Abstract
Palmar hyperhidrosis (PHH) is fairly a common condition, which is treatable by thoracoscopic sympathectomy (TS). Compensatory sweating (CS) is a major side effect of TS. We compared the TS procedure’s long-term success, patient’s satisfaction and complications between children (≤14 years of age) and adolescents and adults (≥15 years of age). A chart review of the patients who had undergone TS at three medical centers (Hillel Yaffe, Soroka and Bnai-Zion) who could be contacted and agreed to reply to a detailed telephone questionnaire yielded 325 patients with a >24-month follow-up. There were 116 children and 209 adolescents and adults with a follow-up of 2–8 years. Most participants (96.3%) reported complete or reasonable symptomatic relief. The long-term postoperative satisfaction was high (84.5%), and significantly higher among children (92.2%) compared to adolescents and adults (80.7%) (P = 0.005). CS appeared within 6 months postoperatively in 81.8% of all the patients but significantly less in children (69.8%) compared to the others (88.5%; P < 0.001). CS increased with time in 12% of the participants, but decreased in 20.8% of the children versus 10.5% of the others (P = 0.034), usually within the first two postoperative years. The severity of the CS was also lower in children: it was absent or mild in 54.3% of the children versus 38.0% of the others, and moderate or severe in 45.7 versus 62%, respectively (P = 0.004). Fifty-one percent of the participants claimed that their quality of life decreased moderately or severely as a result of CS, but only one-third of them (7.9% children vs. 22.4% others, P = 0.001) would not have undergone the operation in retrospect. Thoracoscopic sympathectomy relieves PHH in most cases. Most patients prefer relief from PHH even at the cost of moderate or severe CS. The rate of CS and its severity is tolerated better by children, and their postoperative satisfaction is higher than that of adolescents and adults. Therefore, unless otherwise contraindicated, we recommend doing TS as early as possibly
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Palmar hyperhidrosis (PHH) is a fairly common condition for which there is no efficient medical remedy. Thoracoscopic sympathectomy (TS), a surgical procedure based on the interruption of transmission of impulses from the sympathetic ganglia to the sweat glands, offers a permanent cure of PHH. Although it successfully resolves excessive palmar perspiration, TS bears a considerable long-term cost postoperatively, that of compensatory sweating (CS). We recently published our long-term postoperative results following TS [1]. We had unexpectedly found, for what we believe to be the first time, an apparent difference in the postoperative satisfaction rate between children and adults. That finding motivated us to address the issue of such a possible difference between children and older patients in greater depth. In the current study, we compared the scores for long-term success, satisfaction and complication rates between children and adolescents and adults who had undergone TS 2–8 years earlier (January 1997–December 2004).
Materials and methods
We reviewed the medical charts of 533 patients who had undergone TS and who were followed-up for more than 24 months at the Hillel Yaffe Medical Center (HYMC, Hadera, Israel) Bnai Zion Medical Center (BZMC, Haifa, Israel) and the Soroka Medical Center (SMC, Beersheba, Israel) between January 1998 and December 2004. We asked these individuals to reply to a detailed telephone questionnaire on the surgical success rate, the postoperative satisfaction, and any postoperative long-term complications, with emphasis on any subsequent CS. We then compared the answers of the participating children (≤14 years of age) to those of the compliant adolescents and adults (≥15 years of age).
The surgical technique in all three centers was similar. We used one 10 mm camera with a working 5-mm channel (Karl Storz, GmbH and Co., Tuttlingen, Germany) through which a hook was introduced. The sympathetic chain was ablated on the second and the third ribs for PHH, and on the fourth rib as well for axillary hyperhidrosis. The procedure was done bilaterally in all cases. These operations were performed by one senior pediatric surgeon in HYMC, by two senior pediatric surgeons in SMC and by two senior pediatric surgeons and one senior general surgeon in BZMC. Each surgeon was highly experienced in performing the procedure.
Statistical analysis and IRB approval
Data analysis was performed with Pearson’s Chi-square test as appropriate for categorical variables. Significance was set at P < 0.05. The study was approved by the Institutional Review Board of the Hillel Yaffe Medical Center.
Results
A total of 325 patients complied in responding to the questionnaires, of whom 116 were children (8–14 years of age, median = 13) and 209 were adolescents and adults (15–41 years of age, median = 18). The length of follow-up ranged between 2 and 8 years. There were 193 females (female/male ratio 1.46). Three-hundred and twelve responders (96.3%) reported complete or reasonable symptomatic relief. There was no difference in the reported prevalence of sweaty hands between the children and the older patients. The long-term postoperative satisfaction was 92.2% for the children, but only 80.7% for the adolescents and adults (P = 0.005). One-hundred and six children (92.1%) responded that they would have undergone the operation in retrospect compared to 163 (77.6%) of the others (P = 0.001) (Table 1).
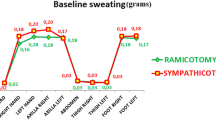
Compensatory sweating was a frequent long-term consequence. It appeared in 266 (81.8%) of the patients, with a significant difference between the older 185 (88.5%) patients and the 81 (69.8%) children (P < 0.001) (Table 2). The severity of CS was also different between the two age groups: the CS was absent or mild in 63 (54.3%) children compared to 79 (38.0%) adolescents and adults (P = 0.004), and moderate or severe in 53 (45.7%) children and in 130 (62.0%) of the others (P = 0.004) (Table 3).
About half of the patients with CS reported that they did not suffer from it or considered that the problem was mild. The quality of life, however, was moderately diminished in 68 (26.9%) and severely diminished in 64 (24.1%) of the patients, with no difference between the younger and older ones (Table 4).
The CS was located at the back in 148 (69.5%) patients, in the soles of the feet in 105 (49.3%), in the abdomen in 49 (23%), in the chest in 15 (7%), and in the face in 12 (5.6%). It involved more than one area in 69% of the patients. When CS was present, it appeared almost immediately following the procedure in 56% of the patients, by 3 months postoperatively in 84.4%, and by 6 months postoperatively in most of them.
The extent of the CS increased with time in 12.8% of the group, but it diminished in 20.8% of children compared to 10.5% of the older patients (P = 0.034), usually within the first two postoperative years (Table 5). Only 55.6% of the patients answered that question.
Discussion
Severe PHH has a considerable negative effect on the affected individual’s quality of life [2]. TS is a well-established operative procedure that reduces the extent of perspiration from excessive to normal in the vast majority of patients. Such was the case in our study of the patients and in the ones reported in the literature [3–5]
With the exception of CS, the long-term morbidity associated with TS is relatively low [5–7]. CS is the most common side effect, primarily affecting the back, the soles and the torso, and it is the main reason for patient’s dissatisfaction [8, 9]. Indeed, despite having dry hands as a result of surgery, patients may report only moderate satisfaction, dissatisfaction or even regret having undergone the operation because of the appearance of CS [10–12]. The specific rate of CS in some recent series ranged between 60 and 90%, and it was considered as being severe in one-third of them [13–16]. Our rate of CS was 81.8%, with a significant difference between children (69.8%) and adults (88.5%). We do not know if this was because of physiological or adaptive reasons. The level of sympathectomy and facial hyperhydrosis (HH) were mentioned as factors affecting outcome following TS [9, 17, 18], but as far as we know, being a child has not been previously mentioned as one of these factors. The reason for our finding might be a secondary effect of the sympathectomy. In addition to the symptomatic relief, dry hands may improve some of the obstacles to the social acceptance of younger patients, such as having copybooks with sweaty streaks, embarrassing slippery accidents in sports activities, etc. These obstacles, if not treated, can potentially aggravate PHH with time. By relieving many of them, sympathectomy improves some of the stress effects that aggravate primary hyperhidrosis. One can expect that the reduction in the stress load may have some secondary effect on CS as well.
The overall satisfaction in children was very high (92.2%), and only 7.9% of them would not have agreed to the operation in retrospect. The adults were less satisfied, with 22.4% of them not having undergone the operation in retrospect. Operative satisfaction is the net result of operative success, the rate, severity and ability of CS to negatively affect quality of life and a variable that might potentially change with time. Our operative success in children as well as in adolescents and adults was high, but the rate of CS and its severity were significantly higher in the older patients. Furthermore, the rate of decrease of CS with time was double for the children compared to that of the adolescents and adults. Greater social pressure and vulnerability to their peers’ opinion of them may be some of the reasons for the children’s attitudes. Sympathectomy relieves many of the obstacles to social acceptance and puts an end to embarrassing accidents in many daily activities. The social pressure on adults is different, and adults have far greater choices in the activities that suit them, with far more opportunities to avoid situations in which sweating is inconvenient or provokes humiliation by others.
There is no effective medical remedy for PHH. The surgical alternative was offered only after the surgeon was convinced that the patient’s quality of life had been seriously compromised for a considerable length of time and that all other efforts to improve it, e.g., antiperspirants, iontophoresis, hypnosis, acupuncture, etc., had failed. Surgery was scheduled only after the suitable candidate was given a clear explanation of the potential operative risks—especially the high risk of having CS that may, in some cases, be worse than the original PHH. We do not encourage our patients to undergo the operation. On the contrary, we express our reluctance to perform it because of the 70% potential of the occurrence of CS. Having said that, once the patient and his/her parents decide upon the surgical alternative, we recommended doing TS as early as possibly because: (1) PHH is not a self-limiting condition and so there is no reason to extend the patient’s suffering; (2) the chances of CS and the degree of its severity are significantly lower in children younger than 14 years; (3) the postoperative satisfaction is very high in children younger than 14 years (>92%) and it is significantly higher than in older patients. The youngest patient who presented to us with PHH and who wanted to undergo this procedure was 8 years old. We think that TS can be offered to children from this age onwards, once the patient and his/her parents fulfill the above-mentioned operative criteria. It should be borne in mind that Israel is a hot country, and it is estimated that nearly 1% of its population (∼70,000 people) suffers from some degree of PHH [19].
The compensatory effect appears to be a dynamic process [5, 10, 16]. It developed immediately following the procedure in 50% of our affected patients, after 3 months in 80%, and after three additional months in 90%. The severity of the CS did not change with time in 73% of our patients. It increased in severity in 12.8% and decreased in severity in 20.8% of the children, but only in 10.5% of the adults within 2 years postoperatively. This phenomenon may also reflect a possible positive long-term secondary effect of dry hands on young people. Only 148 out of 266 (55.6%) patients, however, answered the questions concerning CS dynamics. The difficulty in recalling this change may be due to the gradual nature of the change and the relatively long time that had elapsed since any change had occurred.
Although CS may significantly diminish one’s quality of life (39 out of 116 children, 96 out of 209 adults, Table 4), 30/39 (76.9%) of the children and 55/96 (57.3%) of the adults with severe CS were still satisfied in the long term. This paradoxical response was also witnessed by others [16–18, 20] and it may be considered a testimony to how unbearable was the preoperative PHH.
This study has two main weaknesses. First, it shares the usual limitations of a retrospective study. Second, the collected data are subjective, and there was no objective test to validate the patient’s feelings about his/her quality of life or the severity of CS. In addition, some of the subjective responses depended upon relatively long-term recollection of how much time had elapsed after surgery before CS appeared.
In conclusion, our findings showed that although TS succeeded in considerably reducing excessive PHH in the vast majority of patients of all ages, the rate of CS was shown to be high, albeit significantly lower and milder in children. Despite the high rate of CS associated with TS, most of the children, in contrast to the adolescents and adults, were gratified with the effect the procedure that had on their daily lives and most of them would have undergone the operation in retrospect. The postoperative intensity of CS decreased in children twice as often as in adults within 2 years after surgery. Therefore, we recommend that when needed, TS should be done as early as possible.
References
Steiner Z, Kleiner O, Hershkovitz Y, Mogilner J, Cohen Z (2007) Compensatory sweating following thoracoscopic sympathectomy: an acceptable trade-off. J Pediatr Surg 42:1388–1392
Panhofer P, Zacherl J, Jakesz R, Bischof G, Neumayer C (2006) Improved quality of life after sympathetic block for upper limb hyperhidrosis. Br J Surg 93(5):582–586
Kestenholz PB, Weder W (2002) Thoracic sympathectomy. Curr Probl Dermatol 30:64–76
Dumont P, Denoyer A, Robin P (2004) Long-term results of thoracoscopic sympathectomy for hyperhidrosis. Ann Thorac Surg 78:1801–1807
Gossot D, Galetta D, Pascal A, Debrosse D, Caliandro R, Girard P, Stern JB, Grunenwald D (2003) Long-term results of endoscopic thoracic sympathectomy for upper limb hyperhidrosis. Ann Thorac Surg 75:1075–1079
Kao MC, Lin JY, Chen YL, Hsieh CS, Cheng LC, Huang SJ (1996) Minimally invasive surgery: video endoscopic thoracic sympathectomy for palmar hyperhidrosis. Ann Acad Med Singapore 25:673–678
Cohen Z, Levi I, Pinsk I, Mares AJ (1998) Thoracoscopic upper thoracic sympathectomy for primary palmar hyperhidrosis—the combined paediatric, adolescents and adult experience. Eur J Surg Suppl 580:5–8
Rex LO, Drott C, Claes G, Göthberg G, Dalman P (1998) The Böras experience of endoscopic thoracic sympathectomy for palmar, axillary, facial hyperhidrosis and facial blushing. Eur J Surg Suppl 580:23–26
Chou SH, Kao EL, Lin CC, Chang YT, Huang MF (2006) The importance of classification in sympathetic surgery and a proposed mechanism for compensatory hyperhidrosis: experience with 464 cases. Surg Endosc 20(11):1749–1753 Epub 5 Oct 2006
Chiou SM (2005) Chronological changes of postsympathectomy compensatory hyperhidrosis and recurrent sweating in patients with palmar hyperhidrosis. J Neurosurg Spine 2:151–154
Herbst F, Plas EG, Fugger R, Fritsch A (1994) Endoscopic thoracic sympathectomy for primary hyperhidrosis of the upper limbs. A critical analysis and long-term results of 480 operations. Ann Surg 220:86–90
Lai YT, Yang LH, Chio CC, Chen HH (1997) Complications in patients with palmar hyperhidrosis treated with transthoracic endoscopic sympathectomy. Neurosurgery 41:110–115
Friedman B, Zohar E, Shachor D, Bendahan J, Jedeikin R (2000) Video-assisted transthoracic sympathectomy in the treatment of primary hyperhidrosis: friend or foe? Surg Laparosc Endosc Percutan Tech 4:226–229
Lin TS, Wang NP, Huang LC (2001) Pitfalls and complication avoidance associated with transthoracic endoscopic sympathectomy for primary hyperhidrosis (analysis of 2200 cases). Int J Surg Investig 2:377–385
Zacherl J, Huber ER, Imhof M, Plas EG, Herbst F, Függer R (1998) Long-term results of 630 thoracoscopic sympathectomies for primary hyperhidrosis: the Vienna experience. Eur J Surg Suppl 580:43–46
Licht PB, Pilegaard HK (2004) Severity of compensatory sweating after thoracoscopic sympathectomy. Ann Thorac Surg 78:427–431
Jaffer U, Weedon K, Cameron AE (May 2007) Factors affecting outcome following endoscopic thoracic sympathectomy. Br J Surg 11 [Epub ahead of print]
Dewey TM, Herbert MA, Hill SL, Prince SL, Mack MJ (2006) One-year follow-up after thoracoscopic sympathectomy for hyperhidrosis: outcomes and consequences. Ann Thorac Surg 81(4):1227–1232 discussion 1232–1233
Adar R, Kurchin A, Zweig A, Mozes M (1977) Palmar hyperhidrosis and its surgical treatment: a report of 100 cases. Ann Surg 186:34–41
Leseche G, Castier Y, Thabut G, Petit MD, Combes M, Cerceau O, Besnard M (2003) Endoscopic transthoracic sympathectomy for upper limb hyperhidrosis: limited sympathectomy does not reduce postoperative compensatory sweating. J Vasc Surg 37:124–128
Author information
Authors and Affiliations
Corresponding author
Additional information
Hillel Yaffe Medical Center and Bnai-Zion Medical Center are affiliated to the Rappaport Faculty of Medicine, The Technion, Haifa, Israel. Soroka Medical Center is affiliated to Ben-Gurion University, Beer-Sheba, Israel.
Rights and permissions
About this article
Cite this article
Steiner, Z., Cohen, Z., Kleiner, O. et al. Do children tolerate thoracoscopic sympathectomy better than adults?. Pediatr Surg Int 24, 343–347 (2008). https://doi.org/10.1007/s00383-007-2073-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-007-2073-9