Abstract
Introduction
VACTERL is a rare, non-random association comprising at least three major component features defined by the acronym, and including Vertebral anomalies, Anorectal malformations, Cardiac defects, Tracheo-oEsophageal fistula with or without oesophageal atresia (TOF/OA), Renal abnormalities and Limb anomalies. The aim of this study was to compare the post-operative outcomes following surgical correction of TOF/OA in infants with VACTERL and isolated TOF/OA.
Methods
A retrospective case–control study comparing infants with VACTERL (case group) versus infants with isolated TOF/OA (control group) that underwent surgical correction of TOF/OA at our centre between January 2006 and December 2011. Patient demographics, types of anomalies, operative techniques and post-operative outcomes were collected using inpatient and outpatient records.
Results
We identified 30 consecutive infants with TOF/OA. Five infants had VACTERL (17 %) and 15 infants had isolated TOF/OA (50 %). There was no significant difference in the gestational age (P = 0.79), birth weight (P = 0.69) or operative repair (P = 0.14) between groups. Overall, surgical correction of TOF/OA led to satisfactory morbidity. Infants with VACTERL were not at higher risk of post-operative complications, such as oesophageal stricture (P = 0.17) or gastro-oesophageal reflux (P = 1.0), compared to infants with isolated TOF/OA.
Conclusions
VACTERL association does not increase the risk of post-operative complications following TOF/OA repair.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
VACTERL is a rare, non-random association of complex congenital abnormalities [1, 2]. It has an estimated prevalence of between 1 in 10,000 and 1 in 40,000 infants [3]. The phenotypic characteristics required for the diagnosis of VACTERL have been extensively debated since its original description, but most clinicians agree that at least three major component features (MCFs) are required. These include Vertebral anomalies, Anorectal malformations, Cardiac defects, Tracheo-oEsophageal fistula with or without oesophageal atresia (TOF/OA), Renal abnormalities and Limb anomalies. The aim of this study was to compare the post-operative outcomes following surgical correction of TOF/OA in infants with VACTERL and isolated TOF/OA.
Methods
Our study was approved by the ethical review board of the John Radcliffe Hospital, Oxford. The hospital database was searched to identify all infants with TOF/OA between January 2006 and December 2011. A diagnosis of VACTERL was made if an infant possessed at least three MCFs, and had no clinical signs or chromosomal abnormalities consistent with overlapping syndromes. Congenital defects that are recognised features of prematurity, such as patent ductus arteriosus (PDA), patent foramen ovale and cryptorchidism, were not included as MCFs. Infants with hydrocephalus, i.e. VACTERL-H syndrome were also excluded.
Patient demographics, types of anomalies, operative techniques and post-operative outcomes were collected using inpatient and outpatient records. Categorical data are described by frequency and percentage, and continuous data are described as median (range) or mean ± SD. To determine significant differences between groups, a Fisher exact test was used for categorical variables and a Mann–Whitney U test was used for continuous variables. A P value ≤ 0.05 was considered as significant.
Results
Population
We identified 30 consecutive infants with TOF/OA between January 2006 and December 2011. Five infants had VACTERL (17 %) and 15 infants had isolated TOF/OA (50 %). The remaining infants had CHARGE syndrome (n = 2), Trisomy 18 (n = 2), Treacher-Collins syndrome (n = 1), Townes-Brocks syndrome (n = 1), or, other anomalies that were not consistent with an identifiable syndrome (n = 4). The spectrum of MCFs in infants with VACTERL is outlined in Table 1.
Perinatal morbidity in infants with VACTERL
Antenatal complications included polyhydramnios (n = 5), maternal insulin-dependent diabetes mellitus (n = 1), intrauterine growth retardation (n = 1) and twin reversed arterial perfusion syndrome (n = 1). There was no parental consanguinity [4].
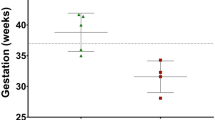
There was no significant difference between the gestational age (P = 0.79) or birth weight (P = 0.69) in infants with VACTERL and isolated TOF/OA (see Table 2). Genetic analysis was performed on all infants with VACTERL and results were negative [5].
VACTERL including TOF/OA
Five infants (2 males) had VACTERL. Four infants were diagnosed antenatally when polyhydramnios and a small/absent fetal stomach bubble were evident on fetal ultrasound scans. Two infants had OA with proximal TOF (40 %) and three infants had OA with distal TOF (60 %). Two infants had long-gap OA (defined as a distance of four or more vertebral bodies whilst under tension [6]). Three infants underwent thoracotomy, fistula ligation and primary OA repair on day 1 of life. One infant with long-gap OA underwent thoracotomy, fistula ligation and gastrostomy. Delayed repair under anastomotic tension was performed 8 weeks later. The second infant with long-gap OA had Fallot-type double outlet right ventricle (DORV), and left hypoplastic lung, pulmonary artery and pulmonary vein. On day 1 of life this infant underwent thoracotomy, fistula ligation and gastrostomy, but primary repair was considered inappropriate due to intra-operative respiratory distress. Cervical oesophagostomy was performed 11 weeks later, although the infant died from heart failure before oesophageal replacement surgery was performed.
Post-operative morbidity included oesophageal stricture (n = 4), gastro-oesophageal reflux (GOR; n = 2), tracheomalacia (n = 2) and anastomotic leak (n = 1). No infant developed fistula recurrence. A contrast study was used to diagnose oesophageal stricture in symptomatic infants. Four infants underwent 2–5 endoscopic balloon dilatations for stricture formation. Anti-reflux surgery was performed in one infant. In comparison to infants with isolated TOF/OA, infants with VACTERL were not at higher risk of post-operative complications (see Table 2).
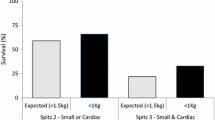
A single infant (birth weight of 2,780 grams) with VACTERL died of heart failure secondary to pulmonary hypertension and complex congenital heart disease (Fallot-type DORV). They underwent total cardiac repair at 4 months of age, but died 2 months later. There was no difference between the overall survival of infants with VACTERL (80 %) and isolated TOF/OA (93 %) (see Table 2).
The median follow-up was 2 years (range 1–6 years).
Discussion
Early observational trials outlining the surgical management of TOF/OA in infants with VACTERL used a temporary gastrostomy prior to definitive repair [7–9]. Since then, corrective surgery of TOF/OA has developed to favour primary repair; often within 1–2 days of birth. In our study, all infants with short-gap OA underwent primary repair, and only those with long-gap OA or intra-operative complications required temporary gastrostomy.
Gastro-oesophageal reflux and oesophageal stricture are the most common post-operative complications associated with OA repair occurring in approximately 40 % and 30 % of cases, respectively [10]. Risk factors for oesophageal stricture include anastomotic leak, GOR and anastomotic tension [6, 10]. In our study, infants with VACTERL were not at statistically higher risk of anastomotic leak, GOR or oesophageal stricture. In addition, there was no difference in the incidence of long-gap OA requiring anastomotic tension. Our findings contrast those reported in a recent publication, in which VACTERL was identified as a significant risk factor (univariate analysis: P = 0.013) for oesophageal stricture following OA repair in a larger retrospective cohort (n = 62) [11].
Our study has two major limitations that should be considered when interpreting the findings. First, this is a retrospective study and prone to the disadvantages associated with such trial design. Second, our sample size is small and underpowered. Nevertheless, it is well recognised that the prevalence of VACTERL is extremely low; estimated between 1 in 10,000 and 1 in 40,000 infants [3]. Registry data also shows that TOF/OA is not a universally expressed phenotypic characteristic in these infants; occurring in around 50–80 % of cases [12–14]. Furthermore, unlike other studies [15, 16], we have only included infants with at least three MCFs of VACTERL and a negative genetic screen, as well as excluding MCFs that are consistent with prematurity (e.g. PDA). These factors mean that although the size of the study group is small, we are confident that these infants were appropriately diagnosed [5].
In summary, we have outlined the surgical management of TOF/OA in infants with VACTERL at our institution over a 6-year period. We can conclude that VACTERL is not associated with a higher risk of surgical morbidity or mortality compared to isolated TOF/OA.
References
Quan L, Smith DW (1973) The VATER association. Vertebral defects, anal atresia, T-E fistula with esophageal atresia, radial and renal dysplasia: a spectrum of associated defects. J Pediatr 82:104–107
Temtamy SA, Miller JD (1974) Extending the scope of the VATER association: definition of the VATER syndrome. J Pediatr 85:345–349
Solomon BD (2011) VACTERL/VATER association. Orphanet J Rare Dis 6:56
Hilger A, Schramm C, Draaken M et al (2012) Familial occurrence of the VATER/VACTERL association. Pediatr Surg Int 28:725–729
Shaw-Smith C (2006) Oesophageal atresia, tracheo-oesophageal fistula, and the VACTERL association: review of genetics and epidemiology. J Med Genet 43:545–554
Holland AJ, Fitzgerald DA (2010) Oesophageal atresia and tracheo-oesophageal fistula: current management strategies and complications. Paediatr Respir Rev 11:100–106
Katz S, Shapiro Y, Mizrahi S et al (1987) Surgical treatment of infants with esophageal atresia and VATER association. Isr J Med Sci 23:209–212
Muraji T, Mahour GH (1984) Surgical problems in patients with VATER-associated anomalies. J Pediatr Surg 19:550–554
Weber TR, Smith W, Grosfeld JL (1980) Surgical experience in infants with the VATER association. J Pediatr Surg 15:849–854
Spitz L (2007) Oesophageal atresia. Orphanet J Rare Dis 2:24
Serhal L, Gottrand F, Sfeir R et al (2010) Anastomotic stricture after surgical repair of esophageal atresia: frequency, risk factors, and efficacy of esophageal bougie dilatations. J Pediatr Surg 45:1459–1462
Botto LD, Khoury MJ, Mastroiacovo P et al (1997) The spectrum of congenital anomalies of the VATER association: an international study. Am J Med Genet 71:8–15
Kallen K, Mastroiacovo P, Castilla EE et al (2001) VATER non-random association of congenital malformations: study based on data from four malformation registers. Am J Med Genet 101:26–32
Rittler M, Paz JE, Castilla EE (1996) VACTERL association, epidemiologic definition and delineation. Am J Med Genet 63:529–536
Keckler SJ, St Peter SD, Valusek PA et al (2007) VACTERL anomalies in patients with esophageal atresia: an updated delineation of the spectrum and review of the literature. Pediatr Surg Int 23:309–313
Seo J, Kim do Y, Kim AR et al (2010) An 18-year experience of tracheoesophageal fistula and esophageal atresia. Korean J Pediatr 53:705–710
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morgan, R.D., O’Callaghan, J.M., Wagener, S. et al. Surgical correction of tracheo-oesophageal fistula and oesophageal atresia in infants with VACTERL association: a retrospective case–control study. Pediatr Surg Int 28, 967–970 (2012). https://doi.org/10.1007/s00383-012-3165-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-012-3165-8