Abstract
Purpose
Elevated intra-abdominal pressure (IAP) has been shown to reduce mesenteric blood flow and cause intestinal damage. The purpose of the present study was to evaluate the effects of IAP and hyperoxia on superior mesenteric artery (SMA) blood flow, enterocyte proliferation and apoptosis in a rat model of abdominal compartment syndrome (ACS).
Methods
Male rats underwent midline laparotomy. SMA was isolated and ultrasonic blood flow probes were placed on the vessel for continuous measurement of regional blood flow. Two catheters were introduced into the peritoneal cavity for inflation of air and for measurement of IAP. Rats were divided into three experimental groups: (1) Sham rats were subjected to IAP of 0 mmHg, (2) ACS-air rats were subjected to IAP of 6 mmHg for 2 h and were ventilated with air, and (3) ACS-O2 rats were subjected to IAP of 6 mmHg and were ventilated with 100% oxygen (O2) during the operation and for 6 h after the operation. Intestinal structural changes, enterocyte proliferation and enterocyte apoptosis were evaluated at 24 h after operation. A paired Student’s t test and the non-parametric Kruskal–Wallis ANOVA test were used as indicated. P < 0.05 was considered statistically significant.
Results
IAP at 6 mmHg caused a moderate decrease in SMA blood flow. Inhalation of 100% oxygen resulted in a trend toward an increase in SMA flow when compared to air-ventilated animals. ACS rats demonstrated a significantly lower index of proliferation in jejunum and ileum as well as a significantly greater apoptotic index in jejunum compared to sham animals. Exposure to 100% oxygen resulted in a significant increase in cell proliferation in jejunum and ileum as well as in a significant decrease in cell apoptosis in jejunum compared to air-breathing animals.
Conclusions
In a rat model of ACS, elevated IAP decreases SMA blood flow and inhibits enterocyte turnover. Hyperoxia results in a trend toward an increase in SMA blood flow, increases enterocyte proliferation and inhibits cell death via apoptosis. These findings may have significant implications for ventilation strategies during laparoscopy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term abdominal compartment syndrome (ACS) refers to the elevated intra-abdominal pressure (IAP), which adversely impact pulmonary, cardiovascular, renal, splanchnic, musculoskeletal and central nervous system physiology [1]. The mechanisms that link elevated IAP with organ derangement are not yet completely understood.
Impaired intestinal function is one of the most consistently described organ dysfunctions associated with ACS. The effects of elevated IAP on the small intestine seem to be multifactorial in their etiology. Splanchnic flow is decreased significantly because of elevated IAP or decreased cardiac output [2, 3]. Increased IAP has a direct mechanical effect on the blood supply of the intra-abdominal organs, most convincingly seen in the kidney and intestine. Some of the deleterious effects may be associated with direct compression of the organ itself. Finally, hormonal changes have been implicated as well [1]. Pathophysiological effects include, release of cytokines, formation of oxygen free radicals, and decreased cellular production of adenosine triphosphate [4]. These processes may lead to translocation of bacteria from the gut and intestinal edema, predisposing patients to multiorgan dysfunction syndrome and death. While changes in visceral perfusion with elevated IAP have been well documented, there are little data available on morphologic changes in the small bowel due to the ACS. Diebel et al. [5] demonstrated that increased IAP can cause severe intestinal ischemia in animals. The authors speculated that intestinal ischemia may be more important than the cardiac, pulmonary, and renal changes. We have previously demonstrated that persistently elevated IAP at 15 and 25 mmHg results in a gut mucosal injury, manifested by mucosal hypoplasia, and an increase in bacterial translocation in the rat [6]. We have also shown that elevated IAP at 6 mmHg results in a moderate decrease in superior mesenteric artery (SMA) blood flow [7]. It should be emphasized that reduced splanchnic blood flow may cause histologic intestinal damage during an extended laparoscopic procedure. We have also shown a subsequent gradual increase in SMA blood flow when the abdomen was gradually decompressed. We hypothesize that abdominal deflation may cause a reperfusion injury in previously ischemic bowel, which may be augmented in patients ventilated with high oxygen concentrations.
The purpose of the present study was to evaluate the effects of elevated IAP and hyperoxia on blood flow in the SMA, on microscopic changes in the gut, on enterocyte proliferation and on apoptosis in a rat model of ACS.
Materials and methods
Animals
All procedures were approved by the Institutional Animal Care and Use Committee (Rappaport Faculty of Medicine, Technion, Haifa, Israel). Briefly, male Sprague-Dawley rats weighing 260–280 g were kept in individual stainless steel cages and were acclimatized to standard conditions of room temperature, light-dark cycles, and feeding schedules for 5 days.
Experimental design
First experiment
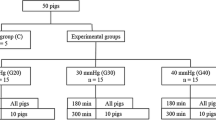
After overnight fasting, the animals were anesthetized by intraperitoneal injection of ketamine (90 mg/kg) and xylasine (13 mg/kg). The trachea was exposed and cannulated with a polyethylene catheter (PE-240) to ensure an open airway. Polyethylene catheters (PE-50) were introduced into the right carotid artery for measurements of blood pressure. Arterial pressure was recorded using a calibrated pressure transducer. After a midline laparotomy, the SMA was isolated and an ultrasonic blood flow probe (Transonic, Ithaca, USA) was placed on the SMA for continuous monitoring of regional blood flow. Two large-caliber percutaneous peripheral intravenous catheters were introduced into the peritoneal cavity for inflation of air and for measurement of IAP, and the abdominal cavity was then closed. The first catheter was connected to a multichannel recorder (CyberAmp 380, Axon Instruments, Foster City, CA), and using a PDCR75 pressure transducer (Cobe CDX III, Argon, Athens, TX), intraabdominal pressure was recorded. Slow insufflation with CO2 was applied until IAP reached 6 mmHg. The relationship between IAP and SMA blood flow was determined. At the end of the experiment, the rats were killed by open pneumothorax.
Second experiment
Two large-caliber percutaneous peripheral intravenous catheters were introduced into the peritoneal cavity without laparotomy. Through the first catheter, the abdomen was slowly insufflated with CO2 until IAP, measured through the second catheter, reached 6 mmHg. During the next 2 h, gas was either added or removed, to keep the IAP at 6 ± 0.5 mmHg. After 2 h at an IAP of 6 mmHg, the abdomen was passively decompressed and the animal allowed to stabilize at normal conditions. The animal’s temperature was kept constant at 36–37°C with a heating blanket and thermal pad.
Animals were randomly assigned to one of three experimental groups: (1) Sham rats (Group A, n = 8) underwent intraperitoneal insertion of percutaneous peripheral intravenous catheter, but no gas was pumped into the peritoneal cavity (IAP was recorded as 0 mmHg); (2) ACS-Air rats (Group B, n = 8) underwent the same procedure and CO2 was insufflated intraperitoneally to a pressure of 6 mmHg for 2 h, and (3) ACS-O2 rats underwent ACS similar to Group B and were treated with inhalation of 100% oxygen during the operation and for 6 h after operation. (Group C, n = 8).
In both experiments, oxygen (100%) was supplied by a mask-type device around the trachea (first experiment) or nose (second experiment) at a constant flow of 4 l/min. The protocol simulates a realistic sequence of events similar to a prolonged laparoscopic operation in humans when the patient is ventilated with oxygen during CO2 pneumoperitoneum and after abdominal decompression. However, in order to assess the “pure” effects of oxygen, no other resuscitative measures were undertaken.
Intestinal morphology analysis
On the morning of the next day, animals were anesthetized with I.P. sodium pentobarbital (745 mg/kg) and killed by inducing an open pneumothorax. The small intestine was removed and divided into two segments: proximal jejunum (10 cm from Treitz ligament) and terminal ileum (10 cm from ileo-cecal junction). Each segment was washed with ice-cold saline, dried and weighed. For each segment, overall bowel weight was calculated per cm of bowel length. The segments were opened lengthwise, the bowel circumference was measured at three equidistant places and mean circumference was calculated. Mucosa was scraped off and weighed.
Histological sections were prepared from the jejunal and ileal remnants. Samples of proximal jejunum and terminal ileum close to the ileo-cecal junction were placed in 5% phosphate-buffered formalin, washed with absolute alcohol, and embedded in paraffin, cut to 5 μm thickness, and stained with hematoxylin–eosin. Five longest villi and crypts were selected for the microscopic analysis, using a 10 × 4 magnifying lens. Histological images were loaded on a 760 × 570 pixels resolution buffer using a computerized image analysis system composed of a trichip RGB video-camera (Sony, Japan), installed on a light microscope (Zeiss, Germany) and attached to an IBM compatible personal computer (Pentium III, MMX, 450 mhz, 125 MB RAM), equipped with a frame grabber. Images were captured, digitized and displayed on a high-resolution monitor. The villous height and crypt depth were measured using the Image Pro Plus 4 image analysis software (Media Cybernetics, Baltimore, Maryland, USA).
The degree of intestinal tissue injury was evaluated on a grading scale from 0 to 8 as described previously by Park et al. [8]: 0—normal mucosa, 1—subepithelial space at villus tip, 2—more extended subepithelial space, 3—epithelial lifting along villus sides, 4—denuded villi, 5—loss of villus tissue, 6—crypt layer infarction, 7—transmucosal infarction, 8—transmural infarction.
Enterocyte proliferation and apoptosis
To determine enterocyte proliferation, rats were injected with standard 5-bromodeoxyuridine (5-BrdU) labeling reagent (Zymed Lab, Inc, CA) at a dose of 1 ml per 100 g body weight, 90 min before sacrifice. Paraffin-embedded slices (5 μm) were deparaffinized with xylene, rehydrated with graded alcohol, and stained with a biotinylated monoclonal anti-BrdU antibody system using the BrdU Staining Kit (Zymed Lab, Inc, CA). An index of proliferation was determined as the ratio of crypt cells staining positively for BrdU per ten crypts.
Apoptotic cells were identified using immunohistochemical analysis for caspase 3. Caspase 3 (CPP32/YAMA) is a marker for the early apoptotic phase. Paraffin-embedded sections (5 μm) were dewaxed and rehydrated with xylene and graded alcohol. Tissue sections were microwave-pretreated in 10 mM citrate buffer (pH 6.0). Immunohistochemical analysis for caspase-3 was performed using the streptavidin–biotin–peroxidase method according to the manufacturers’ protocols. After the blocking of endogenous biotin activity, tissue sections were incubated with primary antibodies (Caspase-3 cleaved concentrated polyclonal antibody; dilution 1:100; Biocare Medical, Walnut Greek, CA) for 1 h at room temperature, followed by incubation with secondary antibodies (human-absorbed, biotinylated, affinity-purified antibody) for 20 min. The DAB was used to create an intense brown deposit around the antigen–antibody–enzyme complex in the sample. For each group, the number of stained cells was counted in two bowel cross sections. The apoptotic index (AI) was defined as the number of apoptotic cells per ten villi.
Statistical analysis
The data are expressed as the mean ± SEM. A paired Student’s t test and the non-parametric Kruskal–Wallis ANOVA test were used as indicted. P < 0.05 was considered statistically significant.
Results
First experiment
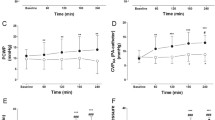
The effect of increased IAP on SMA blood flow in air breathing and 100% oxygen treated rats is summarized in Fig. 1. Elevated IAP resulted in decreased SMA blood flow compared to baseline levels. As expected, IAP at 6 mmHg caused a 18% decrease in SMA blood flow (P < 0.05) with subsequent gradual increase when the abdomen was gradually decompressed to values not significantly different from those before abdominal insufflation. Inhalation of 100% oxygen did not prevent the decline in SMA blood flow, but kept SMA blood flow at higher levels compared to air-breathing animals.
Second experiment
Intestinal mucosal parameters
ACS-Air rats (Group B) showed a significantly lower bowel weight in jejunum (26%, P < 0.05) and ileum (17%, P < 0.05) as well as mucosal weight in jejunum (33%, P < 0.05) and in ileum (28%, P < 0.05) compared to sham animals (Group A) 24 h after insufflation (Fig 2). Inhalation of 100% oxygen (Group C) resulted in a significant increase in bowel weight in jejunum (14%, P < 0.05), as well as mucosal weight in jejunum (31% increase, P < 0.05) and ileum (28% increase, P < 0.05) compared to air-breathing animals (Group B).
Microscopic mucosal parameters
The jejunum and the ileum of sham animals exhibited normal mucosal architecture. Neither abdominal insufflations (Group B) nor inhalation of 100% oxygen (Group C) changed intestinal injury grade significantly compared to sham animals (Group A) (Fig. 3). ACS-air rats (Group B) demonstrated a significant decrease in villous height in the jejunum (24%, P < 0.05) and ileum (23%, P < 0.05) compared to sham animals (Group A) (Fig. 4). Although oxygen treated rats (Group C) showed a trend toward a decrease in villous height in the jejunum and ileum, this trend did not achieve statistical significance.
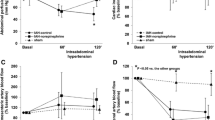
Enterocyte proliferation and apoptosis
ACS-Air rats (Group B) demonstrated a significant decrease in the enterocyte proliferation index in jejunum (104 ± 7 vs. 132 ± 6 BrdU positive cells/10 crypts, P < 0.05) and ileum (1134 ± 10 vs. 138 ± 4 BrdU positive cells/10 crypts, P < 0.05) compared to sham animals (Fig. 5). Inhalation of 100% oxygen (Group C) induced a significant increase in the proliferation index in jejunum (138 ± 11 vs. 104 ± 7 BrdU positive cells/10 crypts, P < 0.05) and ileum (133 ± 9 vs. 113 ± 10 BrdU positive cells/10 crypts, P < 0.05) compared to air-breathing animals (Group B).
Effect of elevated IAP and hyperoxia on enterocyte proliferation and apoptosis. 5-BrdU incorporation into proliferating cells was detected with a goat anti-BrdU antibody. Apoptotic cells were identified using immunohistochemical analysis for caspase 3. Values are mean ± SEM. IAP intra-abdominal pressure, ACS abdominal compartment syndrome, O2-oxygen. * P < 0.05 ACS vs Sham rats, † P < 0.05 ACS-O2 versus ACS-air rats
ACS (Group B) resulted in a significantly greater number of apoptotic cells appearing in the villi of jejunum (2.6 ± 0.6 vs. 0.6 ± 0.1 caspase-3 positive cells/10 villi, P < 0.05) and ileum (3.4 ± 0.7 vs. 1.4 ± 0.4 caspase-3 positive cells/10 villi, P < 0.05) compared to sham animals. Inhalation of 100% oxygen (Group C) led to a significant decrease (vs. ACS-Air) in AI in jejunum (1.1 ± 0.2 vs. 2.6 ± 0.6 caspase-3 positive cells/10 villi, P < 0.05) and a trend toward decrease in AI in ileum; however, this trend was not statistically significant.
Discussion
Small bowel ischemia following laparoscopy was described recently as a rare fatal complication of the CO2 pneumoperitoneum [9]. Andrei et al. reviewed the literature on small bowel ischemia at 1999. Their review yielded five cases following laparoscopic cholecystectomy and one case after laparoscopic Nissen fundoplication [10]. These authors also reported a personal communication of another case after laparoscopic cholecystectomy. Hassan et al. [9] described the first case of intestinal ischemia following a gynecological procedure.
The CO2 pneumoperitoneum is a predisposing factor for intestinal ischemia. The effects of elevated IAP on small intestine seem to be multifactorial in their etiology. ACS compromises the mesenteric circulation through decreased cardiac output and mechanical reduction of the blood flow due to elevated IAP, and humoral vasoconstriction [1–5]. The elevation of systemic vascular resistance is a combined effect of arteriolar vasoconstriction and elevated IAP. It is widely accepted that the intestinal mucosa is highly sensitive to various systemic and regional factors associated with ischemia. In a recent experiment, Duzgun et al. have shown that elevated IAP (15, 20, and 25 mmHg) results in elevated serum d-lactate levels that directly correlate with IAP levels. Histological examinations of the intestinal tissue samples showed no significant pathologic changes concordant with intestinal ischemia [11]. In a recent study, Doty et al. [12] have demonstrated that hemorrhage followed by reperfusion and a subsequent insult of IAP caused significant gastrointestinal mucosal acidosis due to hypoperfusion. We have recently shown that elevated IAP at 15 and 25 mmHg in rats results in mucosal injury of the gut, causing mucosal hypoplasia and increases bacterial translocation [6].
In addition to the damage caused by decreased splanchnic blood flow and concomitant hypoxia, abdominal deflation at the end of an episode of IAP provides a model of reperfusion in previously ischemic bowel. Production of oxygen-derived free radicals may aggravate intestinal tissue injury caused by ischemia following elevated IAP. Pathophysiologic effects of ischemia and reperfusion of the bowel include, release of cytokines, formation of oxygen free radicals, and decreased cellular production of adenosine triphosphate. Eleftheriadis et al. [4] have shown that IAP at 15 mmHg led to increased free radical production in the intestinal mucosa and increased bacterial translocation. The authors have hypothesized that abdominal deflation at the end of a laparoscopic procedure provides a model of reperfusion in previously ischemic organs. In this context, production of oxygen-derived free radicals may aggravate intestinal injury caused by ischemia following elevated IAP, especially in patients ventilated with high oxygen concentrations.
In the present study, we evaluated the consequences of increased IAP and hyperoxia on SMA blood flow because of their potential relationship with intestinal damage following extended laparoscopic procedures. One must keep in mind that clinical laparoscopy generally requires lower levels of pneumoperitoneum than were used in our previous animal study [6]. Therefore, in the current study the maximal level of 6 mmHg was chosen.
In the current study, we have shown that elevated IAP resulted in a mild but significant decrease in SMA blood flow that correlated with the levels of IAP. IAP at 6 mmHg resulted in a significant 18% decrease in SMA blood flow compared to a baseline levels with a subsequent gradual increase when the abdomen was gradually decompressed to values not significantly different from those before abdominal insufflations. Our observations are consistent with the data of other investigators who found a mild decrease in splanchnic blood flow in animals with ACS. Classically, elevation in IAP leads to a reduction in cardiac output because of decreased inferior vena cava flow secondary to direct compression as well as decreased superior vena cava flow caused by increased thoracic pressure [13, 14]. The inhalation of 100% oxygen did not prevent the decline in SMA blood flow, but kept the SMA blood flow at higher levels compared to air-breathing animals.
Since arterial blood supply to the gut decreases in parallel with elevated IAP, we investigated, in the second experiment, the effect of extended modest increases in IAP (6 mmHg) and hyperoxia on intestinal structure and turnover in a rat. Our data suggest that increasing IAP did not cause direct gut injury. This conclusion is supported by the observed unchanged degree of tissue injury (Park’s criteria). Nevertheless, the observed decrease in SMA blood flow circulation was accompanied by intestinal mucosal hypoplasia. This is evident from decreased bowel and mucosal weight in ACS rats compared to sham animals. Histologically, changes in villous height, a close correlate of cell number were observed in direct proportion to decreased mucosal weight. This study does not address the possible association between impaired structure and altered function. However, in our conventional thinking of intestinal function, it is assumed that a decrease in villous height is accompanied by impaired nutrient absorption.
Decreased splanchnic circulation in ACS rats was accompanied by decreased cell proliferation and increased cell apoptosis in both jejunum and ileum compared to control animals. Both mechanisms may be responsible for decreased cell mass. The loss of small intestinal epithelial cells leading to villous atrophy has been well described in various experimental models [15–17]. Growing evidence suggests that cell apoptosis plays a crucial role in this process. Our data showed that programmed cell death is one of the pathways leading to mucosal damage as well as to marked mucosal atrophy observed in half of the animals following abdominal insufflations. Both decreased cell proliferation and increased cell apoptosis suggest decreased enterocyte turnover, which might explain mucosal hypoplasia in ACS animals.
Treatment with 100% oxygen did not significantly change the intestinal injury score compared to air-breathing animals. Additionally, oxygen-treated rats showed a less marked decrease in SMA flow compared to air-breathing animals, suggesting better splanchnic circulation. These changes were accompanied by increased bowel and mucosal weight as well as increased villus height, which represent accelerated intestinal mucosal repair and enhanced enterocyte turnover. Treatment with hyperoxia led to a rapid increase in the uptake of bromdioxyuridine (BrdU) and the size of the proliferative compartment in the crypt. We would hypothesize that after exposure to hyperoxia, an abnormally “rich” supply of oxygen to the enterocytes might directly stimulate mucosal hyperplasia. The increased oxygen supply may also stimulate the release and circulation of enteric hormones, which have trophic effects on small bowel mucosa. Increased cell proliferation rate was accompanied by an increase in villous height, suggesting an increased absorptive surface area. This change was accompanied by decreased cell apoptosis compared to air-breathing rats. The specific mechanism for the apparent anti-apoptotic effects of hyperoxia has not yet been fully elucidated. Hyperoxia may possibly attenuate the enterocyte injury that precedes apoptosis, possibly as a membrane stabilizer, thereby acting in situ on mitochondria to prevent the release of cytochrome c and subsequent caspase activation, thus preventing or delaying the initiation of the apoptotic cascade. Alternatively, oxygen may act intracellularly to alter the expression of genes related to apoptosis or interfere with specific caspase functions.
In conclusion, persistent IAP for 2 h results in a moderate decrease in SMA blood flow and concomitant mucosal hypoplasia. Decreased enterocyte proliferation and elevated cell apoptosis may be responsible for this effect. Treatment with hyperoxia did not exacerbate intestinal injury; in contrast, treatment with 100% oxygen accelerates enterocyte turnover in ACS rats. These findings may have significant implications for ventilation strategies during laparoscopy.
References
Lerner SM (2008) Review article: the abdominal compartment syndrome. Aliment Pharmacol Ther 28:377–384
Caldwell CB, Ricotta JJ (1987) Changes in visceral blood flow with elevated intraabdominal pressure. J Surg Res 43:14–20
Eleftheriadis E, Kotzampassi K, Papanotas K et al (1996) Gut ischemia, oxidative stress, and bacterial translocation in elevated abdominal pressuer in rats. World J Surg 20:11–16
Walker J, Criddle LM (2003) Pathophysiology and management of abdominal compartment syndrome. Am J Crit Care 12:367–371
Diebel LN, Dulchavsky SA, Wilson RF (1992) Effect of increased intra-abdominal pressure on mesenteric arterial and intestinal mucosal blood flow. J Trauma 33:45–48
Sukhotnik I, Bejar Y, Srugo I et al (2006) Adverse effect of increased intraabdominal pressure on small bowel structure and bacterial translocation in rat. J Laparoendosc Adv Surg Tech A 16:404–410
Mogilner J, Sukhotnik I, Brod V et al (2008) Effect of elevated intra-abdominal pressure on portal vein and superior mesenteric artery blood flow in a rat. 17th Annual Congress of Endosurgery in Children, Cannes, France
Park PO, Haglund U, Bulkley GB et al (1990) The sequence of development of intestinal tissue injury after strangulation ischemia and reperfusion. Surgery 107:574–580
Hasson HM, Galanopoulos C, Langerman A (2004) Ischemic necrosis of small bowel following laparoscopic surgery. JSLS 8:159–163
Andrei VE, Schein M, Wise L (1999) Small bowel ischemia following laparoscopic cholecystectomy. Dig Surg 16:522–524
Duzgun AP, Gulgez B, Ozmutlu A et al (2006) The relationship between intestinal hypoperfusion and serum d-lactate levels during experimental intra-abdominal hypertension. Dig Dis Sci 51:2400–2403
Doty JM, Oda J, Ivatury RR (2002) The effects of hemodynamic shock and increased intra-abdominal pressure on bacterial translocation. J Trauma 52:13–17
Saggi BH, Sugerman HJ, Ivatury RR et al (1998) Abdominal compartment syndrome. J Trauma 45:597–609
Kashtan J, Green JF, Parson EQ (1981) Hemodynamic effects of increased abdominal pressure. J Surg Res 30:249–255
Hall PA, Coates PJ, Ansari B et al (1994) Regulation of cell number in the mammalian gastrointestinal tract: the importance of apoptosis. J Cell Sci 107:3569–3577
Sukhotnik I, Helou H, Lurie M et al (2007) The effect of leptin on intestinal recovery following ischemia-reperfusion injury in a rat. Pediatr Surg Int 23:473–478
Sukhotnik I, Shehadeh N, Coran AG et al (2008) Oral insulin enhances cell proliferation, decreases enterocyte apopotosis during methotrexate-induced mucositis in a rat. J Pediatr Gastroenterol Nutr 47:115–122
Author information
Authors and Affiliations
Corresponding author
Additional information
Igor Sukhotnik and Jorge Mogilner have equally contributed to preparation of the manuscript.
Rights and permissions
About this article
Cite this article
Sukhotnik, I., Mogilner, J., Hayari, L. et al. Effect of elevated intra-abdominal pressure and 100% oxygen on superior mesenteric artery blood flow and enterocyte turnover in a rat. Pediatr Surg Int 24, 1347–1353 (2008). https://doi.org/10.1007/s00383-008-2262-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-008-2262-1