Abstract
Aim of the study
To evaluate if gestational age (GA), mode of delivery and abdominal wall closure method influence outcomes in uncomplicated gastroschisis (GTC).
Methods
Retrospective review of NICU admissions for gastroschisis, August 2008–July 2016. Primary outcomes were: time to start enteral feeds (on-EF), time to discontinue parenteral nutrition (off-PN), and length of stay (LOS).
Main results
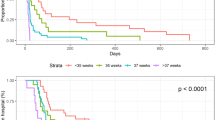
A total of 200 patients with GTC were admitted to our NICU. Patients initially operated elsewhere (n = 13) were excluded. Patients with medical/surgical complications (n = 62) were analyzed separately. The study included 125 cases of uncomplicated GTC. There were no statistically significant differences in the outcomes of patients born late preterm (34 0/7–36 6/7; n = 70) and term (n = 40): on-EF 19 (5–54) versus 17 (7–34) days (p = 0.29), off-PN 32 (12–101) versus 30 (16–52) days (p = 0.46) and LOS 40 (18–137) versus 37 (21–67) days (p = 0.29), respectively. Patients born before 34 weeks GA (n = 15) had significantly longer on-EF, off-PN and LOS times compared to late preterm patients: 26 (12–50) days (p = 0.01), 41 (20–105) days (p = 0.04) and 62 (34–150) days (p < 0.01), respectively. There were no significant differences in outcomes between patients delivered by C-section (n = 62) and patients delivered vaginally (n = 63): on-EF 20 (5–50) versus 19 (7–54) days (p = 0.72), off-PN 32 (12–78) versus 33 (15–105) days (p = 0.83), LOS 42 (18–150) versus 41 (18–139) days (p = 0.68), respectively. There were significant differences in outcomes between patients who underwent primary reduction (n = 37) and patients who had a silo (88): on-EF 15 (5–37) versus 22 (6–54) days (p < 0.01), off-PN 28 (12–52) versus 34 (15–105) days (p = 0.04), LOS 36 (18–72) versus 44 (21–150) days (p = 0.04), respectively.
Conclusion
In our experience, late preterm delivery did not affect outcomes compared to term delivery in uncomplicated GTC. Outcomes were also not influenced by the mode of delivery. Patients who underwent primary reduction had better outcomes than patients who underwent silo placement.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prenatal diagnosis GTC has played a key role in the improved outcomes of patients with uncomplicated gastroschisis observed in the last three decades [1,2,3,4]. The main factors for this are the early diagnosis, the antenatal surveillance, and the possibility of referring women carrying fetuses with GTC to centers where the fetuses can be delivered and receive intensive neonatal and surgical care immediately after birth. The outcomes of patients with uncomplicated GTC, although generally favorable, are still quite variable for reasons and mechanisms that are not completely clear. It is likely that a combination of prenatal factors, perinatal events and postnatal management strategies contribute to the end result. In this study, we evaluated a large series of patients with uncomplicated gastroschisis treated by the same multidisciplinary team of maternal fetal medicine specialists, surgeons and neonatologists in an attempt to determine if the gestational age at birth, mode of delivery and abdominal wall closure method have any influence on surgical outcomes. We only included in this study patients who had an uneventful neonatal course, without any of the many potential complications that can occur in patients born with GTC, to have the most homogeneous group possible.
Materials and methods
After obtaining Institutional Review Board (IRB) approval (IRB 17-013720), we conducted a retrospective review of all patients with gastroschisis admitted to our neonatal intensive care unit between August 2008 and July 2016. A total of 200 patients were identified. We excluded from this analysis 13 patients referred to us for a variety of complications after undergoing operation at other hospitals, 4 patients born at other hospitals referred to us for ECMO due to meconium aspiration, and 58 patients with complex GTC due to intra-abdominal complications either present at birth or developed during their neonatal admission (e.g., intestinal atresia, necrotizing enterocolitis, compartment syndrome, closure dehiscence, bowel necrosis at birth, in utero midgut volvulus). The presence of a thick peel and/or edematous bowel wall was not considered a complication. We included in the study a homogeneous group of 125 patients with simple, uncomplicated GTC. We defined simple GTC as those cases who were not born with complications and who did not develop significant complications during their neonatal hospital stay. None of the patient had clinically relevant concomitant cardiac or renal or pulmonary anomalies. By excluding all types of major complications and clinical relevant co-morbidities, we aimed to learn the primary surgical outcomes of only those patients who had an uncomplicated clinical course. We retrospectively reviewed the prenatal ultrasound findings, perinatal management and postnatal surgical management, and correlated them with surgical outcomes. There was no protocol to deliver fetuses before term, therefore fetuses born before term did so, because of spontaneous preterm labor, or preterm induction/cesarean section due to non-reassuring fetal tracing. We additionally compared the outcomes between inborn cases and outborn cases. All patients were treated by the same medical and surgical teams. The abdominal wall closure method (primary reduction versus silo placement) was not protocolized or randomized, but instead was left at the discretion of each patient’s surgeon. Patients in the analyzed group had no episodes of sepsis of any source. The primary outcomes of the study were: time to initiate enteral feeds (on-EF), time to discontinue parenteral nutrition (off-PN), and length of stay (LOS). Statistical significance was determined by t-test and Chi square test for means and proportions, respectively. A p value less than 0.05 was considered statistically significant.
Results
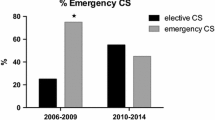
We observed no statistically significant differences in the outcomes of patients born late preterm (34 0/7–36 6/7) versus term (Table 1A). In contrast, patients born early preterm (< 34 weeks GA) had significantly longer on-EF, off-PN and LOS times compared to late preterm patients. We found no statistically significant differences in outcomes between patients delivered by C-section and patients delivered vaginally (Table 1B). The frequency of cesarean delivery within the late preterm and term groups was not statistically different [37/70 (53%) vs. 17/40 (43%), respectively; p = 0.4]. The outcomes were significantly different between patients who underwent primary reduction and patients who had a silo (Table 1C).
Most patients in our series (112/125; 89.6%) were referred to us before birth and were born in our special delivery unit located within our free-standing children’s hospital. Only 13 patients in the series (10.4%) were transported to our NICU after being delivered elsewhere. We did not find a statistically significant difference in outcomes between inborn patients and outborn patients: on-EF 19 (6–50) versus 22 (5–54) days (p = 0.28), off-PN 32 (15–105) versus 34 (12–78) days (p = 0.67), LOS 41 (20–139) versus 48 (18–150) days (p = 0.24), respectively.
The vast majority of the patients in the series were diagnosed prenatally (121/125, 96.8%). Detailed ultrasound features were available in 118 cases. There were 33 cases with abnormal findings on the prenatal ultrasound in addition to the abdominal wall defect: extra-abdominal bowel dilatation (n = 20), intra-abdominal bowel dilatation (n = 22), dilatation of the stomach (n = 5), bowel hypoperistalsis (n = 3), and bowel wall thickening (n = 1). Several patients had more than one finding. None of the patients with abnormal prenatal findings had anatomical anomalies detected after birth. Patients with abnormal prenatal ultrasound findings were demographically equivalent to patients without abnormal prenatal ultrasound findings in terms of gestational age at birth, proportion of early preterm/late preterm/term deliveries, proportion of fetuses delivered due to non-reassuring fetal tracing and rate of primary GTC. We compared the surgical outcomes of patients with abnormal ultrasound features versus patients without abnormal ultrasound features and found no statistically significant differences (Table 2).
There were no mortalities between the time of birth and the time of hospital discharge.
Discussion
Uncomplicated gastroschisis is currently a condition with low morbidity, infrequent long-term sequelae and close to zero neonatal mortality in developed countries [5, 6]. In developing countries, on the other hand, mortality rates are still as high as 100% [7,8,9]. Despite being generally benign, the outcomes of uncomplicated gastroschisis present a wide range of variability, even within apparently homogeneous patient populations. To identify factors that could further improve outcomes, several aspects of the management of patients with GTC have been individually evaluated and reported in the literature, often with conflicting results. Among these are: the prenatal identification of intestinal complications, the time of delivery, the mode of delivery and the abdominal wall closure technique.
One of the strongest and well-known predictors of poorer outcomes in GTC is the prenatal development of intestinal complications such as intestinal atresia, volvulus or necrosis. But even though it would be ideal to be able to identify these events by ultrasound before they occur and potentially intervene prenatally, there are no imaging features that are 100% sensitive and specific for any of those intestinal complications. Our finding of 33 fetuses with abnormal prenatal ultrasound features but an uneventful neonatal course supports this concept (33/118; 28%), confirming the findings in several studies in the literature [10,11,12,13].
There are experimental and clinical data in the literature supporting the hypothesis that the intestinal morbidity observed in patients with GTC may derive, at least in part, from damage to the bowel wall that occurs by being exposed to the amniotic fluid and as well as constriction of the intestine and its blood supply at the abdominal wall opening [14,15,16]. Based on this premise, numerous authors have advocated for elective preterm deliveries in gastroschisis with or without abnormal ultrasound findings [17,18,19], and even at the present time, this is the standard management in some parts of the world [20,21,22,23]. On the other hand, there are numerous articles in the literature suggesting that there are no benefits, and there may be increased morbidity, to delivering fetuses with GTC prematurely [24,25,26,27]. Our study supports that there is no advantage to routinely delivering fetuses with GTC prematurely. On the other hand, our data also suggests that if it becomes indicated based on abnormal findings on the fetal health surveillance, late preterm delivery is not detrimental to the long-term outcomes in GTC. Our study adds to previously published data a homogeneous series, large, single-center series of mostly (89.6%) inborn patients who received the same standardized prenatal, perinatal and postnatal care, provided by the same group of maternal-fetal medicine specialists, surgeons and neonatologists.
The optimal mode of delivery for fetuses with GTC has also been controversial in the literature over the years, and much like the issue of the optimal gestational age, practices vary around the world [20, 28,29,30,31,32]. The current prevailing opinion is that vaginal delivery does not impose additional risk to patients with GTC, and the centers that continue to perform C-sections for GTC do so for the purpose of electively preterm delivery. Our study supports that the mode of delivery plays little to no role in the outcome of uncomplicated GTC. Cesarean deliveries are performed in our institution for routine obstetric indications unrelated to GTC. In our series, the indications for a cesarean delivery included non-reassuring fetal tracing (n = 36), failed induction of labor (n = 9), breech presentation (n = 5), repeat C-section (n = 4), maternal indications (n = 3) and others (n = 5). The overall rate of cesarean section in our study group was ≈ 50%.
We did not find any differences in outcomes between inborn patients and outborn patients. This finding was unexpected, because it is well-established in the literature that there is benefit to delivering at tertiary, high-volume centers [33,34,35]. A possible explanation for the similarity in outcomes could be the disparity in the number of cases in each group: 112 inborn versus only 13 outborn—a larger number of outborn patients might show differences. Additionally, most of those 13 outborn patients were transported to our NICU from centers within a 5-mile radius thus requiring a short transport, some were followed by us prenatally, and 3 babies were actually born in the adjacent adult hospital requiring just a transport through a connecting hallway.
The abdominal wall closure method seems to influence the outcome of patients with uncomplicated GTC, with primary reduction/closure having benefits over all forms of delayed closure [36,37,38]. That being said, it is possible that this observation is biased by the fact that primary reduction tends to be successful in cases where the intestine is in good condition (thin wall, no peel) and there is adequate abdominal capacity for primary reduction. Patients who have the intestine in worse condition (wall edema, thick peel, shortened mesentery) generally undergo spring-loaded silo placement at the bedside, because the eviscerated bowel is in a pack and the manipulation of each individual bowel loop necessary for the complete primary reduction is not feasible (in our experience, a primary reduction is generally possible when we can gradually reduce the intestine loop by loop). In other words, the techniques are not applied randomly, so it is not the technique but rather the condition of the bowel what may determine the outcome. We did not collect prospective data regarding the condition of the bowel at birth, so while we saw a difference in the outcomes between patients who underwent a primary reduction and patients who received a silo, we do not know if the condition of the bowel was comparable between groups and therefore cannot conclude that one closure method was better than the other. Our primary reductions are done in the NICU under anesthesia. We place a nasogastric tube, a Foley catheter and squeeze the colon gently to evacuate the meconium. Next, we gradually reduce the eviscerated bowel and leave the fascial defect open. We then cover the defect with the stump of the umbilical cord and a sterile occlusive dressing. The primary reduction technique has several versions: with anesthesia, without anesthesia, leaving the fascial defect open, closing it after the reduction, a bedside procedure, an OR procedure, and even a primary reduction in the delivery room prior to clamping the umbilical cord [39,40,41]. Regardless, careful judgement needs to be applied on a case by case basis when attempting a primary reduction to avoid the development of abdominal compartment syndrome and the potentially catastrophic consequences related to bowel ischemia and necrosis.
Conclusion
Patients with GTC can develop a number of prenatal and/or postnatal complications that can greatly influence the outcomes. There is a subgroup of patient with gastroschisis, on the other hand, who does not have any prenatal complications and does not develop any postnatal complications. In this select group of patients with simple, uncomplicated GTC, we found no differences in the surgical outcomes of those born at late preterm compared to those born at term. In our opinion, elective delivery before term in gastroschisis is not justified, regardless of the prenatal findings. The outcomes were not influenced by the mode of delivery either, thus cesarean delivery should only be performed for routine obstetric indications independent of GTC. Patients who underwent primary reduction had better outcomes than patients who underwent silo placement-delayed closure, although this is likely not intrinsically related to the technique but rather to the condition of the bowel, since bowel with wall edema and a thick peel is generally not amenable to primary reduction.
References
Grossman M, Fischermann EA, German J (1978) Sonographic findings in gastroschisis. J Clin Ultrasound 6:175–176
Stringel G, Filler RM (1979) Prognostic factors in omphalocele and gastroschisis. J Pediatr Surg 14:515–519
Lewis JE Jr, Kraeger RR, Danis RK (1973) Gastroschisis: ten-year review. Arch Surg 107:218–222
Young DG. Gastroschisis (1967) Proc R Soc Med 60:15–16
Dalton BG, Gonzalez KW, Reddy SR et al (2016) Improved outcomes for inborn babies with uncomplicated gastroschisis. J Pediatr Surg. https://doi.org/10.1016/j.jpedsurg.2016.12
Youssef F, Cheong LH, Emil S (2016) Gastroschisis outcomes in North America: a comparison of Canada and the United States. J Pediatr Surg 51:891–895
Marshall Niles SG, Mitchell-Fearon K, Gill MI et al (2017) Mortality-related factors in gastroschisis—a Jamaican perspective. J Pediatr Surg 52:530–533
Wesonga AS, Fitzgerald TN, Kabuye R et al (2016) Gastroschisis in Uganda: opportunities for improved survival. J Pediatr Surg 51:1772–1777
Apfeld JC, Wren SM, Macheka N et al (2015) Infant, maternal, and geographic factors influencing gastroschisis related mortality in Zimbabwe. Surgery 158:1475–1480
Badillo AT, Hedrick HL, Wilson RD et al (2008) Prenatal ultrasonographic gastrointestinal abnormalities in fetuses with gastroschisis do not correlate with postnatal outcomes. J Pediatr Surg 43:647–653
Alfaraj MA, Ryan G, Langer JC et al (2011) Does gastric dilation predict adverse perinatal or surgical outcome in fetuses with gastroschisis? Ultrasound Obstet Gynecol 37:202–206
Page R, Ferraro ZM, Moretti F et al (2014) Gastroschisis: antenatal sonographic predictors of adverse neonatal outcome. J Pregnancy 2014:239406. https://doi.org/10.1155/2014/239406
Davis RP, Treadwell MC, Drongowski RA et al (2009) Risk stratification in gastroschisis: can prenatal evaluation or early postnatal factors predict outcome? Pediatr Surg Int 25:319–325
Langer JC, Longaker MT, Crombleholme TM et al (1989) Etiology of intestinal damage in gastroschisis. I: effects of amniotic fluid exposure and bowel constriction in a fetal lamb model. J Pediatr Surg 24:992–997
Api A, Olguner M, Hakgüder G et al (2001) Intestinal damage in gastroschisis correlates with the concentration of intraamniotic meconium. J Pediatr Surg 36:1811–1815
Correia-Pinto J, Tavares ML, Baptista MJ et al (2002) Meconium dependence of bowel damage in gastroschisis. J Pediatr Surg 37:31–35
Moir CR, Ramsey PS, Ogburn PL et al (2004) A prospective trial of elective preterm delivery for fetal gastroschisis. Am J Perinatol 21:289–294
Serra A, Fitze G, Kamin G et al (2008) Preliminary report on elective preterm delivery at 34 weeks and primary abdominal closure for the management of gastroschisis. Eur J Pediatr Surg 18:32–37
Peiró JL, Guindos S, Lloret J et al (2005) New surgical strategy in gastroschisis: treatment simplification according to its physiopathology. Cir Pediatr 18:182–187
Schib K, Schumacher M, Meuli M et al (2017) Prenatal and postnatal management of gastroschisis in German-speaking countries: is there a standardized management? Eur J Pediatr Surg. https://doi.org/10.1055/s-0037-1598103
Mesas Burgos C, Svenningsson A, Vejde JH (2015) Outcomes in infants with prenatally diagnosed gastroschisis and planned preterm delivery. Pediatr Surg Int 31:1047–1053
Krause H, Hass HJ, Böttger R et al (2015) Surgical treatment results in gastroschisis based on preterm delivery within the 34th week of gestation by caesarean section. Pol Przegl Chir 87:346–356
Fernández Ibieta M, Aranda García MJ, Cabrejos Perotti C et al (2013) Preliminary results of a multidisciplinary approach to gastroschisis. Cir Pediatr 26:30–36
Carnaghan H, Baud D, Lapidus-Krol E et al (2016) Effect of gestational age at birth on neonatal outcomes in gastroschisis. J Pediatr Surg 51:734–738
Carnaghan H, Pereira S, James CP et al (2014) Is early delivery beneficial in gastroschisis? J Pediatr Surg 49:928–933
Bond DM, Gordon A, Hyett J et al (2015) Planned early delivery versus expectant management of the term suspected compromised baby for improving outcomes. Cochrane Database Syst Rev (11):CD009433. https://doi.org/10.1002/14651858.CD009433
Wilson MS, Carroll MA, Braun SA et al (2012) Is preterm delivery indicated in fetuses with gastroschisis and antenatally detected bowel dilation? Fetal Diagn Ther 32:262–266
Bethel CA, Seashore JH, Touloukian RJ (1989) Cesarean section does not improve outcome in gastroschisis. J Pediatr Surg 24:1–3
Lenke RR, Hatch EI Jr (1986) Fetal gastroschisis: a preliminary report advocating the use of cesarean section. Obstet Gynecol 67:395–398
Grundy H, Anderson RL, Filly RA et al (1987) Gastroschisis: prenatal diagnosis and management. Fetal Ther 2:144–147
Langer JC, Harrison MR, Adzick NS et al (1987) Perinatal management of the fetus with an abdominal wall defect. Fetal Ther 2:216–221
Reigstad I, Reigstad H, Kiserud T et al (2011) Preterm elective caesarean section and early enteral feeding in gastroschisis. Acta Paediatr 100:71–74
Dalton BG, Gonzalez KW, Reddy SR et al (2016) Improved outcomes for inborn babies with uncomplicated gastroschisis. J Pediatr Surg 52(7):1132–1134
Sacks GD, Ulloa JG, Shew SB (2016) Is there a relationship between hospital volume and patient outcomes in gastroschisis repair? J Pediatr Surg 51:1650–1654
Savoie KB, Huang EY, Aziz SK et al (2014) Improving gastroschisis outcomes: does birth place matter? J Pediatr Surg 49:1771–1775
Luck SR, Sherman JO, Raffensperger JG et al (1985) Gastroschisis in 106 consecutive newborn infants. Surgery 98:677–683
Banyard D, Ramones T, Phillips SE et al (2010) Method to our madness: an 18-year retrospective analysis on gastroschisis closure. J Pediatr Surg 45:579–584
Dore Reyes M, Triana Junco P, Barrena Delfa S et al (2016) Primary versus secondary closure: ventilatory and nutritional differences in patients with gastrosquisis. Cir Pediatr 29:49–53
Bianchi A, Dickson AP (1998) Elective delayed reduction and no anesthesia: ‘minimal intervention management’ for gastrochisis. J Pediatr Surg 33:1338–1340
Pet GE, Stark RA, Meehan JJ et al (2017) Outcomes of bedside sutureless umbilical closure without endotracheal intubation for gastroschisis repair in surgical infants. Am J Surg 213(5):958–962
Zhang ZT, Liu CX, Zhou YZ et al (2010) Intrapartum operation on fetuses with birth defects and its outcome. Zhonghua Fu Chan Ke Za Zhi 45:652–657
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fraga, M.V., Laje, P., Peranteau, W.H. et al. The influence of gestational age, mode of delivery and abdominal wall closure method on the surgical outcome of neonates with uncomplicated gastroschisis. Pediatr Surg Int 34, 415–419 (2018). https://doi.org/10.1007/s00383-018-4233-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-018-4233-5