all three groups. Blood vessels could be seen from the subcutaneous structures up to the superficial neodermal areas (Fig. 3).
Neovascularization 14 days after one-step transplantation. a Matriderm, b Integra Single Layer, c control. Endothelial cells are stained with CD31 (red), collagen in Integra Single Layer exhibits autofluorescence (green), cell nuclei are stained with Hoechst (blue). No autofluorescence is observed with Matriderm. The dotted line indicates the basement membrane. A neodermal capillary network can be seen from the subcutaneous structures up to the superficial neodermal areas in all three groups. Scale bars 50 μm
Inflammatory response
There were few granulocytes infiltrating the template-derived neodermises, while the number of granulocytes present in control specimens was even lower. The findings regarding macrophage infiltration were almost identical to granulocyte infiltration (Figs. 4, 5).
Inflammatory response (granulocytes) 14 days after one-step transplantation. a Matriderm, b Integra Single Layer, c control. Granulocytes are stained with Granulocyte antibody HIS48 (red), collagen in Integra Single Layer exhibits autofluorescence (green), cell nuclei are stained with Hoechst (blue). Few granulocytes infiltrating the template-derived neodermises (a and b) can be detected, while only single granulocytes are present in the control group (c). Scale bars 50 μm
Inflammatory response (macrophages) 14 days after one-step transplantation. a Matriderm, b Integra Single Layer, c control. Macrophages are stained with Integrin αM (red), collagen in Integra Single Layer exhibits autofluorescence (green), cell nuclei are stained with Hoechst (blue). There are few macrophages infiltrating the template-derived neodermises (a and b), while only single macrophages can be seen in the control group (c). Scale bars 100 μm
Discussion
This appears to be the first study comparing Matriderm 1 mm and Integra Single Layer 1.3 mm in a small animal model. In the global picture, these two templates do not demonstrate significant differences in their biological behavior early after transplantation in that template and epidermal take rate, vascularization, and inflammatory response were comparable.
Clearly, the perfect template take rate, the prompt vascularization, and the relatively low-grade inflammatory response are favorable parameters with regard to clinical applicability. There are several publications indicating that 1 mm thick Matriderm can successfully be used clinically in a one-step procedure [13, 14, 16–18]. In contrast, there is only one publication describing the successful use of 1.3 mm thick Integra Single Layer in combination with a split thickness skin graft to reconstruct deep facial defects in a one-step procedure [24]. The existence of many more articles concerning Matriderm is probably due to the fact that it has been available since several years, whereas Integra Single Layer has only recently been put in the market.
A particularly promising finding is the fact that the template-based neodermal compartments were clearly, and significantly thicker than the one in the controls, thereby approximating the physiological dermal–epidermal ratio. It is conceivable that this positive feature remains also in the long run and provides the reconstructed skin with a near normal texture, mechanical stability, and adequate elasticity. There was also a certain difference in thickness between the two template-derived neodermises. The most tenable explanation for this phenomenon is a more rapid degradation of Matriderm because its collagen components are (as opposed to Integra Single Layer) not cross-linked. It is well known that crosslinking reinforces matrix stability and makes it less susceptible to degradation (increased resistance against enzymatic digestion) [7, 25, 26]. Yet, a potentially adverse effect of crosslinking is that degradation products can decrease cell survival, proliferation, and adhesion [7, 26], which could explain the lower cell density observed in the Integra Single Layer-derived neodermis.
Astonishingly, the take of the neonatal rat epidermis was almost identically inconsistent in all the groups, explicitly also including the control group. We therefore assume that these problems do not reflect different properties of the templates used, but rather have to do with the fact that the epidermal coverage was extremely thin (2–3 cell layers only!), fragile, and devoid of fibroblasts and collagen. Of note, multiple publications have underscored bad and inconsistent take rates after applying cultured epithelial autografts that share many structural characteristics with the epidermal grafts used here [27–29]. Notably, in a clinical setting, STSG used for coverage by definition, contain a dermal component including fibroblasts and collagen fibres. Therefore, such take problems will most likely not occur, as also evidenced by several publications already showing successful outcomes and rapid wound coverage in one-step procedures using STSG [30, 31].
In summary, this is apparently the first experimental study to compare Matriderm 1 mm and Integra Single Layer 1.3 mm with particular focus on their suitability for a one-step application to close deep skin defects. Our data suggest that both dermal templates can be successfully implanted and that both demonstrate a similarly favorable biological behavior in terms of take, vascularization, and inflammatory response. Thus, both qualify for a one-step procedure.
References
Abbas Khan MA, Chipp E, Hardwicke J, Srinivasan K, Shaw S, Rayatt S (2010) The use of Dermal Regeneration Template (Integra®) for reconstruction of a large full-thickness scalp and calvarial defect with exposed dura. J Plast Reconstr Aesthet Surg 63(12):2168–2171
Böttcher-Haberzeth S, Biedermann T, Reichmann E (2010) Tissue engineering of skin. Burns 36(4):450–460
Schiestl C, Stiefel D, Meuli M (2010) Giant naevus, giant excision, eleg(i)ant closure? Reconstructive surgery with Integra Artificial Skin to treat giant congenital melanocytic naevi in children. J Plast Reconstr Aesthet Surg 63(4):610–615
Schiestl C, Neuhaus K, Biedermann T, Böttcher-Haberzeth S, Reichmann E, Meuli M (2011) Novel treatment for massive lower extremity avulsion injuries in children: slow, but effective with good cosmesis. Eur J Pediatr Surg 21(2):106–110
Stiefel D, Schiestl CM, Meuli M (2009) The positive effect of negative pressure: vacuum-assisted fixation of Integra artificial skin for reconstructive surgery. J Pediatr Surg 44(3):575–580
Stiefel D, Schiestl C, Meuli M (2010) Integra Artificial Skin for burn scar revision in adolescents and children. Burns 36(1):114–120
van der Veen VC, van der Wal MB, van Leeuwen MC, Ulrich MM, Middelkoop E (2010) Biological background of dermal substitutes. Burns 36(3):305–321
Weigert R, Choughri H, Casoli V (2010) Management of severe hand wounds with Integra® dermal regeneration template. J Hand Surg Eur 36(3):185–193
Atherton DD, Tang R, Jones I, Jawad M (2010) Early excision and application of Matriderm with simultaneous autologous skin grafting in facial burns. Plast Reconstr Surg 125(2):60e–61e
Cervelli V, Lucarini L, Cerretani C, Spallone D, Palla L, Brinci L, De Angelis B (2010) The use of Matriderm and autologous skin grafting in the treatment of diabetic ulcers: a case report. Int Wound J 7(4):291–296
Cervelli V, Brinci L, Spallone D, Tati E, Palla L, Lucarini L, De Angelis B (2011) The use of Matriderm(®) and skin grafting in post-traumatic wounds. Int Wound J 8(4):400–405
Greenwood JE, Mackie IP (2011) Neck contracture release with Matriderm collagen/elastin dermal matrix. Eplasty 22(11):e16
Haslik W, Kamolz LP, Nathschläger G, Andel H, Meissl G, Frey M (2007) First experiences with the collagen-elastin matrix Matriderm as a dermal substitute in severe burn injuries of the hand. Burns 33(3):364–368
Haslik W, Kamolz LP, Manna F, Hladik M, Rath T, Frey M (2010) Management of full-thickness skin defects in the hand and wrist region: first long-term experiences with the dermal matrix Matriderm. J Plast Reconstr Aesthet Surg 63(2):360–364
Heckmann A, Radtke C, Rennekampff HO, Jokuszies A, Weyand B, Vogt PM (2011) One-stage defect closure of deperiosted bone and exposed tendons with Matriderm® and skin transplantation: possibilities and limitations. Unfallchirurg May 15 [Epub ahead of print] German
Ryssel H, Gazyakan E, Germann G, Ohlbauer M (2008) The use of Matriderm in early excision and simultaneous autologous skin grafting in burns–a pilot study. Burns 34(1):93–97
Ryssel H, Radu CA, Germann G, Otte M, Gazyakan E (2010) Single-stage Matriderm® and skin grafting as an alternative reconstruction in high-voltage injuries. Int Wound J 7(5):385–392
Ryssel H, Germann G, Kloeters O, Gazyakan E, Radu CA (2010) Dermal substitution with Matriderm(®) in burns on the dorsum of the hand. Burns 36(8):1248–1253
van Zuijlen PP, van Trier AJ, Vloemans JF, Groenevelt F, Kreis RW, Middelkoop E (2000) Graft survival and effectiveness of dermal substitution in burns and reconstructive surgery in a one-stage grafting model. Plast Reconstr Surg 106(3):615–623
Branski LK, Herndon DN, Pereira C, Mlcak RP, Celis MM, Lee JO, Sanford AP, Norbury WB, Zhang XJ, Jeschke MG (2007) Longitudinal assessment of Integra in primary burn management: a randomized pediatric clinical trial. Crit Care Med 35(11):2615–2623
Moiemen N, Yarrow J, Hodgson E, Constantinides J, Chipp E, Oakley H, Shale E, Freeth M (2011) Long-term clinical and histological analysis of Integra dermal regeneration template. Plast Reconstr Surg 127(3):1149–1154
Fusenig NE, Breitkreutz D, Dzarlieva RT, Boukamp P, Bohnert A, Tilgen W (1983) Growth and differentiation characteristics of transformed keratinocytes from mouse and human skin in vitro and in vivo. J Invest Dermatol 81:168s–175s
Schneider J, Biedermann T, Widmer D, Montano I, Meuli M, Reichmann E, Schiestl C (2009) Matriderm versus Integra: a comparative experimental study. Burns 35(1):51–57
Koenen W, Felcht M, Vockenroth K, Sassmann G, Goerdt S, Faulhaber J (2011) One-stage reconstruction of deep facial defects with a single layer dermal regeneration template. J Eur Acad Dermatol Venereol 25(7):788–793
Yannas IV, Burke JF, Gordon PL, Huang C, Rubenstein RH (1980) Design of an artificial skin. II. Control of chemical composition. J Biomed Mater Res 14:107–132
McKegney M, Taggart I, Grant MH (2001) The influence of crosslinking agents and diamines on the pore size, morphology and the biological stability of collagen sponges and their effect on cell penetration through the sponge matrix. J Mater Sci Mater Med 12:833–844
Gobet R, Raghunath M, Altermatt S, Meuli-Simmen C, Benathan M, Dietl A, Meuli M (1997) Efficacy of cultured epithelial autografts in pediatric burns and reconstructive surgery. Surgery 121(6):654–661
Meuli M, Raghunath M (1997) Burns (Part 2). Tops and flops using cultured epithelial autografts in children. Pediatr Surg Int 12(7):471–477
Raghunath M, Meuli M (1997) Cultured epithelial autografts: diving from surgery into matrix biology. Pediatr Surg Int 12(7):478–483
Adams DC, Ramsey ML (2005) Grafts in dermatologic surgery: review and update on full- and split-thickness skin grafts, free cartilage grafts, and composite grafts. Dermatol Surg 31(8 Pt 2):1055–1067 (Review)
Muller MJ, Nicolai M, Wiggins R, MacGill K, Herndon DN (1996) Modern treatment of a burn wound. In: Herndon DN (ed) Total Burn Care. Saunders, London, pp 136–147
Acknowledgments
This work was financially supported by EU-FP6 project EuroSTEC (soft tissue engineering for congenital birth defects in children: contract: LSHB-CT-2006-037409) and by the University of Zurich. We are particularly grateful to the Foundation Gaydoul and the sponsors of “DonaTissue” (Thérèse Meier, Robert Zingg, the Vontobel Foundation, and the Werner Spross Foundation) for their generous financial support and interest in our work.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
S. Böttcher-Haberzeth and T. Biedermann contributed equally to this paper.
Rights and permissions
About this article
Cite this article
Böttcher-Haberzeth, S., Biedermann, T., Schiestl, C. et al. Matriderm® 1 mm versus Integra® Single Layer 1.3 mm for one-step closure of full thickness skin defects: a comparative experimental study in rats. Pediatr Surg Int 28, 171–177 (2012). https://doi.org/10.1007/s00383-011-2990-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-011-2990-5