Abstract
Purpose
We aim to analyze differences in functional outcomes in children operated on for Hirschsprung’s disease (HD) using the Paediatric incontinence/constipation scoring system (PICSS) validated in a normative group.
Methods
A retrospective review of the records of all children operated on for HD between 1997 and 2010 was performed. Patients had either a Soave or transanal endorectal pull-through. Children with total colonic aganglionosis and Down’s syndrome were excluded. Utilizing the PICSS children who scored below their age-specific lower limit 95 % confidence interval PICSS scores were considered to have incomplete continence or constipation. The rates of incomplete continence and constipation were compared between groups. Significance was set at p < 0.05.
Results
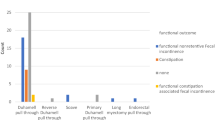
PICSS analysis could be completed in 51 (Soave 35, transanal 16). The median age at interview was 71 months (range 6–191 months). The rate of incomplete continence was 75 % (n = 21) and 71 % (n = 10) for the Soave and transanal groups, respectively (p = 1.00). The constipation rate was 34 % (n = 12) and 25 % (n = 4) for the Soave and transanal groups, respectively (p = 0.74). The overall rates of incomplete continence and constipation rates were 74 and 31 %, respectively, compared with 14 and 10 %, respectively, when rates were calculated by review of records.
Conclusion
The PICSS is a sensitive tool for assessing functional outcome post HD surgery. The Soave and transanal procedures have similar functional outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The evolution of surgical options for the successful management of Hirschsprung’s disease (HD) has been driven by the aspirations of paediatric surgeons to achieve near-perfect functional outcomes. Since Swenson described recto-sigmoidectomy and a colo-anal anastomosis for the treatment of HD in 1948 [1] several new techniques have emerged [2–4]. Controversies still persist as to which technique offers the best outcome. The absence of incontinence and constipation remains the most important marker of a good outcome. The methods of assessment of such functional outcomes post pull-through surgery has varied widely across the literature. Specified, unspecified, tested and untested scoring systems have all been used in these studies [5–14].
It is now accepted that assessment of outcomes such as constipation and incontinence requires a scoring system that can assess subjective symptoms objectively; for this purpose we propose the use of the Paediatric incontinence/constipation scoring system (PICSS) developed by Fichtner-Feigl et al. [15]. Any demonstrable superiority of one technique over the other will be highly desirable to both the surgeon and their patients.
We aim to compare the postoperative constipation and incontinence rates between children operated on for HD utilizing either a modified Soave’s extramucosal endorectal pull-through [3] or the transanal endorectal pull-through procedure [4].
Methods
Patients
This study was carried out at Our Lady’s Children’s Hospital in Dublin Ireland after obtaining ethical approval from the hospital ethics board. The hospital in-patient enquiry (HIPE) system was used to generate a list of children diagnosed and treated with HD between January 1997 and December 2010 and a retrospective review of their records was performed to obtain demographic, intra-operative and post-operative data.
The diagnosis of HD was made by rectal suction biopsy; older children had an open partial thickness rectal biopsy. The children selected had either a modified Soave’s extramucosal endorectal pull-through or a transanal endorectal pull-through procedure. Cases of total colonic aganglionosis due to the extent of resection required and consequent worse outcome were excluded [16]. Children with trisomy 21 were excluded as functional outcomes for a variety of reasons have been shown to be worse in this population [16–18]. Children with other co-morbidities that affect bowel function were excluded; these were mainly hypothyroidism, ano-rectal malformation and syndromic conditions that impair normal global development. Finally, children who still had an intestinal stoma postoperatively or had undergone an antegrade continence enema (ACE) procedure were not suitable for assessment by the PICSS and were thus excluded.
The children selected were 3 months to 15 years post pull-through surgery at the time of interview. Incontinence was assessed in children over 35 months old as toilet training is expected by this age [15].
Surgical technique
Two pull-through procedures were compared: a modification of Soave’s original extramucosal endorectal pull-through procedure [3] and the purely transanal endorectal pull-through procedure [4, 19]. The major modifications to the Soave procedure were a primary colo-anal anastomosis and a split in the posterior wall of the rectal muscle cuff. For both techniques, intraoperative frozen section biopsies were used to confirm the transition zone prior to pull-through. These procedures were carried out by six experienced surgeons in a reasonably standard fashion.
Assessment of functional outcome
Telephone and out-patient clinic interviews utilizing the PICSS were performed with the parents of the 51 children that met the inclusion criteria.
The PICSS questionnaire (Table 1) scores incontinence and constipation [15]. 99 children (76 normal children and 23 with anorectal functional disorders; mean age 4 years and 8 months, SD 32.9 months) were evaluated by a questionnaire with 37 variables. 13 variables were then selected and ascribed values by factor analysis; three variables proved to be decisive for the incontinence score only, five for the constipation score only and five were equally involved in both. The authors then validated the 13 variables (PICSS) by testing them on 122 normal children and arrived at age-specific mean scores and 95 % confidence intervals (CI) for incontinence and constipation. There were three options to each question and the child’s parents were asked to pick one. Each answer had a corresponding score and at the end of the interview the scores were added to give a total for incontinence and constipation. Scores that fell within the age-specific 95 % confidence interval can be interpreted to mean absence of incontinence or constipation. Scores below the 95 % CI reflects incomplete continence and constipation symptomatology, respectively.
Finally, to assess the results obtained using the PICSS we reviewed the records of the same cohort of patients looking for documented problems with continence and constipation that were actively being managed. Incontinence and constipation rates were then calculated by this means.
Statistical analysis
Statistical analysis of Demographic, intra-operative and post-operative data between groups utilized the Fisher’s Exact test for nominal categories and the Student’s t test for continuous dependent variables.
Utilizing the PICSS, children who scored below their age-specific lower limit 95 % confidence interval (CI) scores were considered to have incomplete continence or are constipated. The number of children with such poor scores for incontinence and constipation were then compared between the Soave and transanal groups utilizing the Fisher’s Exact test. Significance was set at p < 0.05. The Statistics Online Computational Resource (SOCR) was used for analysis.
Results
Demographics
From January 1997 to December 2010, 128 children were diagnosed and treated for HD at our institution. There were seven children with total colonic aganglionosis and 23 (17.9 %) diagnosed with Down's syndrome. Seven children still have a stoma while two have undergone an ACE procedure. Eight children without Down’s syndrome had a Swenson’s pull-through, operative records were unavailable for six (their pull-through surgery was performed at other institutions) and one child had passed away. Seventy-three children met the other inclusion criteria; however, the parents of only 51 children were reachable for PICSS analysis (35 Soave and 16 transanal); their demographic and peri-operative characteristics are shown in Table 2.
Children who presented shortly after birth up to age 6 months were classified as ‘neonatal’ presenters and over 6 months ‘chronic’ presenters. If acute abdominal distension, fever and diarrhoea prompted the diagnosis of HD, they were classified as ‘enterocolitis’ presenters. The transanal and Soave groups did not differ in their mode of presentation (p = 0.096).
The transition zone was either classical segment implying disease limited to the proximal sigmoid colon or long segment which involved the descending colon up to the hepatic flexure. Classical segment disease was the more common form in both groups (91 % soave vs. 100 % transanal; p = 0.543). It is standard practice at our institution to perform contrast enemas prior to transanal pull-through to assess the degree of colonic involvement as longer segment disease requires colonic mobilization either laparoscopically or via an umbilical incision [19] and because of this recommendation a transabdominal rectal mucosal dissection (Soave) was the preferred choice for long segment disease. All the transanal procedures in our series were purely transanal without any abdominal colonic mobilization.
As shown in Table 2, the transanal and Soave groups had similar age at diagnosis (p = 0.659), age at surgery (p = 0.882), age at PICSS interview (p = 0.769), duration of stay in hospital post surgery (p = 0.149), prevalence of chronic laxative use (p = 1.000) and the follow-up duration which was defined as the time between surgery and PICSS analysis was also similar between both groups (p = 0.803). Chronic laxative use was defined as consistent use of laxatives to achieve bowel motions for continuous periods of at least 4 weeks at a time.
Functional outcomes
Table 3 shows the mean age-related constipation scores of the transanal and Soave groups and normative scores for each age group arrived at by Fichtner-Feigl et al. [15].
In order to compare the mean scores of the study groups and the normal population age-corrected scores were required. To accomplish this, standard deviations were computed from the mean and confidence interval provided from the normative group. From this data, Z scores were then calculated for each individual at their corresponding age interval. The mean age-corrected Z scores of the Soave and transanal groups and results of analysis comparing groups to each other and to the normative group are shown in Table 4. As the results are age-corrected, they can be combined across age groups.
Both groups and the total study population’s mean constipation scores were worse than the mean scores of the normative group. There was no difference in mean constipation Z scores of the Soave and transanal groups (p = 0.463).
However, since constipation is present when scores are less than the age-related 95 % lower limit CI, a more robust analysis of the prevalence of constipation between groups will be to compare the number of children who had such low scores. The result of this analysis is summarized in Table 5. Comparing the constipation rates between the two groups, 12 (34 %) children in the Soave group while 4 (25 %) children in the transanal group had constipation; (p = 0.746).
Similarly, in children over 35 months of age the mean incontinence scores of both transanal and Soave groups were significantly worse than the mean scores of the normative group; however, there was no statistical difference between the two groups (p = 0.37; Table 6).
The prevalence of incomplete continence (percentage of children with incontinence scores below the lower limit 95 % CI of normative scores) was assessed in both groups and is summarized in Table 5. The rates for the Soave and transanal groups were 75 % (n = 21) and 71 % (n = 10), respectively; there was no significant difference in rates between both groups (p = 1.000).
By review of the records, for children of age over 35 months (n = 42) four children in the Soave group (14 %) and two in the transanal group (14 %) had ongoing problems with incontinence that were actively being managed; overall, the incontinence rate was 14 %. Similarly for constipation (n = 51), the rates by review of their records were 13 % (n = 2) for transanal and 9 % (n = 3) for the soave group and 10 % overall.
Discussion
The goal of surgical treatment for Hirschsprung’s diseases is to enable the affected child have regular spontaneous bowel motions without soiling. The complication of constipation can be so severe that chronic laxative use, further procedures like botulinum injections to the internal sphincter, internal sphincterotomy and even redo-pull through procedures become necessary; it can also predispose to a high incidence of enterocolitis which can be fatal. Incontinence especially in the older child can be socially embarrassing, be difficult to cope with by the family, lead to poor school performance and thus negatively impact on the child’s quality of life [20, 21]. When severe, incontinence can cause perianal excoriations that can be so debilitating that a colostomy becomes necessary to manage the problem.
Therefore, how these subjective symptoms are assessed after pull-through surgery is extremely important. Some studies rely on retrospective reviews with no clear criteria for defining continence and constipation. Others rely on interviews of the children/parents or documentation of unfavourable outcomes in the patients records with no clear cut criteria of how the severity and chronicity of constipation was established as even children without HD do get constipated from time to time; the distinction between occasional soiling and significant incontinence is also occasionally not well established. Some papers have designed scoring systems and interviews that have either not been specified or tested in their efficacy of properly evaluating constipation and incontinence at different stages of a child’s development [5–14].
We applied the PICSS developed by Fichtner-Feigl et al. [15] to compare functional results after two widely used pull-through procedures for HD: the modified Soave extramucosal endorectal pull-through [3] and the purely transanal endorectal pull-through [4]. This questionnaire (Table 1) was unambiguous, user friendly and not time consuming to complete. Mothers provided clear concise answers and were quite knowledgeable on the stooling patterns of the children. Importantly in the development of this questionnaire the symptom of soiling was ascribed to constipation and not incontinence. Soiling is a manifestation of overflow in a constipated child rather than true incontinence, and previous authors have pointed out the limitations/importance of questionnaires differentiating genuine incontinence from overflow incontinence and occasional soiling [13, 16].
The modified Soave extramucosal endorectal pull-through and the purely transanal endorectal pull-through are both standard and widely used procedures. There are, however, key differences that may theoretically explain an improved, if any, outcome in one over the other.
During the transanal procedure the tendency to excessively retract the anal sphincter during mucosal dissection, control of vessels and colonic mobilization may damage the sphincter mechanism [12, 22, 23]. To avoid this complication De la Torre et al. [19] recommend traction on the mucosal tube to pull the bowel down and perform the dissection outside the anus without the need for retraction while Tannuri et al. [23] recommend sacral anaesthesia to induce relaxation of both internal and external sphincters making transanal dissection easier. This theoretical injury to the sphincter mechanism from a transanal dissection has not been corroborated on manometric findings in some series [24, 25] and a clinical correlation to increased soiling was not demonstrated by Stensrud et al. [13]. However, Levitt et al. [22] found that majority of the children referred to their centre for management of incontinence post HD pull-through had undergone a transanal procedure. With a transabdominal dissection and mobilization used in the Soave procedure this potential problem does not arise. Post transanal pull-through, Zhang et al. found that in patients with frequent stools and soiling there was a loss of the natural sigmoid loops on contrast enema and the pulled through colon had a straight course; this was particularly seen in aganglionic segments over 30 cm. They also showed that the pulled through colon which is under some tension leads to a loss of the normal ano-rectal angle [9, 26]. We believe the lack of intra-abdominal mobilization results in a taut pull-through colon preventing the puborectalis from creating this ano-rectal angle. For this reason if the transition zone is more proximal than the mid-sigmoid it has been recommended that a transabdominal mobilization of the colon with occasional division of the middle colic be performed to achieve length and avoid undue tension [19]. Furthermore, in a transanal pull-through there may be a tendency to commence the mucosal dissection and subsequently the anastomosis too close to the dentate line [12, 22]. This disrupts sensory innervations just above the dentate line which on contact with faeces reflexly cause activation of motoneurones of the pudendal nerve to the external sphincter to cause reinforcement of its contraction to maintain continence; these nerves also help to distinguish between gas, liquid and solid. The ideal point to commence this mucosal dissection in most opinions range from 0.5 to 1 cm above the dentate line in the newborn and 1.0–2.0 cm above the dentate line in the older larger child [27]. An anastomosis below the dentate line will result in incontinence [22, 28]. With a transabdominal approach the opposite is true as it can be occasionally difficult to complete the mucosal dissection distal enough to a suitable distance above the dentate line, and an anastomosis too proximal from the dentate line will result in persistence of obstructive symptoms due to the relative aganglionosis at this level. There is a tendency to leave a longer rectal muscle cuff when performing the soave technique. It has been postulated that a long rectal muscle cuff may predispose to constipation and the cuff may roll down and form a constricting ring around the pulled-through bowel; to avoid this many authors recommend a shorter cuff [19]. However, Nasr et al. [29] did not find an increased incidence of constipation and enterocolitis between patients who had a long or short cuff. Furthermore, the rectal muscle cuff is prone to internal sphincter achalasia. This non relaxing internal sphincter may be the reason for constipation in some children and utilizing manometric pressure profiles Keshtgar et al. [30] demonstrated higher resting anal pressures and lower resting rectal pressures in constipated children post pull-through. For this reason a sphincterotomy is performed by splitting the rectal muscle cuff posteriorly for a variable distance particularly during the Soave procedure. During the transanal procedure, the much shorter rectal muscle cuff is sometimes not split because with a shorter cuff (1–3 cm) this step may not be necessary [19]. Finally with inadequate mobilization of the colon during the transanal procedure, tension on the anastomosis may lead to an ischaemic stricture which may result in an acquired aganglionosis that can cause post pull-through constipation [19, 26].
Despite these variable predictors of outcome described above our analysis did not demonstrate an improved outcome in either constipation or incontinence when the soave technique was compared with the transanal technique.
There was, however, a high rate of incomplete continence for both procedures (75 % for Soave, 71 % transanal and 74 % overall). It must be highlighted that this analysis groups incontinence of variable severity together. Children with very poor scores who clinically may be severely incontinent have been grouped with children who are only a few points below the lower limit 95 % CI of normal scores and clinically may correlate to only having occasional soiling accidents with no social consequence. Therefore, aside from the features of each procedure described above that may biologically affect continence, the sensitivity of the PICSS questionnaire in diagnosing this problem and its inability to grade differing severity of poor functional outcomes must be taken into consideration. This is further evident in this cohort as when incontinence and constipation were assessed by reviewing the records and calculating the documented incidence of the complication of incontinence, the rates were 14 % for the soave group (n = 4), the transanal (n = 2) and overall. Similarly, the constipation rates by review of their records were 13 % (n = 2) for transanal and 9 % (n = 3) for the soave group and 10 % overall. This may also mean that there is a lot of underreporting by parents and children adapt over time to poor results, coupled with inadequate documentation/history taking at follow-up all leading to a false picture of normal functional outcome [7]. These findings are similar to those of Catto-smith et al. [31] who showed that faecal soiling was reported more frequently when questionnaires were used (80 %) compared with soiling rates obtained from medical records (44 %).
A pooled sample of about 9,000 patients arrived at an overall incontinence rate of 7.1 % [32]. Menezes et al. [10] reported a range of 3 to 53 % in the literature. Some series which have been criticised for not clearly defining occasional soiling and true incontinence [7] have reported rates as low as 1.1–3.2 % [33]. Fortuna et al. [6] by use of questionnaire arrived at incontinence rates of 75 % in patients less than 5 years post-pull through and 0 % in those older than 15 years post pull-through.
Similarly, a pooled sample of almost 8,000 patients revealed an overall constipation rate of 7.9 % [32]. Again, Menezes et al. [10] reported ranges in the literature from 6 to 34 % and some series report rates as high as 56 % [34].
These variable results reflect the need for an international consensus on a scoring system to critically analyse functional outcome after surgical treatment of HD.
In this retrospective study, the Soave and transanal procedures were carried out by up to six surgeons and this was a limiting factor. The performance of a particular procedure was due to the surgeon’s own personal preference for that procedure and the suitability of the child for that procedure. Meaningful post hoc analyses could not be performed on the surgeon factor given the many levels of this factor (6 surgeons) and multiple cells with only one data point (some surgeons performed only 1 procedure within this cohort during the study period). Accounting for each surgeon’s experience and subtle variations, if any, to the procedures would have improved the sensitivity of our results. Furthermore, in applying the PICSS for assessing functional outcomes the few participants contactable was another limitation.
In conclusion, the Soave and transanal techniques have similar poor functional results post operatively. These poor results which may improve with time [6, 7, 10, 35] suggest that the surgical treatment of Hirschsprung’s disease has not yet been perfected. The PICSS has been shown to be an efficient means of assessing constipation and incontinence. We propose the use of the PICSS as the internationally accepted standard for assessment of functional outcomes after HD surgery and recommend conducting multi-centre prospective analysis of outcomes with larger samples.
References
Swenson O, Bill AH (1948) Resection of rectum and rectosigmoid with preservation of the sphincter for benign spastic lesions producing megacolon; an experimental study. Surgery 24(2):212–220
Duhamel B (1960) A new operation for the treatment of Hirschsprung’s disease. Arch Dis Child 35:38–39
Soave F (1964) A new surgical technique for treatment of Hirschsprung’’s disease. Surgery 56:1007–1014
De la Torre-Mondragon L, Ortega-Salgado JA (1998) Transanal endorectal pull-through for Hirschsprung’s disease. J Pediatr Surg 33(8):1283–1286
Quinn FMJ FR, Guiney EJ, Puri P et al. (1992) Hirschsprungs’s disease: a follow-up of three surgical techniques, 1979-88. In: Hadziselimovic F HB (ed) Pediatric gastroenterology: inflammatory bowel diseases and morbus Hirschsprung. Kluwer Academic Publishers, pp 297–301
Fortuna RS, Weber TR, Tracy TF et al (1996) Critical analysis of the operative treatment of Hirschsprung’s disease. Arch Surg 131(5):520–524
Yanchar NL, Soucy P (1999) Long-term outcome after Hirschsprung’s disease: patients’ perspectives. J Pediatr Surg 34(7):1152–1160
Minford JL, Ram A, Turnock RR et al (2004) Comparison of functional outcomes of Duhamel and transanal endorectal coloanal anastomosis for Hirschsprung’s disease. J Pediatr Surg 39(2):161–165
Zhang SC, Bai YZ, Wang W et al (2005) Clinical outcome in children after transanal 1-stage endorectal pull-through operation for Hirschsprung disease. J Pediatr Surg 40(8):1307–1311
Menezes M, Corbally M, Puri P (2006) Long-term results of bowel function after treatment for Hirschsprung’s disease: a 29-year review. Pediatr Surg Int 22(12):987–990
Sapin E, Centonze A, Moog R et al (2006) Transanal coloanal anastomosis for Hirschsprung’s disease: comparison between endorectal and perirectal pull-through procedures. Eur J Pediatr Surg 16(5):312–317
El-Sawaf MI, Drongowski RA, Teitelbaum DH et al (2007) Are the long-term results of the transanal pull-through equal to those of the transabdominal pull-through? A comparison of the 2 approaches for Hirschsprung disease. J Pediatr Surg 42(1):41–47
Stensrud KJ, Emblem R, Bjornland K (2010) Functional outcome after operation for Hirschsprung disease—transanal vs. transabdominal approach. J Pediatr Surg 45(8):1640–1644
Kim AC, Langer JC, Pastor AC et al (2010) Endorectal pull-through for Hirschsprung’s disease-a multicenter, long-term comparison of results: transanal vs. transabdominal approach. J Pediatr Surg 45(6):1213–1220
Fichtner-Feigl S, Sailer M, Höcht B, Thiede A (2003) Development of a new scoring system for the evaluation of incontinence and constipation in children. Coloproctol 25(1):10–15
Teitelbaum DH, Coran AG (2008) Long-term results and quality of life after treatment of Hirschsprung’s disease and allied disorders. In: Holschneider AM, Puri P (eds) Hirschsprung’s disease and allied disorders, 3rd edn. Springer, Berlin, pp 387–396
Menezes M, Puri P (2005) Long-term clinical outcome in patients with Hirschsprung’s disease and associated Down’s syndrome. J Pediatr Surg 40(5):810–812
Quinn FM, Surana R, Puri P (1994) The influence of trisomy 21 on outcome in children with Hirschsprung’s disease. J Pediatr Surg 29(6):781–783
De La Torre L, Langer JC (2010) Transanal endorectal pull-through for Hirschsprung disease: technique, controversies, pearls, pitfalls, and an organized approach to the management of postoperative obstructive symptoms. Semin Pediatr Surg 19(2):96–106
Engum SA, Grosfeld JL (2004) Long-term results of treatment of Hirschsprung’s disease. Semin Pediatr Surg 13(4):273–285
Moore SW, Albertyn R, Cywes S (1996) Clinical outcome and long-term quality of life after surgical correction of Hirschsprung’s disease. J Pediatr Surg 31(11):1496–1502
Levitt MA, Martin CA, Pena A et al (2009) Hirschsprung’s disease and fecal incontinence: diagnostic and management strategies. J Pediatr Surg 44(1):271–277
Tannuri AC, Tannuri U, Romao RL (2009) Transanal endorectal pull-through in children with Hirschsprung’s disease—technical refinements and comparison of results with the Duhamel procedure. J Pediatr Surg 44(4):767–772
Van Leeuwen K, Geiger JD, Teitelbaum DH et al (2002) Stooling and manometric findings after primary pull-throughs in Hirschsprung’s disease: perineal versus abdominal approaches. J Pediatr Surg 37(9):1321–1325
Till H, Heinrich M, Schuster T (2006) Is the anorectal sphincter damaged during a transanal endorectal pull-through (TERPT) for Hirschsprung’s disease? A 3-dimensional, vector manometric investigation. Eur J Pediatr Surg 16(3):188–191
Zhang SC, Bai YZ, Wang WL et al (2005) Stooling patterns and colonic motility after transanal one-stage pull-through operation for Hirschsprung’s disease in children. J Pediatr Surg 40(11):1766–1772
Langer J, Caty M, de la Torre-Mondragon L et al (2007) IPEG colorectal panel. J Laparoendosc Adv Surg Tech A 17(1):77–100
Pena A, Elicevik M, Levitt MA (2007) Reoperations in Hirschsprung’s disease. J Pediatr Surg 42(6):1008–1013
Nasr A, Langer JC (2007) Evolution of the technique in the transanal pull-through for Hirschsprung’s disease: effect on outcome. J Pediatr Surg 42(1):36–39
Keshtgar AS, Ward HC, De Sousa NM et al (2003) Investigations for incontinence and constipation after surgery for Hirschsprung’s disease in children. Pediatr Surg Int 19(1–2):4–8
Catto-Smith AG, Coffey CM, Hutson JM et al (1995) Fecal incontinence after the surgical treatment of Hirschsprung disease. J Pediatr 127(6):954–957
Little DC, Snyder CL (2008) Early and late complications following operative repair of Hirschsprung’s disease. In: Holschneider AM, Puri P (eds) Hirschsprung’s disease and allied disorders, 3rd edn. Springer, Berlin, pp 375–385
Kleinhaus S, Boley SJ, Sieber WK et al (1979) Hirschsprung’s disease—a survey of the members of the Surgical Section of the American Academy of Pediatrics. J Pediatr Surg 14(5):588–597
Heikkinen M, Rintala RJ, Louhimo I (1995) Bowel function and quality of life in adult patients with operated Hirschsprung’s disease. Pediatr Surg Int 10(5):342–344
Catto-Smith AG, Trajanovska M, Taylor RG (2007) Long-term continence after surgery for Hirschsprung’s disease. J Gastroenterol Hepatol 22(12):2273–2282
Acknowledgments
The First author listed would like to thank the Edinburgh Surgical Sciences Qualification (ESSQ) team. This paper is an excerpt from the final project for the award of MSc in surgical sciences from the University of Edinburgh/Royal College of Surgeons Edinburgh.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aworanti, O.M., Mcdowell, D.T., Martin, I.M. et al. Comparative review of functional outcomes post surgery for Hirschsprung’s disease utilizing the paediatric incontinence and constipation scoring system. Pediatr Surg Int 28, 1071–1078 (2012). https://doi.org/10.1007/s00383-012-3170-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-012-3170-y