Abstract
Hirschsprung’s disease (HSCR) is a developmental disorder characterized by the absence of ganglion cells in the lower digestive tract. Aganglionosis is attributed to a disorder of the enteric nervous system (ENS) whereby ganglion cells fail to innervate the lower gastrointestinal tract during embryonic development. HSCR is a complex disease that results from the interaction of several genes and manifests with low, sex-dependent penetrance and variability in the length of the aganglionic segment. The genetic complexity observed in HSCR can be conceptually understood in light of the molecular and cellular events that take place during the ENS development. DNA alterations in any of the genes involved in the ENS development may interfere with the colonization process, and represent a primary etiology for HSCR. This review will focus on the genes known to be involved in HSCR pathology, how they interact, and on how technology advances are being employed to uncover the pathological processes underlying this disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Understanding how genes and other DNA sequences function together and interact with proteins and environmental factors is paramount to the discovery of the pathways involved in normal processes and in disease pathogenesis. In this respect, the study of the molecular basis of Hirschsprung’s disease (HSCR) has made a marked contribution to the understanding of complex diseases. Complex diseases result from the interaction of two or more genes and/or gene–environment interactions [1] and therefore, have no identifiable pattern of inheritance.
Hirschsprung’s disease (HSCR) is a developmental disorder characterized by the absence of ganglion cells in the lower digestive tract. Aganglionosis is attributed to a disorder of the enteric nervous system (ENS) whereby ganglion cells fail to innervate the lower gastrointestinal tract during embryonic development. There is a significant racial variation in the incidence of the disease, and it is most often found among Asians (2.8 per 10,000 life births) [2]. HSCR has a complex pattern of inheritance and manifests with low, sex-dependent penetrance (frequency of mutation carriers who develop disease as opposed to mutation carriers who remain healthy) and variability in the length of the aganglionic segment. HSCR patients are classified according to the length of the aganglionic segment into: short-segment HSCR (SS-HSCR) (~80% of HSCR cases) and long segment HSCR (LS-HSCR) (~20% of HSCR cases). The rectosigmoid region acts as the boundary between LS-HSCR and SS-HSCR. LS-HSCR is defined as aganglionic segment extending to or beyond the proximal sigmoid colon, whereas, the remaining cases are grouped as SS-HSCR.
The HSCR most commonly presents sporadically although it can be familial (up to 20% of the cases) and is frequently associated with many other neurocristopathies and chromosome abnormalities [3, 4].
The genetic complexity observed in HSCR can be conceptually understood in light of the molecular and cellular events that take place during the ENS development in the embryonic stage. The ganglion cells of the fully developed ENS are derived from vagal neural crest cells (NCCs) of the neural tube [5]. During the colonization process, the NCCs have to adapt to a constantly changing intestinal environment that strongly influences their differentiation into enteric neurons [6]. The entire process is regulated by specific molecular signals from both within the neural crest and intestinal environment [7], and the success of the colonization of the gut depends on the synchronization and balance of the signaling network implicated. DNA alterations in any of the genes codifying for the signaling molecules may interfere with the colonization process, and consequently represent a primary etiology for HSCR. The HSCR phenotype may therefore result from (i) single severe DNA alterations (mutations) in a major gene encoding a crucial molecule; (ii) the summation of the effects of a series of less severe mutations in several genes; (iii) the former and the later combined. The existence of non-clinically affected individuals carrying mutations in major genes invokes a compensatory effect by other genes and reinforces the oligogenic nature of the disease. HSCR has become a model for oligogenic and polygenic disorders in which the phenotypes and mode of transmission result from interactions between different genes.
The genetic etiology of Hirschsprung’s disease
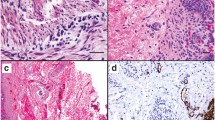
In 1886, Danish pediatrician Harald Hirschsprung (1830–1916) described the disease as a cause of constipation in early infancy due to congenital dilatation of the colon. But it was not till the 1940s, when histological studies revealed absence of intramural ganglion cells of the myenteric and submucosa plexuses downstream the dilated colon (megacolon), that the primary pathology of the disease was discovered [8].
The development of a pull-through surgical procedure by Swenson and Bill in 1948 made a major contribution to our understanding of the disease [9]. This innovative surgical technique enabled a far higher survival rate among patients, which created the conditions for the discovery of the familial transmission of the disease and the determination of its genetic nature. Additional evidence for a role of genetic factors in the pathology of HSCR was indicated by (i) an increased risk of recurrence for sibs of affected individuals compared with the population at large; (ii) an unbalanced sex-ratio; (iii) the association of HSCR with other genetic diseases, including malformation syndromes and chromosomal anomalies; and (iv) the existence of several animal models of colonic aganglionosis showing specific Mendelian modes of inheritance.
In the late 1980s, the locus for multiple endocrine neoplasia (MEN) was assigned to chromosome 10q11.2 [10, 11]. The same locus was also identified as the cause of papillary thyroid carcinoma (PTC) [12–14] and familiar medullary thyroid carcinoma (FMTC) [15]. The co-occurrence of HSCR with multiple endocrine neoplasia type 2 (MEN2) together with the observation of a deletion comprising the MEN2 locus in some HSCR patients [16, 17], prompted the search for a HSCR gene in that chromosomal region. Linkage analysis using chromosome 10 markers in HSCR families revealed a HSCR locus in the pericentromeric region of chromosome 10 [18, 19]. The observation of a HSCR-phenotype in mice with disrupted Ret gene [20] and the detection of RET rare deleterious DNA alterations (“mutations”) in HSCR families [21, 22] lead to the recognition of RET as the main gene implicated in HSCR, almost a century after Harald Hirschsprung first described the disease.
The fact that not all HSCR patients bore mutations in RET, implied that mutations in other genes accounted for the rest of the HSCR patients or/and that mutations occurred in regions of the gene which had not been investigated, namely regulatory non-coding regions. Subsequent studies lead to the identification of other genes in which DNA alterations or mutations lead to the HSCR phenotype. To date, mutations in the coding regions of nine different genes (RET, GDNF, NRTN, PHOX2B, EDNRB, EDN3, ECE1, SOX10, ZFHX1B, KIAA1279, and NRG1; Garcia-Barceló and Tam et al. unpublished data) [8, 23] have been detected in individuals affected with either isolated or syndromic HSCR (Table 1). Most of these genes encode protein members of important inter-related signaling pathways that are critical for the development of enteric ganglia: the GDNF/RET receptor tyrosine kinase, the endothelin type B receptor, and the SOX10-mediated transcription. RET is, however, the major gene involved in HSCR, and the proper expression of the RET protein expression is critical for the normal development of the ENS [24–27]. There is evidence that the manifestation of the HSCR phenotype may result from the interaction and/or accumulation of DNA variants in genes of these signaling pathways as illustrated by the identification of patients bearing mutations in RET in combination with mutations in other genes namely GDNF, Neurturin (NTN), or EDNRB [28] (see below).
Common features to the mutations found in the HSCR genes are low and sex-dependent penetrance and variable expression of the HSCR phenotype for a given mutation. These characteristics are consistent with the expression of a HSCR gene subject to modification by other loci [29, 30], perhaps as a result of cross-talk between signaling pathways (see below).
RET receptor tyrosine kinase pathway
The RET protein, functions as a receptor for the Glial cell line-Derived Neurotrophic Factor (GDNF) family. Receptor–ligand interactions are mediated by RET co-receptors (GDNF-Family Receptors-α; GFRα) [31–33]. Activation of the RET receptor by these neurotrophic factors is essential for the migration and differentiation of NCCs into enteric neurons [20, 34, 35]. The correct development of the ENS therefore depends on the ability of these neurotrophic factors to activate RET, on the ability of the RET receptor to transduce the signal, and on the competence of the intracellular machinery to elaborate a response (Figs. 1 and 2).
Schematic drawing showing the RET gene and the RET protein receptor (adapted from [1]) and its localization on the neural crest cells. Exons of RET gene are indicated with numbered boxes and doted lines indicate the domains of the protein they encode. Different domains of RET receptor are indicated with cylinders. The extracellular part of RET contains cadherin domains (CAD) and the intracellular part of RET contains two tyrosine kinase domains (TK). TMD, transmembrane domain. In brackets, amino-acid residues
Schematic representation of the network of interactions that govern the development of the enteric nervous system (adapted from [1]). Expression of the RET gene (regulated by transcription factors) leads to the formation of the RET protein which functions as a receptor for the Glial cell line-Derived Neurotrophic Factor family (GFL) through co-receptors (GFRA). Activation of the RET receptor by these signaling molecules of the gut environment activates the intracellular machinery necessary for the migration, proliferation, and differentiation of neural crest cells into enteric neurons. Similarly, the EDNRB receptor is activated by EDN3 and initiates a series of events that will also regulate the development of the enteric nervous system in conjunction with the RET pathway. The Prok-1 and NRG1 pathways, thought to be involved in the ENS development, are also represented. Double head arrows indicate interrelation between pathways. Transcription factors involved in RET regulation are pictured in the nucleus. Question marks represent yet unidentified molecule members of the network (see section “Modifying genes and interaction between signaling pathways” in the text)
RET proto-oncogene and HSCR
The RET, also known as RET proto-oncogene, is composed of 21 exons that encode the RET receptor tyrosine kinase protein, a cell-surface molecule that transduces signals. Germline mutations in RET are responsible for four unrelated disorders in humans, HSCR, multiple endocrine neoplasia; type IIB (MEN2B), multiple endocrine neoplasia; type IIA (MEN2A), and medullary thyroid carcinoma (MTC) [36]. In PTC, somatic RET rearrangements are the most commonly detected genetic alterations. No germline mutations are found in PTC patients.
The RET is a single-pass membrane protein with two main domains: extracellular (EC) and intracellular (IC).
Ligand and co-receptor complexes interact with the EC domain of two RET molecules inducing their interaction with various intracellular signaling proteins [37]. Activating mutations in the RET gene cause MTC, MEN2A, and MEN2B, whereas inactivating mutations lead to HSCR [38]. A large number of RET mutations have been reported in HSCR patients. In general, RET gene mutations affecting the RET EC domain alter the folding of the protein impairing its maturation [39, 40]. RET mutations affecting the RET IC interfere with the binding to intracellular signaling proteins [40–42]. Mutations in any intron/exon boundary affecting the splicing consensus sequences can alter mRNA processing. Remarkably, silent mutations (i.e., the mutation does not result in an amino-acid change in the protein) in any of the RET exons can also affect mRNA processing [28]. Unlike in MEN 2, RET mutations causing HSCR are, with a very few exceptions [29], scattered throughout the gene, affecting indiscriminately any part of the RET protein. However, many RET mutations have not been functionally tested and it is very difficult to discern between truly deleterious substitutions and non-deleterious ones. A recent study based on the alignment of the human RET protein with 12 orthologous sequences provides an insight on the prediction of the effect of the RET mutations [43].
Mutations in the coding regions of RET and other HSCR genes (see below) only account for over 50% of the familial cases, and between 7% and 35% of the sporadic cases [44–59]. Intriguingly, genetic-linkage analyses in HSCR families keep implicating the 10q11 chromosomal region (RET locus) even though no RET coding regions can be found [29, 30]. This, besides confirming the central role of RET in HSCR, also indicates that mutations in non-coding (regulatory) regions RET remains to be found. Mutations in regulatory regions can alter the DNA binding sites of transcriptional regulators and reduce or abolish the expression of RET.
In addition to RET mutations, a possible role in HSCR has been attributed to several single nucleotide polymorphisms (SNPs; variations in the DNA present in >1% of the population) of the RET gene since they have been found associated with the disease (the frequency of the DNA variation varies significantly between patients and controls) [60–63], indicating that may indeed play a role, although subtle, in the disease. The current data indicates that these RET-SNPs could act as modifiers by modulating the penetrance of mutations in other HSCR genes and possibly of those mutations in the RET gene itself [64–68]. It has been shown that HSCR-associated RET-SNPs in the promoter region [69–71] and in intron 1 [72–74] quantitatively affect the expression RET. In particular, the RET promoter SNPs associated with HSCR disrupt the binding site of the transcription factor NKX2.1 (previously TTF-1; thyroid transcription factor 1).
It is worth noting that the overall frequencies of the HSCR-associated RET-SNPs and haplotypes are significantly higher in Chinese, not only in patients but also in the general population [63, 74], possibly explaining the higher incidence of HSCR in Asians when compared to Caucasians [2].
GDNF-family ligands and their receptors (GDNF-family receptors-α; GFRα)
The relevance of RET signaling pathway in the ENS development and the phenotypic similarities between Ret, Gdnf, and Gfrα-1 knock-out mice [20, 75–77], prompted an extensive mutation screening of the genes encoding the GDNF family of ligands—GDNF, neurturin (NTN), artemin (ARTN), and persepin (PSPN)—and of the genes encoding their co-receptors (GFR-α1–4) and adaptors. However, mutations in those genes have been identified in a very small number of patients and generally co-segregate with mutations in RET [78–82]. Screening of patients affected with idiopathic slow transit constipation and megacolon revealed no mutations associated with the phenotype [83]. Also, none of the of mutations identified in the GDNF gene is likely “per se” to cause HSCR, although it is thought they can contribute to disease via interaction with other susceptibility loci [33, 84–86]. Surprisingly, RET is virtually the only target of HSCR mutations in the RET signaling pathway. It is possible that homozygous mutations in the GDNF family of ligands were lethal, and that these ligands, particularly GDNF, may have other functions not mediated by RET, and therefore come under selective pressure against mutations.
HSCR genes involved in the transcriptional regulation of RET
Because of the key role played by RET in HSCR, mutations in genes known to be involved in the regulation of RET are likely to give rise to phenotypes involving aganglionosis. Not all the genes involved in the regulation process are known and the precise mechanisms of regulation remain unclear. Thus, further investigation on the molecules involved in RET regulation is likely to shed more light to the mechanisms underlying HSCR. In these respect, several RET regulators have been scrutinized.
SOX10
The SOX10 gene encodes a transcriptional regulator, the expression of which is essential for the development of cells in the NCC lineage, including melanocites and enteric neurons. During the development of the ENS, the SOX10 protein physically interacts and cooperates with another transcriptional regulator (PAX3) to activate transcription of RET [35, 87, 88]. Importantly, Sox10 also interacts with Ednrb in mice [89, 90].
The significance of the SOX10 gene in HSCR was revealed through the study of a mouse model of HSCR (Dom) fortuitously generated at the Jackson Laboratory [91]. The molecular defect in Dom mice was a mutation in the Sox10 gene [92–95]. Heterozygous Dom mice presented with distal colonic aganglionosis and localized hypomelanosis of the skin and hair (features similar to those in Waardenburg’s syndrome), which indicated that neural crest-derived melanocytes and enteric neurons were affected in Sox10 mutants. Dom homozygous mice were embryonic lethal.
In humans, heterozygous SOX10 mutations have been identified in patients with Waardenburg-Shah syndrome (WS4; HSCR type 2). Patients with WS4 display a combination of the features of Waardenburg syndrome (wide bridge of the nose, pigmentary abnormalities, and cochlear deafness) and HSCR [92, 96–102]. SOX10 mutations also lead to Yemenite deaf-blind hypopigmentation syndrome and other myelin deficiencies [103]. To date, no SOX10 mutations have been found in patients presenting aganglionosis as an isolated trait. SOX10 is therefore unlikely to be major gene in isolated HSCR. Interestingly, and despite the absence of genetic mutations, abnormal SOX10 gene expression can be observed in aganglionic intestine of isolated HSCR patients [102, 104].
PHOX2B
The paired mesoderm homeobox 2b gene (PHOX2) encodes a transcription factor which is involved in the development of several noradrenergic neuron populations. In mice homozygous disruption of the Phox2b gene results in absence of enteric ganglia, a feature reminiscent of HSCR. Furthermore, there is no Ret expression in Phox2b mutant embryos indicating that regulation of Ret by Phox2b could account for the failure of the ENS to develop [105, 106]. All these observations make the PHOX2B a candidate gene for HSCR. Interestingly, a chromosomal alteration involving the deletion of the PHOX2B locus has been described in a patient with syndromic HSCR (developmental delay, severe hypotonia, facial dysmorphism, and short-segment aganglionosis) [107]. This suggests that PHOX2B haploinsufficiency may predispose to HSCR. A SNP of the PHOX2B gene has been found to be associated with HSCR and importantly, the interaction between PHOX2B and RET HSCR-associated SNPs increases susceptibility to HSCR [108, 109].
PHOX2B represents the first gene for which germline mutations predispose to neuroblastoma [110–112] and is the major locus for congenital central hypoventilation syndrome (CCHS, Ondine’s curse) [113, 114]. In particular, 25–30% of the CCHS patients are affected with aganglionosis (Haddad syndrome) [115]. Intriguingly, both neuroblastoma and CCHS are frequently associated with HSCR [8, 116, 117]. Taken together these data support the contribution of PHOX2B to HSCR.
HOXB5
Recently, using transgenic mouse technology, it has been shown that the transcription factor Hoxb5 may contribute to HSCR by interfering with the regulation of the Ret gene. A fraction of Hoxb5 mutant mice presented with reduction of ganglia (hypoganglionosis) and slow peristalsis and Ret expression was markedly reduced or absent. In addition, HOXB5 SNPs were found associated to HSCR in Chinese patients. All these data suggest that DNA alterations in Hoxb5 contribute to the etiology of HSCR [118, 119].
As all HOX genes have a major role in gut development (the enteric Hox code), the implications of alterations in other gene members of the human HOX clusters was also investigated in Chinese HSCR patients. Genetic interaction was found among SNPs in two HOX loci (5′-HOXA13 and 3′UTR-HOXB7) and the most HSCR-associated RET-SNP, suggesting that the interacting HOX loci may affect the penetrance of the RET-risk locus [120].
NKX2.1
It was shown later that RET transcription was decreased due to alteration of the NKX2-1 transcription factor binding site by two HSCR-associated RET promoter SNPs (see above), the NKX2-1 gene was investigated for mutations in HSCR patients. Direct sequencing of 188 Chinese and 70 Caucasian patients revealed the presence of a Met3Leu mutation in two Caucasian patients. This mutation reduced the activity of the RET promoter and it is thought to contribute to HSCR by affecting the RET expression through defective interactions with other transcription factors [71, 121].
Endothelin type B receptor pathway
The endothelins are a family of three signaling peptides (EDN1, EDN2, and EDN3) that can act on two subtypes of G protein-coupled receptors, termed endothelin-A and endothelin-B receptors (EDNRA and EDNRB) (Fig. 2). The endothelins are synthesized as much larger proteins which are cleaved by the endothelin converting enzyme (ECE-1) to produce an active peptide. The human genes coding for these proteins are EDN1, EDN2, EDN3, EDNRA, and EDNRB, respectively.
The involvement of the endothelin type B receptor pathway in the pathology of HSCR was demonstrated when a targeted disruption of the mouse endothelin-B receptor gene (Ednrb) resulted in an autosomal recessive phenotype with aganglionic megacolon and white spotting of the coat [122]. A targeted disruption of the mouse endothelin-3 ligand (Edn3) gene produced a similar recessive phenotype of megacolon and white coat spotting [123]. These data indicated an essential role for the members of the EDNRB pathway in the development of two neural crest-derived cell lineages, enteric neurons and epidermal melanocytes. EDNRB signaling not only regulates migration of the ENS progenitors but can also modulate the response of NCCs to GDNF [6, 124]. This provides evidence of interaction between two different pathways implicated in the pathogenesis of HSCR.
EDNRB gene and HSCR
The occurrence of multiple cases of both isolated HSCR and WS4 in an inbreed Old Order Mennonite community facilitated the mapping of another major HSCR susceptibility gene to the chromosomal region 13q22 [125, 126]. The gene identified on 13q22 was the endothelin type B receptor (EDNRB) which had a mutation that resulted in the W276C amino-acid change in the protein. In contrast to the recessive, fully penetrant defects in the rodent model, this human mutation was neither fully dominant nor fully recessive. The homozygous W276C mutation (CC) was more penetrant than the heterozygous (WC), and that penetrance was sex dependent. Individuals homozygous (CC) presented with WS4 features, while those with the heterozygous mutation (WC) presented with isolated HSCR. Furthermore, some family members with no W279C mutation were clinically affected. This implied the presence of additional predisposing genes among this closely-related group. In fact, a genetic modifier of HSCR found among the group was mapped to chromosome 21q21 [125]. Subsequent EDNRB mutation analyses conducted on both isolated HSCR and WS4 patients revealed other EDNRB mutations with similar genetic behavior to W279C. Homozygous EDNRB mutations were associated with WS4 [127, 128] and heterozygous mutations with isolated HSCR [58, 59, 129–134]. Overall, EDNRB mutations account for 5% of the isolated HSCR phenotype. Functional analyses of EDNRB missense mutations showed impairment of the intracellular signaling [132, 135, 136]. EDNRB mutations found this far, are mainly inherited from unaffected parents, and associated with short-segment aganglionosis.
EDN3 and ECE-1 genes
HSCR patients are being screened for mutations in the human EDN3 because of the HSCR-like phenotype presented by mice with disruption of the Edn3 gene. To the best of our knowledge, very few EDN3 mutations have been characterized in HSCR patients. With very few exceptions [94], heterozygous EDN3 mutations are associated with isolated HSCR [137, 138] and homozygous mutations with WS4 [139, 140].
Again a knock-out mouse model provided evidence of the involvement of another member of the EDNRB pathway, ECE-1, in HSCR [141]. The gene encodes the endothelin converting enzyme (ECE-1), which cleaves the large inactive endothelins into smaller 21 amino-acids active endothelins. Mice carrying an Ece-1 null mutation (no protein is synthesized) present with craniofacial and cardiac abnormalities, absence of melanocytes, and absence of the enteric neurons in the distal gut. This phenotype is similar to that presented by mice with mutations in the genes encoding other members of the EDNRB pathway (EDN3 and EDNRB). To date, only one mutation in the ECE-1 gene has been found and the patient was affected with syndromic HSCR [142].
As a general rule, severe homozygous mutations in genes involved in the EDNRB pathway are mainly associated with WS4 (absence of enteric ganglia and epidermal melanocytes, both neural crest cell derivatives). The association of homozygous mutations with WS4 and heterozygous mutations with isolated HSCR may indicate that melanocytes and enteric ganglia differ in sensitivity to the varying levels of EDNRB signaling [143].
The restriction of aganglionosis to the distal colon in mice with EBNRB and EDN3 deficiency and the fact that HSCR patients with mutations in these genes mainly present with short-segment aganglionosis suggested that the EDNRB signaling pathway is only required during the later stages of the colonization of the colon [144, 145]. However, it has recently been shown that the EDNRB signaling pathway is required for the colonization of both colon and small bowel [124]. The colonization process is subject to distinct spatial and temporal signaling requirements, and at some stage EDNRB signaling enhances the ability of the NCCs to migrate into the distal bowel [6].
ZFHX1B (previously SIP1)
The observation of a translocation involving the ZFHX1B locus (2q22) in a patient with HSCR disease, microcephaly, mental retardation, epilepsy and characteristic facial appearance, led to the first documentation of ZFHX1B involvement in this syndromic form of HSCR [146]. Other chromosomal abnormalities involving 2q22 and mutations in the ZFHX1B gene are being described in patients with similar clinical features (recently named Mowat–Wilson syndrome) although not all of them present with aganglionosis.
ZFHX1B encodes a transcriptional repressor (SIP1, Smad interacting protein 1), which interacts with several members of the Smad family. Some Smad proteins act as tranducers in signaling cascades critical to embryogenesis. It is not yet known how mutations in ZFHX1B may result in defects of the ENS, although it is tempting to speculate on a possible functional link between SIP1 and the signaling pathways currently known to be essential for the ENS development. As in SOX10, no mutations have been found in patients with isolated HSCR, and therefore ZFHX1B is unlikely to be major gene in non-syndromic HSCR [147–149].
KIAA1279
By homozygosity mapping, a novel locus on 10q21.3-q22.1 for Goldberg–Shprintzen syndrome (GOSHS) was identified in an inbreed family. Phenotypic features of GOSHS in this inbred family included microcephaly, polymicogyria, and mental retardation, as well as HSCR. Homozygous missense mutations were identified in the KIAA1279 gene at 10q22.1 [27]. This finding established the importance of KIAA1279 in both enteric and central nervous system development although the role of KIAA1279 is not yet understood. No mutations in this gene have been found in isolated HSCR patients.
Modifying genes and interaction between signaling pathways
As indicated above, the successful colonization of the gut by the ENS precursors depends on a coordinated and balanced network of interacting molecules (Fig. 2). Conceivably, there should be a functional and genetic link among these molecules for them to interact. The mechanisms underlying these interactions may help to explain the complexity of the HSCR phenotype and resolve puzzling genetic observations, e.g., that in some cases more than one mutated gene is needed to produce the phenotype, while (conversely) healthy individuals exist with mutations in HSCR genes. Interaction between pathways requires not only coordination among the pathway members but also with those molecules that mediate their interaction.
The RET and EDNRB signaling pathways were initially thought to be biochemically independent. However, the identification of a HSCR patient carrying both a RET mutation inherited from the healthy mother and a EDNRB mutation transmitted by the healthy father suggested that these two pathways were related, and indeed, that more than one mutation was needed for the manifestation of the phenotype. The latter is especially true when the effect of the mutation on the protein function is not severe [28]. The genetic interaction between mutations in RET and EDNRB in HSCR was verified in 2002 in an association study conducted on 43 Mennonite family trios segregating the W276C mutation in the EDNRB described above [64]. The study demonstrated the joint transmission of both the W276C mutation in EDNRB and HSCR-associated RET-SNPs in affected individuals. The combination of these two genotypes increased the penetrance of the W276C mutation and therefore the risk to disease. Genetic interaction between RET and EDNRB pathways has also been demonstrated in mice [64, 124, 150]. The fact that two mutated genes are needed for the manifestation of the disease also implies functional interaction. EDN3 and GDNF seem to have a synergistic effect on the proliferation of the undifferentiated ENS progenitors and an antagonistic effect on the migration of differentiated enteric ganglia. It appears that EDN3 has a variable distribution along the developing gut with differential effects on processes regulated by the RET. It has been firmly established that the interaction between these signaling pathways controls the ENS development throughout the intestine [6, 124]. However, both pathways have to be integrated by additional molecules or “mediators”. Protein kinase A has been suggested as a key component of the molecular mechanisms that mediate and link the RET and EDNRB signaling pathways [124]. Also, in mice, Sox10 has been shown to act on both Ret and EdnrB genes [26, 87–90] further linking these two signaling pathways. All the molecule members of these pathways/networks are not known. This means that genes involved in the development of the ENS still await discovery, and that DNA alterations in multiple genes have the potential to combine and hinder a phenotype. Obviously, defective functioning of these still unknown “mediators” could modify the outcome of the development of the ENS. RET and EDNRB are central to the genesis of HSCR but little is known about the influence of the genetic background. Unknown loci (that could encode protein members of the RET and EDNRB pathways) can modify RET expression and act as a disease promoting or suppressing genes (modifiers). A linkage study conducted on 12 HSCR families enriched for L-HSCR form, demonstrated linkage to RET in all but one family. However, 6 out of the 11 families linked to RET, also showed linkage to the 9q31 locus. Interestingly, no severe RET mutations were detected in those 6 families. The effect of a mutated gene in the 9q31 region is thought to be required to produce the HSCR phenotype in those individuals bearing weak RET mutations [30]. A genome-wide scan on 49 S-HSCR families detected linkage to three chromosomal regions, 10q12, 3p21, and 19q12. Since S-HSCR did not segregate in the absence of RET, the authors suggested that 3q21 and 19q12 loci are RET-dependent, therefore, modifiers of the RET expression [29]. A recent study on the 3p21 chromosomal region narrowed down a HSCR-associated region comprising three genes involved in neurological phenotypes [151]. Other examples of interaction include those reported between RET and genes of the NTF3/NTRK3 signaling pathway, which also plays an essential role in the ENS development [152].
These studies emphasize the central role of RET in all forms of HSCR (short and long) and explained the non-Mendelian inheritance of the disease. Also, they suggest that the genetics of long- and short-segment HSCR may depend on the effects of the different RET modifiers.
Other HSCR candidate genes
Mouse models and syndromes associated with HSCR provide insights into the genes that may share a common signaling pathway involved in the development of the ENS and therefore in the pathogenesis of HSCR. It is therefore logical to study the possible contribution of these genes to HSCR. This can be illustrated by the example posed by the Indian hedgehog gene (IHH). The hedgehog gene family encodes a group of secreted signaling molecules that are essential for growth and patterning of many different body parts of vertebrate and invertebrate embryos [153]. In particular, Ihh signaling controls growth of bones and is required for the proper development of the ENS and the intestinal stem cell proliferation and differentiation [154]. Ihh mutant mice present with dilated colon with abnormally thin wall, and enteric neurons missing from parts of the small intestine and from the dilated regions of the colon. This HSCR-like phenotype is observed with an incomplete penetrance of 50%, which suggest that interaction with other factors will be required for full expression of the phenotype. These features are strikingly similar to those observed in HSCR patients. In humans, mutations in the IHH gene (2q33-35) are associated with congenital limb malformations [155] and other skeletal dysplasias [156] some of which are also seen in some HSCR patients [3, 4]. Yet, IHH mutation analysis in over 60 HSCR patients with no mutations in the HSCR genes described so far, reveal no coding region mutations that could account for the disease [157].
Similar results were obtained for the human L1CAM gene. This gene encodes the L1 cell adhesion molecule involved in the development of the nervous system [158]. Mutations in L1CAM are linked to a recessive form of congenital hydrocephalus [159]. The detection of L1CAM mutations in individuals with congenital hydrocephalus and HSCR [160, 161] and the fact that L1CAM maps to chromosome Xq28, (which could account for the higher penetrance of HSCR in males) encouraged the mutational screening of this gene in isolated HSCR patients [162]. Although no coding region mutations were identified, it was hypothesized that L1CAM-mediated cell adhesion may be important for the ability of ganglion cell precursors to populate the gut, and that the L1CAM gene could modify the effects of a Hirschsprung disease-associated gene to cause intestinal aganglionosis.
Genome-wide association studies (GWASs) and HSCR
Current technology allows the search of the whole genome for common variants affecting the incidence of a disease. Recently, our group conducted the first GWAS on HSCR patients through which we identified the neuregulin1 gene (NRG1) as a new HSCR susceptibility gene. NRG1 (a signaling protein) and its receptors (the ErbB family of tyrosine kinase receptors) are among the molecular regulators of the NCCs’ development by promoting neuronal survival amid other biological functions. In this study, which was conducted on individuals of Chinese origin, besides the RET-SNPs, the strongest overall associations were found for two SNPs located in intron 1 of NRG1. Importantly, NRG1 SNPs increased risk to disease in the presence of the RET HSCR-associated SNPs [163] implying genetic and most likely, functional interaction between these two genes. Studies are underway to further identify the NRG1 variants that disturb the function of the gene (Garcia-Barceló and Tam et al. unpublished data).
Genetic counseling
In isolated HSCR, a relatively precise recurrence risk tailored to individual families could be estimated based on the estimates provided by Badner [164]. The highest recurrence risk is for a male sib of a female proband with L-HSCR [3]. Nonetheless, the reduced penetrance of the HSCR mutations makes it difficult to rationally predict and assess the risk to disease. Genetic testing is only performed on a research basis, and due to the advances of the surgical management of HSCR, its utility is questionable.
As outlined earlier, mutations in the RET proto-oncogene are also the underlying cause of the inherited cancer syndromes MEN2A, MEN2B, and FMTC. In HSCR patients, RET mutations are dispersed throughout the gene, while in MEN2A and FMTC patients, mutations are clustered in the cysteine codons of the RET extracellular domain (exons 10 and 11). Although HSCR and MEN2A are two different entities, occasionally they co-segregate in some families [165–169], and affected individuals carry a single mutation in exons 10 or 11. Importantly, RET mutations identical to those found in MEN2A have been detected in HSCR patients with no clinical symptoms of MEN2A [170, 171]. This means that some HSCR patients may be exposed to a highly increased risk of tumors, where HSCR patients carry these tumor-specific mutations, exploration of the family history of MEN2A and periodic screening for tumors is advisable. In families segregating both MEN2A and HSCR, RET gene testing, tumor screening, and prophylactic thyroidectomy is also warranted.
Future directions
Although modern surgical procedures have already achieved a high success rate of HSCR treatment, a better understanding of the mechanisms involved in the disease pathogenesis would enable improved diagnosis, prevention, and treatment.
The major breakthrough in the study of the pathogenesis of HSCR has been the demonstration of the genetic and functional interaction between the RET and EDNRB signaling pathways and their establishment as key players in the development of the ENS. These important findings should lead to the study of the complete gene network that makes the genesis of the ENS possible. Regarding HSCR gene-discovery, additional GWAS and whole-genome sequencing of DNA from HSCR patients are currently underway.
The GWAS studies are aimed at the discovery of genes whose common variants (SNPs) are associated with the disease, as per the common-disease-common variant hypothesis, whereby common variants (present in >1% of the population) might contribute to susceptibility to common diseases. These disease-associated common variants have a modest contribution to risk. Thus, more disease-associated functional common variants are to be identified when the disease results from their summative effect. Importantly, several lines of evidence indicate that in addition to common variants/SNPs, deleterious rare variants also contribute to the multifactorial inheritance of complex diseases although their effect and mode of inheritance is usually masked by the effect of other disease-contributing genes. The genes in which disease-associated common variants are found are to be considered as candidates for the search of deleterious rare variants (mutations) [172, 173]. Indeed, HSCR constitute a perfect example of the above. The RET gene contains high-frequency common variants with modest effects as well as deleterious rare variants (mutations). The latter may be transmitted in an autosomal dominant manner with reduced penetrance giving rise to familial HSCR. Because mutations are rare in the population, they must be identified by sequencing in cases and controls in each study. Yet, the contribution of common and rare variants to a disease or in particular, to HSCR, is not necessarily independent. Common variants may act as modifiers of the mutation effects as exemplified with the EDNRB W276C mutation, whose penetrance is increased by the presence of RET HSCR-associated SNPs in the same individual.
For obvious reasons, conducting gene or protein expression analyses for the study of HSCR and other human diseases that result from gene dysfunction during development is not feasible. Mice can provide access to the study of human genes and proteins that have an equivalent in mice. Scientists are now resorting to the isolation individual mouse cell types by making use of stem cell research. This has allowed the study the specific requirements of the gut neural crest stem cells (NCSCs) [124, 174, 175]. A recent study has shown that Prokineticin-1 (Prok-1) can induce both proliferation and expression of differentiation markers of Ret deficient mouse NCCs, suggesting that Prok-1 may provide a complementary pathway to GDNF/Ret signaling during the ENS development. This indicates that Prok-1 crosstalks with GDNF/Ret signaling and probably provides an additional layer of signaling refinement to maintain proliferation and differentiation of enteric NCCs. If the behavior of the gut NCSCs is better understood, it may be possible to treat HSCR by transplanting NCSCs directly into the aganglionic gut. It will be intriguing to determine whether these NCSCs are able to mature and engraft in the forming gut and enhance bowel motility, and further research of this kind should yield new therapeutic approaches.
The HSCR phenotype may therefore be a consequence of the interplay and/or accumulation of both common and rare deleterious DNA variants in gene members of the pathways involved in ENS development, and despite the importance of RET, additional HSCR susceptibility genes exist and are currently being uncovered through both genetic and cell functional studies.
References
Tam PK, Garcia-Barcelo M (2004) Molecular genetics of Hirschsprung’s disease. Semin Pediatr Surg 13:236–248
Torfs C (2004) An epidemiological study of Hirschsprung’ disease in a multiracial California population. Third International Meeting: Hirschsprung’s disease and related neurocristophaties Evian, France 1998
Amiel J, Lyonnet S (2001) Hirschsprung disease, associated syndromes, and genetics: a review. J Med Genet 38:729–739
Moore SW (2006) The contribution of associated congenital anomalies in understanding Hirschsprung’s disease. Pediatr Surg Int 22:305–315
Burns AJ, Douarin NM (1998) The sacral neural crest contributes neurons and glia to the post-umbilical gut: spatiotemporal analysis of the development of the enteric nervous system. Development 125:4335–4347
Kruger GM, Mosher JT, Tsai YH, Yeager KJ, Iwashita T, Gariepy CE, Morrison SJ (2003) Temporally distinct requirements for endothelin receptor B in the generation and migration of gut neural crest stem cells. Neuron 40:917–929
Gariepy CE (2001) Intestinal motility disorders and development of the enteric nervous system. Pediatr Res 49:605–613
Amiel J, Sproat-Emison E, Garcia-Barcelo M, Lantieri F, Burzynski G, Borrego S, Pelet A, Arnold S, Miao X, Griseri P, Brooks AS, Antinolo G, de Pontual L, Clement-Ziza M, Munnich A, Kashuk C, West K, Wong KK, Lyonnet S, Chakravarti A, Tam PK, Ceccherini I, Hofstra RM, Fernandez R (2008) Hirschsprung disease, associated syndromes and genetics: a review. J Med Genet 45:1–14
Swenson O (1996) Early history of the therapy of Hirschsprung’s disease: facts and personal observations over 50 years. J Pediatr Surg 31:1003–1008
Simpson NE, Kidd KK, Goodfellow PJ, McDermid H, Myers S, Kidd JR, Jackson CE, Duncan AM, Farrer LA, Brasch K (1987) Assignment of multiple endocrine neoplasia type 2A to chromosome 10 by linkage. Nature 328:528–530
Mulligan LM, Kwok JB, Healey CS, Elsdon MJ, Eng C, Gardner E, Love DR, Mole SE, Moore JK, Papi L (1993) Germ-line mutations of the RET proto-oncogene in multiple endocrine neoplasia type 2A. Nature 363:458–460
Grieco M, Santoro M, Berlingieri MT, Donghi R, Pierotti MA, Della PG, Fusco A, Vecchio G (1988) Molecular cloning of PTC, a new oncogene found activated in human thyroid papillary carcinomas and their lymph node metastases. Ann N Y Acad Sci 551:380–381
Grieco M, Santoro M, Berlingieri MT, Melillo RM, Donghi R, Bongarzone I, Pierotti MA, Della PG, Fusco A, Vecchio G (1990) PTC is a novel rearranged form of the ret proto-oncogene and is frequently detected in vivo in human thyroid papillary carcinomas. Cell 60:557–563
Donghi R, Sozzi G, Pierotti MA, Biunno I, Miozzo M, Fusco A, Grieco M, Santoro M, Vecchio G, Spurr NK (1989) The oncogene associated with human papillary thyroid carcinoma (PTC) is assigned to chromosome 10 q11-q12 in the same region as multiple endocrine neoplasia type 2A (MEN2A). Oncogene 4:521–523
Donis-Keller H, Dou S, Chi D, Carlson KM, Toshima K, Lairmore TC, Howe JR, Moley JF, Goodfellow P, Wells SA Jr (1993) Mutations in the RET proto-oncogene are associated with MEN 2A and FMTC. Hum Mol Genet 2:851–856
Martucciello G, Bicocchi MP, Dodero P, Lerone M, Silengo M, Puliti A, Gimelli G (1992) Total colonic aganglionosis associated with interstitial deletion of the long arm of chromosome 10. Pediatr Surg Int 7:308–310
Fewtrell MS, Tam PK, Thomson AH, Fitchett M, Currie J, Huson SM, Mulligan LM (1994) Hirschsprung’s disease associated with a deletion of chromosome 10 (q11.2q21.2): a further link with the neurocristopathies? J Med Genet 31:325–327
Angrist M, Kauffman E, Slaugenhaupt SA, Matise TC, Puffenberger EG, Washington SS, Lipson A, Cass DT, Reyna T, Weeks DE (1993) A gene for Hirschsprung disease (megacolon) in the pericentromeric region of human chromosome 10. Nat Genet 4:351–356
Lyonnet S, Bolino A, Pelet A, Abel L, Nihoul-Fekete C, Briard ML, Mok-Siu V, Kaariainen H, Martucciello G, Lerone M (1993) A gene for Hirschsprung disease maps to the proximal long arm of chromosome 10. Nat Genet 4:346–350
Schuchardt A, D’Agati V, Larsson-Blomberg L, Costantini F, Pachnis V (1995) RET-deficient mice: an animal model for Hirschsprung’s disease and renal agenesis. J Intern Med 238:327–332
Romeo G, Ronchetto P, Luo Y, Barone V, Seri M, Ceccherini I, Pasini B, Bocciardi R, Lerone M, Kaariainen H (1994) Point mutations affecting the tyrosine kinase domain of the RET proto-oncogene in Hirschsprung’s disease. Nature 367:377–378
Edery P, Lyonnet S, Mulligan LM, Pelet A, Dow E, Abel L, Holder S, Nihoul-Fekete C, Ponder BA, Munnich A (1994) Mutations of the RET proto-oncogene in Hirschsprung’s disease. Nature 367:378–380
Brooks AS, Bertoli-Avella AM, Burzynski GM, Breedveld GJ, Osinga J, Boven LG, Hurst JA, Mancini GM, Lequin MH, de Coo RF, Matera I, de Graaff E, Meijers C, Willems PJ, Tibboel D, Oostra BA, Hofstra RM (2005) Homozygous nonsense mutations in KIAA1279 are associated with malformations of the central and enteric nervous systems. Am J Hum Genet 77:120–126
Natarajan D, Marcos-Gutierrez C, Pachnis V, de Graaff E (2002) Requirement of signalling by receptor tyrosine kinase RET for the directed migration of enteric nervous system progenitor cells during mammalian embryogenesis. Development 129:5151–5160
Iwashita T, Kruger GM, Pardal R, Kiel MJ, Morrison SJ (2003) Hirschsprung disease is linked to defects in neural crest stem cell function. Science 301:972–976
Stanchina L, Baral V, Robert F, Pingault V, Lemort N, Pachnis V, Goossens M, Bondurand N (2006) Interactions between Sox10, Edn3 and Ednrb during enteric nervous system and melanocyte development. Dev Biol 295:232–249
Tam PK, Gould SJ, Martucciello G, Biddolph S, Takahashi M, Jasonni V (1996) Ret protein in the human fetal rectum. J Pediatr Surg 31:568–571
Auricchio A, Griseri P, Carpentieri ML, Betsos N, Staiano A, Tozzi A, Priolo M, Thompson H, Bocciardi R, Romeo G, Ballabio A, Ceccherini I (1999) Double heterozygosity for a RET substitution interfering with splicing and an EDNRB missense mutation in Hirschsprung disease. Am J Hum Genet 64:1216–1221
Gabriel SB, Salomon R, Pelet A, Angrist M, Amiel J, Fornage M, Attie-Bitach T, Olson JM, Hofstra R, Buys C, Steffann J, Munnich A, Lyonnet S, Chakravarti A (2002) Segregation at three loci explains familial and population risk in Hirschsprung disease. Nat Genet 31:89–93
Bolk S, Pelet A, Hofstra RM, Angrist M, Salomon R, Croaker D, Buys CH, Lyonnet S, Chakravarti A (2000) A human model for multigenic inheritance: phenotypic expression in Hirschsprung disease requires both the RET gene and a new 9q31 locus. Proc Natl Acad Sci USA 97:268–273
Jing S, Wen D, Yu Y, Holst PL, Luo Y, Fang M, Tamir R, Antonio L, Hu Z, Cupples R, Louis JC, Hu S, Altrock BW, Fox GM (1996) GDNF-induced activation of the ret protein tyrosine kinase is mediated by GDNFR-alpha, a novel receptor for GDNF. Cell 85:1113–1124
Treanor JJ, Goodman L, de Sauvage F, Stone DM, Poulsen KT, Beck CD, Gray C, Armanini MP, Pollock RA, Hefti F, Phillips HS, Goddard A, Moore MW, Buj-Bello A, Davies AM, Asai N, Takahashi M, Vandlen R, Henderson CE, Rosenthal A (1996) Characterization of a multicomponent receptor for GDNF. Nature 382:80–83
Bar KJ, Facer P, Williams NS, Tam PK, Anand P (1997) Glial-derived neurotrophic factor in human adult and fetal intestine and in Hirschsprung’s disease. Gastroenterology 112:1381–1385
Pachnis V, Mankoo B, Costantini F (1993) Expression of the c-ret proto-oncogene during mouse embryogenesis. Development 119:1005–1017
Taraviras S, Marcos-Gutierrez CV, Durbec P, Jani H, Grigoriou M, Sukumaran M, Wang LC, Hynes M, Raisman G, Pachnis V (1999) Signalling by the RET receptor tyrosine kinase and its role in the development of the mammalian enteric nervous system. Development 126:2785–2797
Hofstra RM, Landsvater RM, Ceccherini I, Stulp RP, Stelwagen T, Luo Y, Pasini B, Hoppener JW, van Amstel HK, Romeo G (1994) A mutation in the RET proto-oncogene associated with multiple endocrine neoplasia type 2B and sporadic medullary thyroid carcinoma. Nature 367:375–376
Airaksinen MS, Saarma M (2002) The GDNF family: signalling, biological functions and therapeutic value. Nat Rev Neurosci 3:383–394
Pasini B, Borrello MG, Greco A, Bongarzone I, Luo Y, Mondellini P, Alberti L, Miranda C, Arighi E, Bocciardi R (1995) Loss of function effect of RET mutations causing Hirschsprung disease. Nat Genet 10:35–40
Iwashita T, Murakami H, Asai N, Takahashi M (1996) Mechanism of ret dysfunction by Hirschsprung mutations affecting its extracellular domain. Hum Mol Genet 5:1577–1580
Pelet A, Geneste O, Edery P, Pasini A, Chappuis S, Atti T, Munnich A, Lenoir G, Lyonnet S, Billaud M (1998) Various mechanisms cause RET-mediated signaling defects in Hirschsprung’s disease. J Clin Invest 101:1415–1423
Geneste O, Bidaud C, De Vita G, Hofstra RM, Tartare-Deckert S, Buys CH, Lenoir GM, Santoro M, Billaud M (1999) Two distinct mutations of the RET receptor causing Hirschsprung’s disease impair the binding of signalling effectors to a multifunctional docking site. Hum Mol Genet 8:1989–1999
Iwashita T, Kurokawa K, Qiao S, Murakami H, Asai N, Kawai K, Hashimoto M, Watanabe T, Ichihara M, Takahashi M (2001) Functional analysis of RET with Hirschsprung mutations affecting its kinase domain. Gastroenterology 121:24–33
Kashuk CS, Stone EA, Grice EA, Portnoy ME, Green ED, Sidow A, Chakravarti A, McCallion AS (2005) Phenotype-genotype correlation in Hirschsprung disease is illuminated by comparative analysis of the RET protein sequence. Proc Natl Acad Sci USA 102:8949–8954
Edery P, Pelet A, Mulligan LM, Abel L, Attie T, Dow E, Bonneau D, David A, Flintoff W, Jan D (1994) Long segment and short segment familial Hirschsprung’s disease: variable clinical expression at the RET locus. J Med Genet 31:602–606
Yin L, Barone V, Seri M, Bolino A, Bocciardi R, Ceccherini I, Pasini B, Tocco T, Lerone M, Cywes S (1994) Heterogeneity and low detection rate of RET mutations in Hirschsprung disease. Eur J Hum Genet 2:272–280
Angrist M, Bolk S, Thiel B, Puffenberger EG, Hofstra RM, Buys CH, Cass DT, Chakravarti A (1995) Mutation analysis of the RET receptor tyrosine kinase in Hirschsprung disease. Hum Mol Genet 4:821–830
Attie T, Pelet A, Edery P, Eng C, Mulligan LM, Amiel J, Boutrand L, Beldjord C, Nihoul-Fekete C, Munnich A (1995) Diversity of RET proto-oncogene mutations in familial and sporadic Hirschsprung disease. Hum Mol Genet 4:1381–1386
Yin L, Seri M, Barone V, Tocco T, Scaranari M, Romeo G (1996) Prevalence and parental origin of de novo RET mutations in Hirschsprung’s disease. Eur J Hum Genet 4:356–358
Kusafuka T, Wang Y, Puri P (1997) Mutation analysis of the RET, the endothelin-B receptor, and the endothelin-3 genes in sporadic cases of Hirschsprung’s disease. J Pediatr Surg 32:501–504
Svensson PJ, Molander ML, Eng C, Anvret M, Nordenskjold A (1998) Low frequency of RET mutations in Hirschsprung disease in Sweden. Clin Genet 54:39–44
Inoue K, Shimotake T, Iwai N (2000) Mutational analysis of RET/GDNF/NTN genes in children with total colonic aganglionosis with small bowel involvement. Am J Med Genet 93:278–284
Hofstra RM, Wu Y, Stulp RP, Elfferich P, Osinga J, Maas SM, Siderius L, Brooks AS, vd Ende JJ, Heydendael VM, Severijnen RS, Bax KM, Meijers C, Buys CH (2000) RET and GDNF gene scanning in Hirschsprung patients using two dual denaturing gel systems. Hum Mutat 15:418–429
Sancandi M, Ceccherini I, Costa M, Fava M, Chen B, Wu Y, Hofstra R, Laurie T, Griffths M, Burge D, Tam PK (2000) Incidence of RET mutations in patients with Hirschsprung’s disease. J Pediatr Surg 35:139–142
Julies MG, Moore SW, Kotze MJ, du Plessis L (2001) Novel RET mutations in Hirschsprung’s disease patients from the diverse South African population. Eur J Hum Genet 9:419–423
Seri M, Yin L, Barone V, Bolino A, Celli I, Bocciardi R, Pasini B, Ceccherini I, Lerone M, Kristoffersson U, Larsson LT, Casasa JM, Cass DT, Abramowicz MJ, Vanderwinden JM, Kravcenkiene I, Baric I, Silengo M, Martucciello G, Romeo G (1997) Frequency of RET mutations in long- and short-segment Hirschsprung disease. Hum Mutat 9:243–249
Li JC, Ding SP, Song Y, Li MJ (2002) Mutation of RET gene in Chinese patients with Hirschsprung’s disease. World J Gastroenterol 8:1108–1111
Solari V, Ennis S, Yoneda A, Wong L, Messineo A, Hollwarth ME, Green A, Puri P (2003) Mutation analysis of the RET gene in total intestinal aganglionosis by wave DNA fragment analysis system. J Pediatr Surg 38:497–501
Gath R, Goessling A, Keller KM, Koletzko S, Coerdt W, Muntefering H, Wirth S, Hofstra RM, Mulligan L, Eng C, von Deimling A (2001) Analysis of the RET, GDNF, EDN3, and EDNRB genes in patients with intestinal neuronal dysplasia and Hirschsprung disease. Gut 48:671–675
Garcia-Barcelo M, Sham MH, Lee WS, Lui VC, Chen BL, Wong KK, Wong JS, Tam PK (2004) Highly recurrent RET mutations and novel mutations in genes of the receptor tyrosine kinase and endothelin receptor B pathways in Chinese patients with sporadic Hirschsprung disease. Clin Chem 50:93–100
Borrego S, Saez ME, Ruiz A, Gimm O, Lopez-Alonso M, Antinolo G, Eng C (1999) Specific polymorphisms in the RET proto-oncogene are over-represented in patients with Hirschsprung disease and may represent loci modifying phenotypic expression. J Med Genet 36:771–774
Fitze G, Schreiber M, Kuhlisch E, Schackert HK, Roesner D (1999) Association of RET protooncogene codon 45 polymorphism with Hirschsprung disease. Am J Hum Genet 65:1469–1473
Ceccherini I, Hofstra RM, Luo Y, Stulp RP, Barone V, Stelwagen T, Bocciardi R, Nijveen H, Bolino A, Seri M (1994) DNA polymorphisms and conditions for SSCP analysis of the 20 exons of the ret proto-oncogene. Oncogene 9:3025–3029
Garcia-Barcelo MM, Sham MH, Lui VC, Chen BL, Song YQ, Lee WS, Yung SK, Romeo G, Tam PK (2003) Chinese patients with sporadic Hirschsprung’s disease are predominantly represented by a single RET haplotype. J Med Genet 40:e122
Carrasquillo MM, McCallion AS, Puffenberger EG, Kashuk CS, Nouri N, Chakravarti A (2002) Genome-wide association study and mouse model identify interaction between RET and EDNRB pathways in Hirschsprung disease. Nat Genet 32:237–244
Fitze G, Cramer J, Ziegler A, Schierz M, Schreiber M, Kuhlisch E, Roesner D, Schackert HK (2002) Association between c135G/A genotype and RET proto-oncogene germline mutations and phenotype of Hirschsprung’s disease. Lancet 359:1200–1205
Griseri P, Pesce B, Patrone G, Osinga J, Puppo F, Sancandi M, Hofstra R, Romeo G, Ravazzolo R, Devoto M, Ceccherini I (2002) A rare haplotype of the RET proto-oncogene is a risk-modifying allele in Hirschsprung disease. Am J Hum Genet 71:969–974
Borrego S, Wright FA, Fernandez RM, Williams N, Lopez-Alonso M, Davuluri R, Antinolo G, Eng C (2003) A founding locus within the RET proto-oncogene may account for a large proportion of apparently sporadic Hirschsprung disease and a subset of cases of sporadic medullary thyroid carcinoma. Am J Hum Genet 72:88–100
Borrego S, Ruiz A, Saez ME, Gimm O, Gao X, Lopez-Alonso M, Hernandez A, Wright FA, Antinolo G, Eng C (2000) RET genotypes comprising specific haplotypes of polymorphic variants predispose to isolated Hirschsprung disease. J Med Genet 37:572–578
Fitze G, Appelt H, Konig IR, Gorgens H, Stein U, Walther W, Gossen M, Schreiber M, Ziegler A, Roesner D, Schackert HK (2003) Functional haplotypes of the RET proto-oncogene promoter are associated with Hirschsprung disease (HSCR). Hum Mol Genet 12:3207–3214
Sancandi M, Griseri P, Pesce B, Patrone G, Puppo F, Lerone M, Martucciello G, Romeo G, Ravazzolo R, Devoto M, Ceccherini I (2003) Single nucleotide polymorphic alleles in the 5′ region of the RET proto-oncogene define a risk haplotype in Hirschsprung’s disease. J Med Genet 40:714–718
Garcia-Barcelo M, Ganster RW, Lui VC, Leon TY, So MT, Lau AM, Fu M, Sham MH, Knight J, Zannini MS, Sham PC, Tam PK (2005) TTF-1 and RET promoter SNPs: regulation of RET transcription in Hirschsprung’s disease. Hum Mol Genet 14:191–204
Burzynski GM, Nolte IM, Osinga J, Ceccherini I, Twigt B, Maas S, Brooks A, Verheij J, Menacho IP, Buys CH, Hofstra RM (2004) Localizing a putative mutation as the major contributor to the development of sporadic Hirschsprung disease to the RET genomic sequence between the promoter region and exon 2. Eur J Hum Genet 12:604–612
Burzynski GM, Nolte IM, Bronda A, Bos KK, Osinga J, Plaza Menacho I, Twigt B, Maas S, Brooks AS, Verheij JB, Buys CH, Hofstra RM (2005) Identifying candidate Hirschsprung disease-associated RET variants. Am J Hum Genet 76:850–858
Emison ES, McCallion AS, Kashuk CS, Bush RT, Grice E, Lin S, Portnoy ME, Cutler DJ, Green ED, Chakravarti A (2005) A common sex-dependent mutation in a RET enhancer underlies Hirschsprung disease risk. Nature 434:857–863
Moore MW, Klein RD, Farinas I, Sauer H, Armanini M, Phillips H, Reichardt LF, Ryan AM, Carver-Moore K, Rosenthal A (1996) Renal and neuronal abnormalities in mice lacking GDNF. Nature 382:76–79
Enomoto H, Araki T, Jackman A, Heuckeroth RO, Snider WD, Johnson EM Jr, Milbrandt J (1998) GFR alpha1-deficient mice have deficits in the enteric nervous system and kidneys. Neuron 21:317–324
Shen L, Pichel JG, Mayeli T, Sariola H, Lu B, Westphal H (2002) Gdnf haploinsufficiency causes Hirschsprung-like intestinal obstruction and early-onset lethality in mice. Am J Hum Genet 70:435–447
Angrist M, Bolk S, Halushka M, Lapchak PA, Chakravarti A (1996) Germline mutations in glial cell line-derived neurotrophic factor (GDNF) and RET in a Hirschsprung disease patient. Nat Genet 14:341–344
Doray B, Salomon R, Amiel J, Pelet A, Touraine R, Billaud M, Attie T, Bachy B, Munnich A, Lyonnet S (1998) Mutation of the RET ligand, neurturin, supports multigenic inheritance in Hirschsprung disease. Hum Mol Genet 7:1449–1452
Myers SM, Salomon R, Goessling A, Pelet A, Eng C, von Deimling A, Lyonnet S, Mulligan LM (1999) Investigation of germline GFR alpha-1 mutations in Hirschsprung disease. J Med Genet 36:217–220
Salomon R, Attie T, Pelet A, Bidaud C, Eng C, Amiel J, Sarnacki S, Goulet O, Ricour C, Nihoul-Fekete C, Munnich A, Lyonnet S (1996) Germline mutations of the RET ligand GDNF are not sufficient to cause Hirschsprung disease. Nat Genet 14:345–347
Ivanchuk SM, Myers SM, Eng C, Mulligan LM (1996) De novo mutation of GDNF, ligand for the RET/GDNFR-alpha receptor complex, in Hirschsprung disease. Hum Mol Genet 5:2023–2026
Chen B, Knowles CH, Scott M, Anand P, Williams NS, Milbrandt J, Tam PK (2002) Idiopathic slow transit constipation and megacolon are not associated with neurturin mutations. Neurogastroenterol Motil 14:513–517
Eketjall S, Ibanez CF (2002) Functional characterization of mutations in the GDNF gene of patients with Hirschsprung disease. Hum Mol Genet 11:325–329
Borghini S, Bocciardi R, Bonardi G, Matera I, Santamaria G, Ravazzolo R, Ceccherini I (2002) Hirschsprung associated GDNF mutations do not prevent RET activation. Eur J Hum Genet 10:183–187
Lui VC, Samy ET, Sham MH, Mulligan LM, Tam PK (2002) Glial cell line-derived neurotrophic factor family receptors are abnormally expressed in aganglionic bowel of a subpopulation of patients with Hirschsprung’s disease. Lab Invest 82:703–712
Lang D, Epstein JA (2003) Sox10 and Pax3 physically interact to mediate activation of a conserved c-RET enhancer. Hum Mol Genet 12:937–945
Lang D, Chen F, Milewski R, Li J, Lu MM, Epstein JA (2000) Pax3 is required for enteric ganglia formation and functions with Sox10 to modulate expression of c-ret. J Clin Invest 106:963–971
Zhu L, Lee HO, Jordan CS, Cantrell VA, Southard-Smith EM, Shin MK (2004) Spatiotemporal regulation of endothelin receptor-B by SOX10 in neural crest-derived enteric neuron precursors. Nat Genet 36:732–737
Cantrell VA, Owens SE, Chandler RL, Airey DC, Bradley KM, Smith JR, Southard-Smith EM (2004) Interactions between Sox10 and EdnrB modulate penetrance and severity of aganglionosis in the Sox10Dom mouse model of Hirschsprung disease. Hum Mol Genet 13(19):2289–2301
Lane PW, Liu HM (1984) Association of megacolon with a new dominant spotting gene (Dom) in the mouse. J Hered 75:435–439
Southard-Smith EM, Angrist M, Ellison JS, Agarwala R, Baxevanis AD, Chakravarti A, Pavan WJ (1999) The Sox10(Dom) mouse: modeling the genetic variation of Waardenburg-Shah (WS4) syndrome. Genome Res 9:215–225
Southard-Smith EM, Kos L, Pavan WJ (1998) Sox10 mutation disrupts neural crest development in Dom Hirschsprung mouse model. Nat Genet 18:60–64
Pingault V, Puliti A, Prehu MO, Samadi A, Bondurand N, Goossens M (1997) Human homology and candidate genes for the Dominant megacolon locus, a mouse model of Hirschsprung disease. Genomics 39:86–89
Herbarth B, Pingault V, Bondurand N, Kuhlbrodt K, Hermans-Borgmeyer I, Puliti A, Lemort N, Goossens M, Wegner M (1998) Mutation of the Sry-related Sox10 gene in dominant megacolon, a mouse model for human Hirschsprung disease. Proc Natl Acad Sci USA 95:5161–5165
Pingault V, Bondurand N, Kuhlbrodt K, Goerich DE, Prehu MO, Puliti A, Herbarth B, Hermans-Borgmeyer I, Legius E, Matthijs G, Amiel J, Lyonnet S, Ceccherini I, Romeo G, Smith JC, Read AP, Wegner M, Goossens M (1998) SOX10 mutations in patients with Waardenburg–Hirschsprung disease. Nat Genet 18:171–173
Pingault V, Guiochon-Mantel A, Bondurand N, Faure C, Lacroix C, Lyonnet S, Goossens M, Landrieu P (2000) Peripheral neuropathy with hypomyelination, chronic intestinal pseudo-obstruction and deafness: a developmental “neural crest syndrome” related to a SOX10 mutation. Ann Neurol 48:671–676
Pingault V, Girard M, Bondurand N, Dorkins H, Van Maldergem L, Mowat D, Shimotake T, Verma I, Baumann C, Goossens M (2002) SOX10 mutations in chronic intestinal pseudo-obstruction suggest a complex physiopathological mechanism. Hum Genet 111:198–206
Touraine RL, Attie-Bitach T, Manceau E, Korsch E, Sarda P, Pingault V, Encha-Razavi F, Pelet A, Auge J, Nivelon-Chevallier A, Holschneider AM, Munnes M, Doerfler W, Goossens M, Munnich A, Vekemans M, Lyonnet S (2000) Neurological phenotype in Waardenburg syndrome type 4 correlates with novel SOX10 truncating mutations and expression in developing brain. Am J Hum Genet 66:1496–1503
Inoue K, Shilo K, Boerkoel CF, Crowe C, Sawady J, Lupski JR, Agamanolis DP (2002) Congenital hypomyelinating neuropathy, central dysmyelination, and Waardenburg–Hirschsprung disease: phenotypes linked by SOX10 mutation. Ann Neurol 52:836–842
Inoue K, Tanabe Y, Lupski JR (1999) Myelin deficiencies in both the central and the peripheral nervous systems associated with a SOX10 mutation. Ann Neurol 46:313–318
Sham MH, Lui VC, Chen BL, Fu M, Tam PK (2001) Novel mutations of SOX10 suggest a dominant negative role in Waardenburg-Shah syndrome. J Med Genet 38:E30
Bondurand N, Kuhlbrodt K, Pingault V, Enderich J, Sajus M, Tommerup N, Warburg M, Hennekam RC, Read AP, Wegner M, Goossens M (1999) A molecular analysis of the Yemenite deaf-blind hypopigmentation syndrome: SOX10 dysfunction causes different neurocristopathies. Hum Mol Genet 8:1785–1789
Chan KK, Wong CK, Lui VC, Tam PK, Sham MH (2003) Analysis of SOX10 mutations identified in Waardenburg–Hirschsprung patients: differential effects on target gene regulation. J Cell Biochem 90:573–585
Dubreuil V, Hirsch MR, Pattyn A, Brunet JF, Goridis C (2000) The Phox2b transcription factor coordinately regulates neuronal cell cycle exit and identity. Development 127:5191–5201
Pattyn A, Morin X, Cremer H, Goridis C, Brunet JF (1999) The homeobox gene Phox2b is essential for the development of autonomic neural crest derivatives. Nature 399:366–370
Benailly HK, Lapierre JM, Laudier B, Amiel J, Attie T, De Blois MC, Vekemans M, Romana SP (2003) PMX2B, a new candidate gene for Hirschsprung’s disease. Clin Genet 64:204–209
Garcia-Barcelo M, Sham MH, Lui VC, Chen BL, Ott J, Tam PK (2003) Association study of PHOX2B as a candidate gene for Hirschsprung’s disease. Gut 52:563–567
Miao X, Garcia-Barcelo MM, So MT, Leon TY, Lau DK, Liu TT, Chan EK, Lan LC, Wong KK, Lui VC, Tam PK (2007) Role of RET and PHOX2B gene polymorphisms in risk of Hirschsprung’s disease in Chinese population. Gut 56:736
Trochet D, Bourdeaut F, Janoueix-Lerosey I, Deville A, de Pontual L, Schleiermacher G, Coze C, Philip N, Frebourg T, Munnich A, Lyonnet S, Delattre O, Amiel J (2004) Germline mutations of the paired-like homeobox 2B (PHOX2B) gene in neuroblastoma. Am J Hum Genet 74:761–764
Perri P, Bachetti T, Longo L, Matera I, Seri M, Tonini GP, Ceccherini I (2005) PHOX2B mutations and genetic predisposition to neuroblastoma. Oncogene 24:3050–3053
Fan J, Tam P, Woude GV, Ren Y (2004) Normalization and analysis of cDNA microarrays using within-array replications applied to neuroblastoma cell response to a cytokine. Proc Natl Acad Sci USA 101:1135–1140
Amiel J, Laudier B, ttie-Bitach T, Trang H, de Pontual L, Gener B, Trochet D, Etchevers H, Ray P, Simonneau M, Vekemans M, Munnich A, Gaultier C, Lyonnet S (2003) Polyalanine expansion and frameshift mutations of the paired-like homeobox gene PHOX2B in congenital central hypoventilation syndrome. Nat Genet 33:459–461
Bachetti T, Matera I, Borghini S, Di Duca M, Ravazzolo R, Ceccherini I (2005) Distinct pathogenetic mechanisms for PHOX2B associated polyalanine expansions and frameshift mutations in congenital central hypoventilation syndrome. Hum Mol Genet 14:1815–1824
Verloes A, Elmer C, Lacombe D, Heinrichs C, Rebuffat E, Demarquez JL, Moncla A, Adam E (1993) Ondine–Hirschsprung syndrome (Haddad syndrome). Further delineation in two cases and review of the literature. Eur J Pediatr 152:75–77
Lai D, Schroer B (2008) Haddad syndrome: a case of an infant with central congenital hypoventilation syndrome and Hirschsprung disease. J Child Neurol 23:341–343
Fitze G, Konig IR, Paditz E, Serra A, Schlafke M, Roesner D, Ziegler A, Schackert HK (2008) Compound effect of PHOX2B and RET gene variants in congenital central hypoventilation syndrome combined with Hirschsprung disease. Am J Med Genet A 146A:1486–1489
Lui VC, Cheng WW, Leon TY, Lau DK, Garcia-Bareclo MM, Miao XP, Kam MK, So MT, Chen Y, Wall NA, Sham MH, Tam PK (2008) Perturbation of hoxb5 signaling in vagal neural crests down-regulates ret leading to intestinal hypoganglionosis in mice. Gastroenterology 134:1104–1115
Fu M, Lui VC, Sham MH, Cheung ANY, Tam PK (2003) HOXB5 expression is spatially and temporarily regulated in human embryonic gut during neural crest cell colonization and differentiation of enteric neuroblasts. Dev Dyn 228:1–10
Garcia-Barcelo MM, Miao X, Lui VC, So MT, Ngan ES, Leon TY, Lau DK, Liu TT, Lao X, Guo W, Holden WT, Moore J, Tam PK (2007) Correlation between genetic variations in Hox clusters and Hirschsprung’s disease. Ann Hum Genet 71:526–536
Garcia-Barcelo MM, Lau DK, Ngan ES, Leon TY, Liu TT, So MT, Miao XP, Lui VC, Wong KK, Ganster RW, Cass DT, Croaker GD, Tam PK (2007) Evaluation of the thyroid transcription factor-1 gene (TITF1) as a Hirschsprung’s disease locus. Ann Hum Genet 71(Pt 6):746–754
Hosoda K, Hammer RE, Richardson JA, Baynash AG, Cheung JC, Giaid A, Yanagisawa M (1994) Targeted and natural (piebald-lethal) mutations of endothelin-B receptor gene produce megacolon associated with spotted coat color in mice. Cell 79:1267–1276
Baynash AG, Hosoda K, Giaid A, Richardson JA, Emoto N, Hammer RE, Yanagisawa M (1994) Interaction of endothelin-3 with endothelin-B receptor is essential for development of epidermal melanocytes and enteric neurons. Cell 79:1277–1285
Barlow A, de Graaff E, Pachnis V (2003) Enteric nervous system progenitors are coordinately controlled by the G protein-coupled receptor EDNRB and the receptor tyrosine kinase RET. Neuron 40:905–916
Puffenberger EG, Kauffman ER, Bolk S, Matise TC, Washington SS, Angrist M, Weissenbach J, Garver KL, Mascari M, Ladda R (1994) Identity-by-descent and association mapping of a recessive gene for Hirschsprung disease on human chromosome 13q22. Hum Mol Genet 3:1217–1225
Puffenberger EG, Hosoda K, Washington SS, Nakao K, de Wit D, Yanagisawa M, Chakravart A (1994) A missense mutation of the endothelin-B receptor gene in multigenic Hirschsprung’s disease. Cell 79:1257–1266
Attie T, Till M, Pelet A, Amiel J, Edery P, Boutrand L, Munnich A, Lyonnet S (1995) Mutation of the endothelin-receptor B gene in Waardenburg–Hirschsprung disease. Hum Mol Genet 4:2407–2409
Verheij JB, Kunze J, Osinga J, van Essen AJ, Hofstra RM (2002) ABCD syndrome is caused by a homozygous mutation in the EDNRB gene. Am J Med Genet 108:223–225
Sakai T, Nirasawa Y, Itoh Y, Wakizaka A (2000) Japanese patients with sporadic Hirschsprung: mutation analysis of the receptor tyrosine kinase proto-oncogene, endothelin-B receptor, endothelin-3, glial cell line-derived neurotrophic factor and neurturin genes: a comparison with similar studies. Eur J Pediatr 159:160–167
Amiel J, Attie T, Jan D, Pelet A, Edery P, Bidaud C, Lacombe D, Tam P, Simeoni J, Flori E, Nihoul-Fekete C, Munnich A, Lyonnet S (1996) Heterozygous endothelin receptor B (EDNRB) mutations in isolated Hirschsprung disease. Hum Mol Genet 5:355–357
Tanaka H, Moroi K, Iwai J, Takahashi H, Ohnuma N, Hori S, Takimoto M, Nishiyama M, Masaki T, Yanagisawa M, Sekiya S, Kimura S (1998) Novel mutations of the endothelin B receptor gene in patients with Hirschsprung’s disease and their characterization. J Biol Chem 273:11378–11383
Kusafuka T, Wang Y, Puri P (1996) Novel mutations of the endothelin-B receptor gene in isolated patients with Hirschsprung’s disease. Hum Mol Genet 5:347–349
Kusafuka T, Puri P (1997) Mutations of the endothelin-B receptor and endothelin-3 genes in Hirschsprung’s disease. Pediatr Surg Int 12:19–23
Auricchio A, Casari G, Staiano A, Ballabio A (1996) Endothelin-B receptor mutations in patients with isolated Hirschsprung disease from a non-inbred population. Hum Mol Genet 5:351–354
Abe Y, Sakurai T, Yamada T, Nakamura T, Yanagisawa M, Goto K (2000) Functional analysis of five endothelin-B receptor mutations found in human Hirschsprung disease patients. Biochem Biophys Res Commun 275:524–531
Fuchs S, Amiel J, Claudel S, Lyonnet S, Corvol P, Pinet F (2001) Functional characterization of three mutations of the endothelin B receptor gene in patients with Hirschsprung’s disease: evidence for selective loss of Gi coupling. Mol Med 7:115–124
Svensson PJ, Von Tell D, Molander ML, Anvret M, Nordenskjold A (1999) A heterozygous frameshift mutation in the endothelin-3 (EDN-3) gene in isolated Hirschsprung’s disease. Pediatr Res 45:714–717
Bidaud C, Salomon R, Van Camp G, Pelet A, Attie T, Eng C, Bonduelle M, Amiel J, Nihoul-Fekete C, Willems PJ, Munnich A, Lyonnet S (1997) Endothelin-3 gene mutations in isolated and syndromic Hirschsprung disease. Eur J Hum Genet 5:247–251
Edery P, Attie T, Amiel J, Pelet A, Eng C, Hofstra RM, Martelli H, Bidaud C, Munnich A, Lyonnet S (1996) Mutation of the endothelin-3 gene in the Waardenburg–Hirschsprung disease (Shah-Waardenburg syndrome). Nat Genet 12:442–444
Hofstra RM, Osinga J, Tan-Sindhunata G, Wu Y, Kamsteeg EJ, Stulp RP, Ravenswaaij-Arts C, Majoor-Krakauer D, Angrist M, Chakravarti A, Meijers C, Buys CH (1996) A homozygous mutation in the endothelin-3 gene associated with a combined Waardenburg type 2 and Hirschsprung phenotype (Shah-Waardenburg syndrome). Nat Genet 12:445–447
Yanagisawa H, Yanagisawa M, Kapur RP, Richardson JA, Williams SC, Clouthier DE, de Wit D, Emoto N, Hammer RE (1998) Dual genetic pathways of endothelin-mediated intercellular signaling revealed by targeted disruption of endothelin converting enzyme-1 gene. Development 125:825–836
Hofstra RM, Valdenaire O, Arch E, Osinga J, Kroes H, Loffler BM, Hamosh A, Meijers C, Buys CH (1999) A loss-of-function mutation in the endothelin-converting enzyme 1 (ECE-1) associated with Hirschsprung disease, cardiac defects, and autonomic dysfunction. Am J Hum Genet 64:304–308
McCallion AS, Chakravarti A (2001) EDNRB/EDN3 and Hirschsprung disease type II. Pigment Cell Res 14:161–169
Leibl MA, Ota T, Woodward MN, Kenny SE, Lloyd DA, Vaillant CR, Edgar DH (1999) Expression of endothelin 3 by mesenchymal cells of embryonic mouse caecum. Gut 44:246–252
Sidebotham EL, Woodward MN, Kenny SE, Lloyd DA, Vaillant CR, Edgar DH (2002) Localization and endothelin-3 dependence of stem cells of the enteric nervous system in the embryonic colon. J Pediatr Surg 37:145–150
Wakamatsu N, Yamada Y, Yamada K, Ono T, Nomura N, Taniguchi H, Kitoh H, Mutoh N, Yamanaka T, Mushiake K, Kato K, Sonta S, Nagaya M (2001) Mutations in SIP1, encoding Smad interacting protein-1, cause a form of Hirschsprung disease. Nat Genet 27:369–370
Mowat DR, Croaker GD, Cass DT, Kerr BA, Chaitow J, Ades LC, Chia NL, Wilson MJ (1998) Hirschsprung disease, microcephaly, mental retardation, and characteristic facial features: delineation of a new syndrome and identification of a locus at chromosome 2q22-q23. J Med Genet 35:617–623
Garavelli L, Donadio A, Zanacca C, Banchini G, Della GE, Bertani G, Albertini G, Del Rossi C, Zweier C, Rauch A, Zollino M, Neri G (2003) Hirschsprung disease, mental retardation, characteristic facial features, and mutation in the gene ZFHX1B (SIP1): confirmation of the Mowat–Wilson syndrome. Am J Med Genet 116A:385–388
Cerruti MP, Pastore G, Zweier C, Rauch A (2004) Mowat–Wilson syndrome and mutation in the zinc finger homeo box 1B gene: a well defined clinical entity. J Med Genet 41:E16
McCallion AS, Stames E, Conlon RA, Chakravarti A (2003) Phenotype variation in two-locus mouse models of Hirschsprung disease: tissue-specific interaction between Ret and Ednrb. Proc Natl Acad Sci USA 100:1826–1831
Garcia-Barcelo MM, Fong PY, Tang CS, Miao XP, So MT, Yuan ZW, Li L, Guo WH, Liu L, Wang B, Sun XB, Huang LM, Tou JF, Wong KK, Ngan ES, Lui VC, Cherny SS, Sham PC, Tam PK (2008) Mapping of a Hirschsprung’s disease locus in 3p21. Eur J Hum Genet 16:833–840
Fernandez RM, Sanchez-Mejias A, Mena MD, Ruiz-Ferrer M, Lopez-Alonso M, Antinolo G, Borrego S (2009) A novel point variant in NTRK3, R645C, suggests a role of this gene in the pathogenesis of Hirschsprung disease. Ann Hum Genet 73:19–25
Murone M, Rosenthal A, de Sauvage FJ (1999) Hedgehog signal transduction: from flies to vertebrates. Exp Cell Res 253:25–33
Ramalho-Santos M, Melton DA, McMahon AP (2000) Hedgehog signals regulate multiple aspects of gastrointestinal development. Development 127:2763–2772
Gao B, Guo J, She C, Shu A, Yang M, Tan Z, Yang X, Guo S, Feng G, He L (2001) Mutations in IHH, encoding Indian hedgehog, cause brachydactyly type A-1. Nat Genet 28:386–388
Hellemans J, Coucke PJ, Giedion A, De Paepe A, Kramer P, Beemer F, Mortier GR (2003) Homozygous mutations in IHH cause acrocapitofemoral dysplasia, an autosomal recessive disorder with cone-shaped epiphyses in hands and hips. Am J Hum Genet 72:1040–1046
Garcia-Barcelo MM, Lee WS, Sham MH, Lui VC, Tam PK (2003) Is there a role for the IHH gene in Hirschsprung’s disease? Neurogastroenterol Motil 15:663–668
Faissner A, Kruse J, Nieke J, Schachner M (1984) Expression of neural cell adhesion molecule L1 during development, in neurological mutants and in the peripheral nervous system. Brain Res 317:69–82
Van Camp G, Vits L, Coucke P, Lyonnet S, Schrander-Stumpel C, Darby J, Holden J, Munnich A, Willems PJ (1993) A duplication in the L1CAM gene associated with X-linked hydrocephalus. Nat Genet 4:421–425
Parisi MA, Kapur RP, Neilson I, Hofstra RM, Holloway LW, Michaelis RC, Leppig KA (2002) Hydrocephalus and intestinal aganglionosis: is L1CAM a modifier gene in Hirschsprung disease? Am J Med Genet 108:51–56
Okamoto N, Wada Y, Goto M (1997) Hydrocephalus and Hirschsprung’s disease in a patient with a mutation of L1CAM. J Med Genet 34:670–671
Hofstra RM, Elfferich P, Osinga J, Verlind E, Fransen E, Lopez PJ, Die-Smulders CE, Stolte-Dijkstra I, Buys CH (2002) Hirschsprung disease and L1CAM: is the disturbed sex ratio caused by L1CAM mutations? J Med Genet 39:E11
Garcia-Barcelo MM, Tang CS, Ngan ES, Lui VC, Chen Y, So MT, Leon TY, Miao XP, Shum CK, Liu FQ, Yeung MY, Yuan ZW, Guo WH, Liu L, Sun XB, Huang LM, Tou JF, Song YQ, Chan D, Cheung KM, Wong KK, Cherny SS, Sham PC, Tam PK (2009) Genome-wide association study identifies NRG1 as a susceptibility locus for Hirschsprung’s disease. Proc Natl Acad Sci USA 106:2694–2699
Badner JA, Sieber WK, Garver KL, Chakravarti A (1990) A genetic study of Hirschsprung disease. Am J Hum Genet 46:568–580
Borst MJ, VanCamp JM, Peacock ML, Decker RA (1995) Mutational analysis of multiple endocrine neoplasia type 2A associated with Hirschsprung’s disease. Surgery 117:386–391
Mulligan LM, Eng C, Attie T, Lyonnet S, Marsh DJ, Hyland VJ, Robinson BG, Frilling A, Verellen-Dumoulin C, Safar A (1994) Diverse phenotypes associated with exon 10 mutations of the RET proto-oncogene. Hum Mol Genet 3:2163–2167
Reynolds LF, Eng C (1995) RET mutations in multiple endocrine neoplasia type 2 and Hirschsprung disease. Curr Opin Pediatr 7:702–709
Cosma MP, Panariello L, Quadro L, Dathan NA, Fattoruso O, Colantuoni V (1996) A mutation in the RET proto-oncogene in Hirschsprung’s disease affects the tyrosine kinase activity associated with multiple endocrine neoplasia type 2A and 2B. Biochem J 314(Pt 2):397–400
Inoue K, Shimotake T, Inoue K, Tokiwa K, Iwai N (1999) Mutational analysis of the RET proto-oncogene in a kindred with multiple endocrine neoplasia type 2A and Hirschsprung’s disease. J Pediatr Surg 34:1552–1554
Romeo G, Ceccherini I, Celli J, Priolo M, Betsos N, Bonardi G, Seri M, Yin L, Lerone M, Jasonni V, Martucciello G (1998) Association of multiple endocrine neoplasia type 2 and Hirschsprung disease. J Intern Med 243:515–520
Sijmons RH, Hofstra RM, Wijburg FA, Links TP, Zwierstra RP, Vermey A, Aronson DC, Tan-Sindhunata G, Brouwers-Smalbraak GJ, Maas SM, Buys CH (1998) Oncological implications of RET gene mutations in Hirschsprung’s disease. Gut 43:542–547
Bodmer W, Bonilla C (2008) Common and rare variants in multifactorial susceptibility to common diseases. Nat Genet 40:695–701
Altshuler D, Daly MJ, Lander ES (2008) Genetic mapping in human disease. Science 322:881–888
Fu M, Lui VC, Sham MH, Pachnis V, Tam PK (2004) Sonic Hedgehog regulates the proliferation, differentiation and migration of enteric neural crest cells in gut. J Cell Biol 166(5):673–684
Ngan ES, Lee KY, Sit FY, Poon HC, Chan JK, Sham MH, Lui VC, Tam PK (2007) Prokineticin-1 modulates proliferation and differentiation of enteric neural crest cells. Biochim Biophys Acta 1773(4):536–545
Acknowledgments
The authors would like to acknowledge the research grants HKU 765407M and HKU 775907M from the Hong Kong Research Grants Council to MGB and PT, respectively.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tam, P.K.H., Garcia-Barceló, M. Genetic basis of Hirschsprung’s disease. Pediatr Surg Int 25, 543–558 (2009). https://doi.org/10.1007/s00383-009-2402-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-009-2402-2