Abstract
The aim of this study was to analyse the long-term outcome after surgical correction of Hirschsprung’s disease using a standardised questionnaire designed specifically to address the long-term results, in correlation to the physical examination of each patient. The data was collected from the medical records of patients treated over a 15 year period (2000–2014). Sixty-two patients were treated, 33 using one-stage and 29 using multistage surgical procedures. Twenty-seven children took part in the whole study, which consisted of personal interview, completing the questionnaire and physical examination. The Duhamel-Martin and transanal endorectal pull through techniques were used. Statistical analysis was performed using STATISTICA 10. The statistical significance was set at p < 0.05. The Mann-Whitney’s test and the Spearman’s rank correlation coefficient were used. The most common side effect after surgical treatment was faecal incontinence (23 patients). There was no correlation between the method of the surgery and number of side effects. Postoperatively, there were significant correlations (p < 0.05) between the number of loose stools and the growth of these patients, 48% of the children were outside the normal centile (10–90) and 74% for weight, with consideration to their sex and age. This group of patients was below the 10th centile for weight and growth. There are significant deviations in the patients’ development after surgical treatment of Hirschsprung’s disease. The long-term results after surgical procedure were satisfactory for children and their parents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There are differing opinions about outcomes after surgical correction of Hirschsprung’s disease. In many publications, postoperative results of the surgical management are described as satisfactory [1,2,3,4,5,6,7,8,9,10,11,12]. In contrary, many studies report a higher than anticipated incidence of problems related to surgical treatment of Hirschsprung’s disease [13,14,15,16].
There are many factors which can influence the results of surgical treatment. One is the type of surgical method utilised. Since 1946, when Swenson and Bill first carried out successful surgery, many types of procedures have been described. There were several of them reported: Duhamel, Soave and Rehbein procedures [17]. In the early 1990s, Georgeson established a minimal access approach. It consists of a laparoscopic biopsy for identification of transition zone, laparoscopic preparation of the rectum and endorectal mucosal dissection. The anastomosis is performed after prolapsing and excising the rectum. Laparoscopic approaches have also been reported for the Duhamel and Swenson surgeries. In 1998, De la Torre-Mondragon and Ortega described the single-stage total transanal endorectal pull through (TEPT) [18].
Research findings and conclusions often vary across independent studies. The aim of this study was to analyse the overall long-term outcomes after surgical correction of Hirschsprung’s disease using a standardised questionnaire designed specifically to address the long-term effects of surgical treatment of Hirschsprung’s disease, in connection with physical examination of each patient. This study also evaluated the development of these patients.
Methods
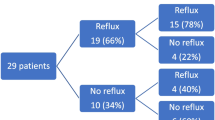
Data were collected based on the medical records review from 2000 till 2014 in the Department of Paediatric Surgery, Traumatology and Urology in Poznan. During 15 years, 62 patients were treated using one-stage and multistage surgery methods. There were 33 children treated using one-stage surgery and 29 using multistage method. Duhamel-Martin and TEPT techniques were used.
Final diagnosis of Hirschsprung’s disease was always confirmed by biopsy and histopathological examination in all children. All of the patients referred from other centres by the first diagnosis and colostomy were not included in the study. The choice of one-stage or multistage surgery was of surgeon’s decision based on the clinical status of the patient. During radical surgery the level of intestine’s resection was determined based on intraoperative histopathology examination.
There were three parts of the study: a personal interview with parents and patient, completing the standardised questionnaire and a physical examination.
The letters announcing control visits for patients with Hirschsprung’s disease with the standardised questionnaires were sent to all 62 patients. Of these, 10 were returned to sender. The questionnaires of 4 children were completed by parents and sent to the clinic without wishing to take part in the study. Twenty-seven children took part in the personal interview, submitted questionnaires and were fully examined. The other 21 patients did not respond to the letter.
The questionnaire also included questions about the actual weight and height (which were verified and referenced to standard values for sex and age contained in the percentile charts) [19].
The other questions analysed the demographic data, family history of diseases, evaluation of the pregnancy and the childbirth, other diseases and congenital anomalies of patient, age of first symptoms, age of diagnosis, type of performed diagnostic, type of performed surgery, presence of side effects after surgical correction, assessment of the stool using Bristol scale, type of treatment for the side effects, and also assessment of the nutritional status and general condition.
The Bristol stool scale is a medical aid designed to classify the form of human faeces into seven categories. Types 1 and 2 indicate constipation types 3 and 4 are the ideal stools, as they are easy to defecate while not containing excess liquid, and 5, 6 and 7 tending towards diarrhoea. In this study, diarrheas coexisting with symptoms of gastrointestinal infections were excluded from the statistical analysis. Details of the Bristol scale were included in Fig. 1.
The full clinical examination included palpation of the abdomen assessed with particular emphasis on the shape (i.e. distension), the tension and the painfulness. There was assessment of the tone of the anal sphincter, anal stenosis or anastomotic stricture, faecal retention, a faecal incontinence during Valsalva manoeuvre and faecal soiling.
Statistical analysis was performed using STATISTICA 10 (StatSoft Inc., Tulsa, USA). The statistical significance was set at p < 0.05. To examine the relationship between described variables, the Mann-Whitney’s test and the Spearman’s rank correlation coefficient were used.
In order to classify patients to the appropriate group, due to the presence of side effects after surgical treatment of Hirschsprung’s disease, the data mining method—classification and regression tree (CRT)—was used. Its construction included age of diagnosis and time after surgery until medical check-ups. CRT, exhaustive search for univariate splits method, was used to find divisions of predictor variable. The Gini measure was chosen as the measure of goodness of fit. The FACT (Fast Algorithm for Classification Trees)-style direct stopping was used as the stopping rule.
The study was conducted in accordance with a protocol presented to the Bioethical Commission of Poznan University of Medical Sciences (Decision No. 58/12).
Results
There were 33 children treated using one-stage surgery and 29 using multistage method. Thirty-one patients participated in the questionnaire survey, 27 in the whole study. Duhamel-Martin technique was used in 2 children treated in one-stage and in 7 patients operated in few stages. TEPT method was used in 19 children treated in one-stage and in 3 patients operated in few stages. The average age of patients taking part in the study was 8. They were aged between 3 and 17 years.
Using centile charts, in a wide range of norm (10–90 percentile), 74% of children were outside the norm for growth, and 48% for weight, taking into account sex and age (Fig. 2).
There were no correlations between abnormal weight or growth and method of the surgery found.
There were statistically significant dependences between the higher frequency of loose stools and lower body weight and less growth (Figs. 3 and 4).
Control studies showed the occurrence of side effects after treatment in 71% of children operated TEPT technique and in 80% patients treated using Duhamel-Martin surgery (Table 1).
During control studies anal stenosis or anastomotic stricture were not diagnosed.
There was no correlation between the method of the surgery and number of side effects after treatment.
There were also no correlations between the number of side effects, the type of stool, the frequency of defecation and the time after surgery. It was not found that frequency of loose stools decreases with increasing time after surgery. Also, there was no relationship between children’s nutritional status and all other analysed parameters.
Discussion
Since the first description in 1998, the TEPT has become extensively used [18]. It potentially obviates laparotomy or laparoscopy [20]. The Duhamel-Martin technique is performed using two approaches: abdominal and perineal. In the abdominal phase, intestine is identified and mobilised. The normally innervated gut is localised in created retrorectal space and pulled outside through the posterior rectal wall and anus. Then, an end-to-side and side-to-side anastomoses are made [21].
Taking into account the different ways of performing these two types of surgeries, the aim of this study was to analyse the overall long-term outcomes after surgical correction of Hirschsprung’s disease. Standardised questionnaires designed specifically to address the long-term effects after surgical treatment and physical examination were analysed.
In this study, 71% of children operated using TEPT technique and 80% patients treated using Duhamel-Martin surgery presented side effects after operation. Stringer et al. wrote that 60 to 70% of patients after surgery of Hirschsprung’s disease have continuing difficulties with constipation, soiling and abdominal pain. They reported that these problems appear to be independent of the operation, age at surgery or sex of the child [22].
A significant part of the analysed children demonstrated at the time of medical check-ups deficiency of the body growth (74%) and weight (48%). These results can be related to the publication of Moore, which confirms deviations not only in antropomorphic indices, but also in delayed developmental milestones [16].
A correlation between the method of the surgery and number of side effects was not found. Moore et al. described the increased incidence of complications in children treated using Duhamel or Swenson technique. The Duhamel surgery was associated with an increased frequency of constipation. The Swenson procedure was connected with a higher incidence of micturition disturbance, abdominal distension and cuff stricture [16].
A lot of publications describe occurrence of loose stools like a side effect after surgical treatment. One example is publication of Langer et al. [23]. However, a publication, which summed up the influence of frequency of loose stools on the growth and weight of the patients, was not found. Figures 3 and 4 show correlation between increased frequency of the loose stools and decreased growth and weight in children after surgical treatment.
In this study, the frequency of side effects after surgical treatment was comparable for both methods. Faecal incontinence was the most common complication for these methods and involved 23 children (Table 1). A similar situation was described in publication of Catto-Smith et al. [24]. Their study again confirmed the high prevalence of long-term faecal incontinence after the surgical treatment of Hirschsprung’s disease. In this report, 39% operated children presented soiling accidents that occurred “often” or “always”. At least a couple of publications confirmed this observation [22, 24, 25]. Importantly, it was found the evidence of a reduction in faecal incontinence with age [24]. It was not confirmed in our study. No correlation like this was detected.
The second most common side effect was faecal retention during rectal examination. It was observed in 7 children treated using TEPT technique and in 4 patients operated using Duhamel-Martin method. Stringer et al. described faecal retention in 10% of children treated surgically [22].
Abdominal pain was observed in 32% of children treated surgically. Catto-Smith et al. reported that this complication occurred in 53% patients, who took part in his study [24].
In summary, this study proved that frequency of loose stools has influence on the weight and growth of the children and does not decrease with longer time after surgery. A significant part of the patients treated surgically because of Hirschsprung’s disease is outside of the norm (below the 10th centile) for the growth and weight, taking into account their sex and age.
This research shows that faecal incontinence is the most common postoperative complication. The frequency of all side effects after surgical treatment was comparable for both methods. The analysis of the described parameters shows that the long-term results of the transanal pull-through and transabdominal pull-through are equally satisfying for children and their parents. The final evaluation of the effects of surgical treatment requires long-term analysis of a large group of patients.
References
Swenson O, Sherman JO, Fisher JH (1973) Diagnosis of congenital megacolon: an analysis of 501 cases. J Pediatr Surg 8:587–594
Ehrenpreiss TH (1970) Hirschsprung’s disease. Year Book Publishers, Chicago, pp 58–60
Puri P, Nixon HH (1977) Long term results of Swenson’s operation for Hirschsprung’s disease. Prog Pediatr Surg 10:87–96
Kleinhaus S, Boley SJ, Sherman M et al (1979) Hirschsprung’s disease: a survey of the Surgical Section of the American Academy for Pediatrics. J Pediatr Surg 16:588–597
Holschneider AM (1982) Hirschsprung’s disease. Thieme-Stratton, Stuttgart, pp 237–240
Soave F (1985) Endorectal pullthrough: 20 years experience. J Pediatr Surg 20:568–579
Ikeda K, Goto S (1984) Diagnosis and treatment of Hirschsprung’s disease in Japan. An analysis of 1628 patients. Ann Surg 199:400–405
Nixon HH (1985) Hirschsprung’s disease: progress in management and diagnostics. World J Surg 9:189–202
Foster P, Cowan G, Wrenn E (1990) Twenty-five years experience with Hirschsprung’s disease. J Pediatr Surg 25:531–534
Rescorla FJ, Morrison AM, Engles D et al (1992) Hirschsprung’s disease. Evaluation of mortality and long term function in 260 cases. Arch Surg 127:934–942
Klein MD, Philippart AI (1993) Hirschsprung’s disease: three decades experience at a single institution. J Pediatr Surg 28:1291–1294
Shono K, Hutson JM (1994) The treatment of postoperative complications of Hirschsprung’s disease—a 10 year experience. Pediatr Surg Int 9:362–365
Clausen EG, Davies OG (1963) Early and late complications of the Swenson pull-through operation. Am J Surg:372–380
Kluck P, Ten Kate FJW, van der Kamp AWM et al (1986) Pathological explanation for postoperative obstipation in Hirschsprung’s disease revealed by monoclonal antibody staining. Am J Clin Path 86:490–492
Molenaar J, Tibboel D, van der Kamp AWM et al (1989) Diagnosis of innervation-related motility disorders of the gut. Prog Pediatr Surg 24:173–185
Moore SW, Albertyn R, Cywes S (1996) Clinical outcome and long-term quality of life after surgical correction of Hirschsprung’s disease. J Pediatr Surg 31:1496–1502
Dahal GR, Wang JX, Guo LH et al (2011) Long-term outcome of children after single-stage transanal endorectal pull-through for Hirschsprung’s disease. World J Pediatr 7:65–69
De La Torre L, Langer JC (2010) Transanal endorectal pull-through for Hirschsprung disease: technique, controversies, pearls, pitfalls, and an organized approach to the management of postoperative obstructive symptoms. Semin Pediatr Surg 19:96–106
Niedźwiecka Z, Palczewska I (1999) Siatka centylowa masy i długości ciała. Instytut Matki i Dziecka, Warszawa
El-Sawaf MI, Drongowski RA, Chamberlain JN et al (2007) Are the long-term results of the transanal pull-through equal to those of the transabdominal pull-through? A comparison of the 2 approaches for Hirschsprung disease. Semin Pediatr Surg 42:41–47
Sosnowska P, Blaszczyński M (2016) A 15-year experience with the one-stage surgery for treatment of Hirschsprung’s disease in newborns, infants, and young children. Indian J Surg 77:1109–1114
Stringer MD, Oldham KT, Mouriquand PDE et al (2006) Pediatric surgery and urology. Long-term outcomes, 2nd edn. Cambridge University Press, Cambrige, p 425
Langer JC, Durrant AC, De La Torre L et al (2003) One-stage transanal soave pull-through for Hirschsprung disease. A multicenter experience with 141 children. Ann Surg 569–576
Catto-Smith AG, Trajanovska M, Taylor R (2007) Long-term continence after surgery for Hirschsprung’s disease. J Gastroenterol Hepatol 22:2273–2282
Catto-Smith AG, Coffey CM, Nolan TM (1995) Fecal incontinence after the surgical treatment of Hirschsprung disease. J Pediatr 127:954–957
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Funding
This study was not founded by any institution.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Sosnowska, P., Błaszczyński, M., Moryciński, S. et al. Analysis of Outcomes After Surgical Correction for Hirschsprung’s Disease: Are the Long-Term Results of the Transanal and Transabdominal Pull-Through Operations Equally Satisfying for Children and Their Parents?. Indian J Surg 80, 580–585 (2018). https://doi.org/10.1007/s12262-017-1671-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-017-1671-6