Abstract
There are some evidence to suggest that careful antenatal monitoring, scheduled preterm delivery and immediate abdominal wall closure may reduce gastroschisis morbidity. We hypothesised that the advantages of a scheduled preterm delivery balance possible complications related to prematurity. A retrospective study was performed including all cases of gastroschisis born between 1990 and 2004 (n = 69). Cases were categorised in two groups. Group 1 contained gastroschisis cases born between 1990 and 1997. Group 2 contained cases occurring since 1997, when a new management pathway for gastroschisis was established: weekly evaluation of the foetal gut by ultrasound (>28 weeks), corticosteroids, and delivery by scheduled caesarean section at 35 weeks (before if evidence of bowel compromise was present). The primary endpoints of this study were the initiation of oral feeding and the number of re-operation for intestinal obstruction. There was a significantly faster initiation of oral feeding (P < 0.0001), however, duration of parenteral nutrition (34 vs. 38 days) and hospital discharge (53 vs. 58.5 days) was not reduced. There was no complication due to prematurity in group 2. Postoperative outcome was improved with less need for muscular stretching or prosthetic patch and less re-operation for intestinal obstruction (P < 0.05). Scheduled and elective preterm delivery facilitates surgical procedure and shortens the time to first feeding. A delivery at 35 weeks (preferring vaginal delivery) seems to be a good compromise between risks related to prematurity and complications related to intestinal peel.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gastroschisis is a rare congenital abnormality which was first described by Ambroise Paré in 1634 [1]. During the last two decades, many western countries have demonstrated an increase in the incidence of gastroschisis. In France, the incidence is currently 1.46–2.69 per 10,000 live births [2]. The mortality rate for gastroschisis is now less than 10%, but morbidity remains high, mainly due to the delayed onset of intestinal function. The mechanism of intestinal hypomotility remains incompletely understood but the presence of an inflammatory peel may be implicated. Current findings suggest that intestinal injuries occur mainly during the third trimester of pregnancy [3].
Scheduled preterm delivery is really controversial but many authors [4–7] have proved that this management may promote better outcome by reducing total parental nutrition duration, hospital length of stay and surgical complications without increased mortality or morbidity due to prematurity. The aim of our study was to evaluate the benefits of a scheduled preterm delivery to avoid bowel damage and its post-natal consequences.
Materials and methods
A retrospective study was performed including all cases of gastroschisis managed at our centre between January 1990 and January 2004 (n = 69) with at least 1 year of follow-up. Cases were categorised in two groups. Group 1 contained gastroschisis cases born between 1990 and 1997, when ultrasonographic monitoring was not strictly organised and delivery was not scheduled and occurred mainly at term. Before 1997, only three ultrasonographic controls were done during pregnancy.
Group 2 contained cases occurring since 1997, when a new management pathway for gastroschisis was established. This pathway was developed on the hypothesis that preterm delivery prevents serious gastrointestinal compromise, facilitates primary surgical closure, and improves postoperative outcome. The pathway included ultrasound evaluation of the foetal gut, maternal administration of corticosteroids (double maternal dose of 20 mg of betamethasone), and delivery at 35 weeks by scheduled elective caesarean section (CS) if necessary. During the second trimester, ultrasonographies were performed monthly and after 28 weeks of pregnancy, weekly evaluation was done. Multiple ultrasonographic parameters were studied: maximum bowel inner diameter, bowel wall thickness, bowel dilatation progression, gastric dilatation, umbilical cord and mesenteric artery Doppler, bowel motility, parietal defect size and foetal growth parameters. If the bowel status worsens (progression of dilatation, bowel diameter upper than 18 mm, Doppler anomalies, gastric dilatation, absence of bowel movements…) an other ultrasonography was performed 2 or 3 days later. Therefore, if necessary, a multidisciplinary (obstetrician, surgeon and neonatologist) decision of rapid delivery was taken. Earlier delivery was also performed for foetal (worsening foetal status) or maternal indications. For groups 1 and 2, the surgical management was similar, with an attempt of primary abdominal wall closure.
Neonates were received by the neonatologist immediately after delivery. Initial management included rapid physical assessment, placement of the distal part of the neonate in a sterile bowel bag to prevent hypothermia and dehydration. The neonate was then placed in the right lateral position to prevent venous engorgement, a nasogastric tube was inserted and intravenous fluid perfusion was started. They were then transported to the operative room where general anaesthesia and endotracheal intubation were performed. The time between birth and surgery was shortened as soon as possible. Peak inspiratory pressure and lower limb oxygen saturation were followed throughout the surgical procedure. After draping, bowel loops were inspected and meconium was evacuated manually from the colon. Bowel loops were reduced into the abdomen without extending the abdominal wall defect. Fascia was separated from the skin and repaired transversally with a non-absorbable suture. If complications occurred during the procedure such as a decrease in lower limb oxygen saturation or a significant reduction in pulmonary compliance necessitating an increase in peak inspiratory pressure, other procedures were performed:
-
the parietal defect was extended, abdominal stretching was performed and the abdominal wall was closed, using a Gore-Tex® patch [8],
-
if reduction was impossible due to persistently high intra-abdominal pressure, a staged repair was performed using the silo technique.
The measures collected to compare the two groups were maternal age, gestational age at diagnosis and at delivery, foetal sex, mode of delivery (vaginal vs. CS), birth weight, bowel aspect at birth, size of abdominal wall defect, associated extra-intestinal anomalies, type of closure (primary vs. staged repair), incidences of complications and mortality rates, time to first feeding, duration of total parenteral nutrition and length of hospital stay.
Inflammatory peel was graded as absent, moderate or thick. “Thick” peel was noted if intestinal wall was thickened, inflammatory and rigid and if fibrinous peel was abundant. “Moderate” peel was an intermediate steps between “absent” and “thick” peel (presence of few fibrinous membranes). This subjective gradation was based on the operative reports.
Complex gastroschisis was defined as that associated with intestinal complications such as intestinal atresia, perforations, necrotic segments, and volvulus.
Group 1 (1990–1996) and group 2 (1997–2004) were compared using the Student’s t test.
Results
Patients
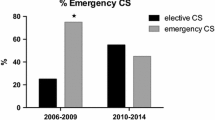
A total of 69 infants were treated between 1990 and 2004; 43 boys and 26 girls. The average maternal age was 26.3 years. Prenatal diagnosis was not done for five patients, all in group 1 (7%). Mean gestational age at the time of the diagnosis was 21.8 ± 6.7 weeks (range, 11–37 weeks). A total of 61 infants were delivered by caesarean section (90%). Intrauterine growth retardation was frequent as shown in Table 1. In group 2, 23 babies (64%) were delivered before 35 weeks of gestation: in 6 cases for premature membrane rupture, in 1 case for preterm labour, in 5 cases for foetal heart rate anomalies and in 2 cases for intrauterine growth retardation. For the other cases, bowel status worsened leading to CS before 35 weeks of gestation. Neonatal distress was diagnosed in nine cases. There was a reduction in neonatal distress rates with scheduled delivery compared to non-scheduled delivery (3 vs. 23%, P = 0.06).
A total of 68% of exposed abdominal contents constituted bowel only; other organs exposed included stomach (24.2%), gonads (13%), bladder (2.9%), gallbladder (2.9%) and pylorus (1.4%). Mean abdominal wall defect diameter was 21 ± 8.7 mm (range, 7–40 mm).
Complex gastroschisis occurred in eight cases (6 intestinal atresias and 2 volvulus): four in group 1 and four in group 2 (non-significant difference). Outcome was worse for complex cases as shown in Table 2. Defect size was also smaller for complex gastroschisis in comparison with isolated gastroschisis (23 vs. 12 mm).
Four patients (5.8%) died. The reasons for death were polymalformative syndrome (trisomy 13), total bowel necrosis, multiple atresias, and severe iatrogenic hydro-electrolytic disorders due to parenteral nutrition. Other complications are listed in Table 3.
Impact of period of treatment on patient outcome
The effects of period of treatment on patient outcome are summarised in Table 4. A total of 33 patients were treated between 1990 and 1996 (group 1), and 36 between 1997 and 2004 (group 2). As expected, group 2 patients had a significantly lower birth weight than in group 1 (1.94 ± 0.48 vs. 2.46 ± 0.56 kg, respectively, P < 0.001) due to preterm delivery. However, intrauterine growth retardation was less frequent for children born preterm compared to children born at term. Birth weight for gestational age was below the 10th percentile in 15% of children born before 34 weeks of gestation, and 48% of children born after 37 weeks of gestation (cf. Table 1). Groups were similar with respect to maternal age, sex and associated anomalies (data not shown). Severity of inflammatory peel was significantly reduced in group 2: thick peel occurred in 44% of cases in group 1, compared to 6% in group 2 (P < 0.001).
Primary closure was achieved in 88% in group 1 and 95% in group 2 (non-significant difference). The surgery was easily performed in group 2, with less need for abdominal stretching or a prosthetic patch (Table 4). Re-operation rate for bowel obstruction was reduced in group 2 compared to group 1 (19 and 42%, respectively).
Patients were discharged from the hospital when they were gaining weight and tolerating feeds. The time until first feeding was significantly earlier in group 2 (13.5 days) compared to group 1 (25.5 days). However, the duration of parenteral feeding and length of hospital stay were similar in both groups (Table 4). Rates of medical complications were 45% in group 1 and 64% in group 2, a non-significant difference. There were no complications due to prematurity in group 2 (pulmonary, neurological or digestive).
Discussion
Prevalence of gastroschisis is increasing [9] and is currently diagnosed predominantly in utero. However, there is no consensus in optimal management of antenatally diagnosed gastroschisis. Controversies persist in the method, the site and the gestational age at delivery [10]. Consensus has not been reached on the time to surgery [11] and the benefit of primary versus staged repair [12]. Therefore, we systematically propose antenatal parental counselling to explain perinatal management of gastroschisis. This counselling should be multidisciplinary involving the paediatric surgeon, obstetrician, neonatologist and ultrasonographist. Counselling may reduce parental anxiety [13] and permit a dialogue between members of the multidisciplinary team.
The main complications for patients with gastroschisis are: increased intra-abdominal pressure, post-operative bowel hypomotility and necrotising enterocolitis. In 1953, Moore [14] was the first to report the inflammatory “peel” associated with gastroschisis. The pathophysiology of intestinal injuries in gastroschisis is still unknown. Intestinal damage and particularly peel formation, in gastroschisis may be attributed to digestive [15, 16] or urinary [17, 18] wastes in amniotic fluid. Many paediatric surgeons believe that the prolonged contact of exposed bowel to amniotic fluid increases intestinal lesions (hyperplasia and hypertrophy of smooth muscle cells, submucosal collagen accumulation…) and results in prolonged intestinal dysfunction [19]. These lesions have been thought to lead to an increased intra-abdominal pressure which is putatively responsible for complications, surgical difficulties and mortality [20]. Mesenteric ischaemia due to inflammatory peel or to stricture may also contribute to foetal intestinal injuries [17, 21]. Tibboel et al. [22] demonstrated that histological changes occur late in gestation, after 30 weeks. So, we hypothesised that preterm delivery with early repair may limit the period of intrauterine damage and may improve outcome. We decided to perform a weekly bowel evaluation by high-resolution ultrasound after 28 weeks of gestation. Scheduled delivery was performed at 35 weeks or before this time if evidence of bowel compromise was present. In our study, intra-abdominal (intravesical or intragastric) pressure was not monitored systematically. We decided to perform abdominal wall stretching, abdominal prosthetic patch or delayed closure if low limbs saturation decreased or ventilation pressure rose. We agree that the decision to perform primary or delayed closure depend mainly on surgeon and anaesthesiologist experience. On the other hand, small size defect has been thought to lead to intestinal lesions [17, 20]. Intestinal ischaemia caused by constriction may induce atresia or bowel necrosis. Our study is in agreement with the hypothesis that abdominal wall defect in “complex gastroschisis” have a defect wall diameter smaller than isolated gastroschisis. Moreover, the results of our study suggest that cases of “complex gastroschisis” suffer a worse prognosis than non-complex cases. Of the eight patients who had complex gastroschisis, 63% required intestinal derivation (versus 0% for non-complex gastroschisis), length of hospital stay was longer, re-operation rate was more frequent and mortality rate was dramatically increased. This is in concordance with Molik et al. report [23].
Several studies have previously examined the role of elective preterm delivery in gastroschisis, but few of these have studied a scheduled birth at 35 weeks of gestation. We choose a delivery at this time because it could be a good compromise between risks of intestinal lesions and morbidity related to preterm birth. Indeed, mortality and morbidity due to prematurity (pulmonary bronchodysplasia, intracerebral haemorrhage, retinopathy…) is less frequent after 32 weeks of gestation [24]. In our study, mean time to delivery was 33.5 weeks of gestation while we choose a delivery at 35 weeks. This difference could be explained by babies delivered before 35 weeks of gestation for foetal or maternal reasons or for worsened aspect of the bowel. Our management did not increase complications due to prematurity, length of hospital stay or mortality rate. In our patient population, medical and surgical complications are in agreement with the literature [20, 25]. More than half of the patients developed non-surgical complications during their hospital stay. On the other hand, preterm delivery remains controversial. For many authors [26], early delivery increases morbidity (medical complications, staged repair rate, length of hospital stay), cost of hospitalisation and mortality [3]. In a study of 354 infants born with gastroschisis, Salihu et al. [11] demonstrate that infants who were born preterm (<37 weeks of gestation) were more than three times as likely to die in the neonatal period as their counterparts who were born at term. In a recent randomised controlled trial of elective preterm delivery, Logghe et al. [27] demonstrated that there was no significant benefit from this management. However, in 1999, Moore et al. [28] proposed a preterm and particularly a prelabour CS to reduce peel formation and avoid complications of gastroschisis. Many authors [4–7] proposed that elective preterm delivery (before 35–38 weeks of gestation) using specific ultrasound criteria resulted in improved postoperative outcome without significant morbidity secondary to prematurity (pulmonary, digestive, neurological). Recently, Serra et al. [7] reported a faster initiation of enteral feeding, a shorter hospital stay with an excellent postoperative outcome. On the other hand, in these studies late complications due to prematurity as Attention Deficit Hyperactivity Disorders or retinopathy were not considered.
In our report, severity of intestinal peel was significantly reduced for patients born after preterm scheduled CS. Moreover, we demonstrate that perinatal management of infants with gastroschisis in group 2 facilitates surgical performance and decrease rates of early surgical complications. The need for abdominal stretching or use of a prosthetic patch was reduced in group 2. We could hypothesise that reduction of peel severity facilitates surgical performance. Moreover, re-operation for adhesive bowel obstruction was less frequent with scheduled preterm delivery, we hypothesised that inflammatory aspect of bowel due to thick peel bowel or more frequent adhesion secondary to the use of prosthetic patch may induce more bowel obstruction.
Many controversies exist regarding the choice between primary and delay closure of the abdominal wall. If primary closure can be done without tension, some authors have shown that infectious complications, TPN duration and hospital duration stay decreased in comparison with delayed closure [12, 20, 29]. One the other hand, some authors [27, 30] have proposed routine insertion of preformed spring-loaded silo and delayed closure with good results. Bianchi et al. [31] have also proposed primary closure without anaesthesia in selected patients. We thought that our management could permit an easier reduction with a bowel supple and free of peel and should already facilitate delayed closure.
In group 2 (1997–2004), the mean time to first feeding obtained in our study is in agreement with reported ranges (13.5 vs. 14–21 days[32]) whereas it was more than 25 days in group 1 (1990–1996). In line with Eggink et al.’s [32] study in 2006, our study showed a strong trend for infants born later than 37 weeks to start feeding later. This is in concordance with the previous hypothesis that prolonged exposure of bowel to amniotic fluid may impair absorption and/or motility of the gut [33]. On the other hand, this difference could be explained by the changes of practice; surgeons choose to start feed earlier; rather than suggesting an advantage of the timing and mode of delivery. In our study, preterm delivery did not improve outcome regarding parenteral feeding duration or length of hospital stay. Median length of hospital stay is still high at 55 days, but this is still within the mean range of 25–92 days reported by other studies [30, 34]. We accept that our prenatal and postnatal management did not decrease duration of TPN, length of hospital stay or rate of medical complications in comparison with literature. On the other hand, surgery was easily performed, bowel obstruction was less frequent and length of hospital stay was similar for patients born at term and patients born before 35 weeks of gestation.
In our study, scheduled CS was preferred because this allowed the medical team to be ready to receive the newborn with gastroschisis and postnatal management could be achieved quickly. Controversies regarding time between delivery and surgery exist. For many surgeons, time between delivery and surgical repair have to be reduced as soon as possible to provide good outcome [35, 36] by reducing bowel oedema and facilitating reintegration. Some studies focused on a delayed surgery, there were no difference (concerning morbidity, mortality, TPN duration) for newborn treated before or after 6–7 h [10, 37] (which is not a really long delay).
Caesarean section rate was high in group 1 (up to 90%) because until the end of the 1990s it was thought that vaginal delivery should be deleterious on exteriorised bowel. It has been reported that uterine contraction and vaginal delivery can induce intestinal lesions and intestinal rupture [38]. On the other hand, CS may protect the bowel from dystocia, traumatism and microbial contamination [28, 39–43]. Recently, a meta-analysis by Segel et al. [44] found that there was no significant relationship between mode of delivery and the rate of primary fascial repair, neonatal sepsis or paediatric mortality. Additionally, there was no significant relationship between mode of delivery and time until enteral feeding or length of hospital stay. In our report, we focused on newborn outcome but we did not studied mother’s morbidity or mortality due to CS. We recognise that a prior CS may compromise future pregnancies with a greater risk of uterine rupture, endometriosis and increased need for blood transfusion [45]. However, induction of labour in preterm pregnancy is often inconsistent. Blackwell et al. [46] reports a rate of unsuccessful labour induction of 32% for preterm severe pre-eclamptic patients between 32 and 34 weeks. Nonetheless, we actually do not recommend CS for gastroschisis delivery and we are trying as soon as possible to induce labour.
Our study has many points of limitation. First of all, it is a retrospective study extending over more than 10 years. Improvement of outcome between groups 1 and 2 should be explained by progresses made in antenatal diagnosis, surgery, anaesthesiology, knowledge of TPN and neonatal intensive care over the past years. These modifications could lead to explain the best outcome reported in group 2. Edouard Herriot Hospital surgical team [47] reported a gastroschisis study in 1984, when the mortality rate was 32%. In our current study, between 1997 and 2004, the mortality rate was less than 3%. Moreover, choosing a preterm delivery, maternal administration of steroid was systematically used to prevent neonatal pulmonary complications in group 2 and could have resulted in an attenuation of the intestinal lesions. Using an animal model, local intra amniotic instillation of steroid has improved the intestinal lesions of gastroschisis by reducing the inflammation due to intra amniotic waste [48, 49]. On the other hand, there is actually no objective evidence that maternal administration of steroids could play a protective role. One other bias in our study is the frequent use of CS. Caesarean section could be an independent variable improving outcome. So, many factors could play a major role in this improvement and should be explored in a prospective trial.
In conclusion, our experience suggests that scheduled and elective preterm delivery facilitate surgical procedure and shorten the time to first feeding. A delivery at 35 weeks should be proposed and seems to be a good compromise between risks related to prematurity and complications related to intestinal peel. This management does not increase mortality or morbidity rates. In contrast, duration of hospital stay, duration of parenteral nutrition and complex gastroschisis rate (atresia, necrosis, volvulus) was not reduced in our study. We believe that systematic CS should be avoided but scheduled preterm birth seems to be important, so we actually recommend a vaginal delivery with induction of labour. Further research in antenatal ultrasonography to determine pertinent variables may help in developing new strategies and interventions to improve postnatal outcome of children with gastroschisis.
References
Paré A (1634) “The works of that famous surgeon.” Th. Cotes & R. Young, London
Stoll C, Alembik Y, Dott B, Roth MP (2001) Risk factors in congenital abdominal wall defects (omphalocele and gastroschisis): a study in a series of 265,858 consecutive births. Ann Genet 44:201–208
Ergun O, Barksdale E, Ergun FS et al (2005) The timing of delivery of infants with gastroschisis influences outcome. J Pediatr Surg 40:424–428 1999,15:97–104
Peiro JL, Guindos S, Lloret J et al (2005) New surgical strategy in gastroschisis: treatment simplification according to its physiopathology. Cir Pediatr 18:182–187
Vegunta RK, Wallace LJ, Leonardi MR et al (2005) Perinatal management of gastroschisis: analysis of a newly established clinical pathway. J Pediatr Surg 40:528–534
Moir CR, Ramsey PS, Ogburn PL et al (2004) A prospective trial of elective preterm delivery for fetal gastroschisis. Am J Perinatol 21:289–294
Serra A, Fitze G, Kamin G et al (2008) Preliminary report on elective preterm delivery at 34 weeks and primary abdominal closure for the management of gastroschisis. Eur J Pediatr Surg 18(1):32–37
Stringel G (1993) Large gastroschisis: primary repair with Gore-Tex patch. J Pediatr Surg 28:653–655
Laughon M, Meyer R, Bose C et al (2003) Rising birth prevalence of gastroschisis. J Perinatol 23:291–293
Singh SJ, Fraser A, Leditschke JF et al (2003) Gastroschisis: determinants of neonatal outcome. Pediatr Surg Int 19:260–265
Salihu HM, Emusu D, Aliyu ZY et al (2004) Mode of delivery and neonatal survival of infants with isolated gastroschisis. Obstet Gynecol 104:678–683
Puri A, Bajpai M (1999) Gastroschisis and omphalocele. Indian J Pediatr 66:773–789
Kemp J, Davenport M, Pernet A (1998) Antenatally diagnosed surgical anomalies: the psychological effect of parental antenatal counseling. J Pediatr Surg 33:1376–1379
Moore TC, Stokes GE (1953) Gastroschisis; report of two cases treated by a modification of the gross operation for omphalocele. Surgery 33:112–120
Correia-Pinto J, Tavares ML, Baptista MJ et al (2002) Meconium dependence of bowel damage in gastroschisis. J Pediatr Surg 37:31–35
Api A, Olguner M, Hakguder G et al (2001) Intestinal damage in gastroschisis correlates with the concentration of intraamniotic meconium. J Pediatr Surg 36:1811–1815
Kluck P, Tibboel D, van der Kamp AW, Molenaar JC (1983) The effect of fetal urine on the development of the bowel in gastroschisis. J Pediatr Surg 18:47–50
Morrison JJ, Klein N, Chitty LS et al (1998) Intra-amniotic inflammation in human gastroschisis: possible aetiology of postnatal bowel dysfunction. Br J Obstet Gynaecol 105:1200–1204
Srinathan SK, Langer JC, Blennerhassett MG et al (1995) Etiology of intestinal damage in gastroschisis III: morphometric analysis of the smooth muscle and submucosa. J Pediatr Surg 30:379–383
Kidd JN Jr, Jackson RJ, Smith SD, Wagner CW (2003) Evolution of staged versus primary closure of gastroschisis. Ann Surg 237:759–764 discussion 764–755
Amoury RA, Beatty EC, Wood WG et al (1988) Histology of the intestine in human gastroschisis—relationship to intestinal malfunction: dissolution of the “peel” and its ultrastructural characteristics. J Pediatr Surg 23:950–956
Tibboel D, Vermey-Keers C, Kluck P et al (1986) The natural history of gastroschisis during fetal life: development of the fibrous coating on the bowel loops. Teratology 33:267–272
Molik KA, Gingalewski CA, West KW et al (2001) Gastroschisis: a plea for risk categorization. J Pediatr Surg 36:51–55
Draper ES, Manktelow B, Field DJ et al (1999) Prediction of survival for preterm births by weight and gestational age: retrospective population based study. BMJ 23:1093–1097
Blakelock RT, Upadhyay V, Pease PW, Harding JE (1997) Are babies with gastroschisis small for gestational age? Pediatr Surg Int 12:580–582
Charlesworth P, Njere I, Allotey J et al (2007) Postnatal outcome in gastroschisis: effect of birth weight and gestational age. J Pediatr Surg 42(5):815–818
Logghe HL, Mason GC, Thornton JG, Stringer MD (2005) A randomized controlled trial of elective preterm delivery of fetuses with gastroschisis. J Pediatr Surg 40:1726–1731
Moore TC, Collins DL, Catanzarite V, Hatch EI Jr (1999) Pre-term and particularly pre-labor cesarean section to avoid complications of gastroschisis. Pediatr Surg Int 15(2):97–104
Driver CP, Bowen J, Doig CM et al (2001) The influence of delay in closure of the abdominal wall on outcome in gastroschisis. Pediatr Surg Int 17:32–34
Minkes RK, Langer JC, Mazziotti MV et al (2000) Routine insertion of a silastic spring-loaded silo for infants with gastroschisis. J Pediatr Surg 35:843–846
Bianchi A, Dickson AP, Alizai NK (2002) Elective delayed midgut reduction. No anaesthesia for gastroschisis. J Ped Surg 37(9):1334–1336
Eggink BH, Richardson CJ, Malloy MH, Angel CA (2006) Outcome of gastroschisis: a 20-year case review of infants with gastroschisis born in Galveston, Texas. J Pediatr Surg 41:1103–1108
Lopez de Torre B, Tovar JA, Uriarte S, Aldazabal P (1991) Transperitoneal exchanges of water and solutes in the fetus with gastroschisis. Experimental study in the chick embryo. Eur J Pediatr Surg 1:346–352
Fasching G, Mayr J, Sauer H (1996) The effect of mode of delivery on outcome in fetuses with gastroschisis. Pediatr Surg Int 11:100–102
Vilela PC, Ramos De Amorim MM, Falbo GH, Santos LC (2001) Risk factors for adverse outcome of newborns with gastroschisis in a Brazilian hospital. J Pediatr Surg 36:559–564
Blessed WB, Coughlin JP, Johnson MP et al (1993) Immediate delivery room repair of fetal abdominal wall defects. Fetal Diagn Ther 8:203–208
Driver CP, Bowen J, Doig CM et al (2001) The influence of delay in closure of the abdominal wall on outcome in gastroschisis. Pediatr Surg Int 17:32–34
Komuro H, Imaizumi S, Hirata A, Matsumoto M (1998) Staged silo repair of gastroschisis with preservation of the umbilical cord. J Pediatr Surg 33:485–488
How HY, Harris BJ, Pietrantoni M et al (2000) Is vaginal delivery preferable to elective cesarean delivery in fetuses with a known ventral wall defect? Am J Obstet Gynecol 182:1527–1534
Lenke RR, Hatch EI Jr (1986) Fetal gastroschisis: a preliminary report advocating the use of cesarean section. Obstet Gynecol 67:395–398
Swift RI, Singh MP, Ziderman DA et al (1992) A new regime in the management of gastroschisis. J Pediatr Surg 27:61–63
Quirk JG Jr, Fortney J, Collins HB 2nd et al (1996) Outcomes of newborns with gastroschisis: the effects of mode of delivery, site of delivery, and interval from birth to surgery. Am J Obstet Gynecol 174:1134–1138 discussion 1138–1140
Dunn JC, Fonkalsrud EW, Atkinson JB (1999) The influence of gestational age and mode of delivery on infants with gastroschisis. J Pediatr Surg 34:1393–1395
Segel SY, Marder SJ, Parry S, Macones GA (2001) Fetal abdominal wall defects and mode of delivery: a systematic review. Obstet Gynecol 98:867–873
Landon MB, Hauth JC, Leveno KJ et al (2004) Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med 351:2581–2589 Epub 2004 Dec 2514
Blackwell SC, Redman ME, Tomlinson M et al (2001) Labor induction for the preterm severe pre-eclamptic patient: is it worth the effort? J Matern Fetal Med 10:305–311
Chappuis JP, Takvorian P, Philibert M et al (1984) Current aspects of laparoschisis. Apropos of 22 cases. Pediatrie 39:437–444
Guo W, Swaniker F, Fonkalsrud EW et al (1995) Effect of intraamniotic dexamethasone administration on intestinal absorption in a rabbit gastroschisis model. J Pediatr Surg 30:983–986 discussion 986–987
Yu J, Gonzalez-Reyes S, Diez-Pardo JA, Tovar JA (2004) Local dexamethasone improves the intestinal lesions of gastroschisis in chick embryos. Pediatr Surg Int 19:780–784
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gelas, T., Gorduza, D., Devonec, S. et al. Scheduled preterm delivery for gastroschisis improves postoperative outcome. Pediatr Surg Int 24, 1023–1029 (2008). https://doi.org/10.1007/s00383-008-2204-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-008-2204-y