Abstract
Purpose
Endoscopic thoracic sympathectomy/sympathotomy for the treatment of palmar hyperhidrosis is generally performed by either cutting or clamping the sympathetic chain. However, it remains unclear as to which of these methods is more effective and has fewer side effects. This study was conducted to compare the effects of sympathotomy by cutting or clamping at T3 on two outcomes—postoperative palmar sweating and compensatory sweating; it also evaluated postoperative patient satisfaction.
Methods
The participants were among 289 patients who underwent bilateral sympathotomy at T3 for palmar hyperhidrosis. These patients were sent questionnaires by mail to assess their self-reported degree of postoperative palmar sweating and compensatory sweating, as well as their level of satisfaction. Of the 92 patients who responded to the questionnaire, 54 had undergone sympathotomy by cutting (cutting group) and 38 by clamping (clamping group).
Results
The degree of postoperative palmar sweating was significantly lower in the cutting group than in the clamping group. However, compensatory sweating was significantly more severe in the cutting group than in the clamping group. No significant difference was observed in the degree of patient satisfaction between the groups.
Conclusions
Sympathotomy by clamping at T3 was less effective in reducing the primary symptom of postoperative palmar sweating, but induced less compensatory sweating than did sympathotomy by cutting at T3. However, both methods were similar with regard to patient satisfaction. The degree of postoperative palmar sweating and the severity of compensatory sweating were inversely correlated with the degree of patient satisfaction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although endoscopic thoracic sympathectomy (removal of sympathetic chain and/or ganglion)/sympathotomy (interruption of sympathetic chain without removing ganglion) for the treatment of palmar hyperhidrosis is associated with high success rate and low morbidity, postoperative compensatory sweating remains an occasional, but bothersome, side effect [1–5]. Recently, there has been an increasing consensus that limiting the extent of sympathectomy/sympathotomy using the clamping method minimizes the risk of severe compensatory sweating and, hence, maximizes patient satisfaction [1, 4, 6]. Currently, the best surgical method to use for sympathectomy/sympathotomy, either cutting or clamping, remains controversial despite the fact that both methods have good results if the level of division is correctly achieved [6–10].
The object of this study was to compare the effects of sympathotomy by cutting and the effects of sympathotomy by clamping on postoperative palmar sweating, compensatory sweating, and patient satisfaction when the sympathotomy is restricted to the T3 level in patients with palmar hyperhidrosis. We also evaluated associations among postoperative outcomes.
Materials and methods
Surgical procedure
The procedure was performed with the patient under general anesthesia in the semi-seated position and with arms abducted. A double-lumen endotracheal intubation was used to deflate the lung on the operative side. A 5-mm trocar was inserted at the anterior axillary line, in the fifth intercostal space, for thoracoscopy. Another 5-mm trocar for the endoscopic applier was inserted at the mid-axillary line, in the second or third intercostal space. Under real-time video guidance, the parietal pleura over the correspondent sympathetic chain was opened with the hooked diathermy probe. The sympathetic chain was either transected completely or clamped by a clip at the T3 level (sympathotomy). Transection was performed with electrocautery, at the T3 rib bed, and an autosuture endoscopic clip was placed above or below the T3 rib using the 5-mm endoclip applier (Fig. 1).
Participants
The participants in this study represented a consecutive series of 289 patients who underwent bilateral thoracoscopic sympathotomy at T3 for medically refractory palmar hyperhidrosis at the NTT Medical Center Tokyo between January 2004 and December 2010. Institutional review board approval was obtained before any data were collected. Data including sex, age, and surgical technique (cutting or clamping) were obtained from the clinical records.
In May 2013, the patients were asked to fill out questionnaires to assess operative outcomes after sympathotomy, such as the degree of postoperative palmar sweating, compensatory sweating, satisfaction with the procedure, and any other complications. Written informed consent was obtained from each patient before completing the questionnaire. The self-reported degree of postoperative palmar sweating was graded on a scale from 1 to 4 as follows: 1, dry; 2, mild; 3, moderate; and 4, complete recurrence. The severity of postoperative compensatory sweating reported by the patient was graded on a scale from 1 to 4 as follows: 1, no compensatory sweating; 2, occasional mild sweating; 3, frequent but not troublesome sweating; and 4, frequent and troublesome sweating that interferes with daily activities. The degree of patient satisfaction was also graded on a scale from 1 to 5 (1, dissatisfied and 5, very satisfied). The responders to the questionnaire were divided into two groups, depending on whether they received the cutting or clamping procedure.
Statistical analysis
The Mann–Whitney U test and χ 2 test were used to identify the differences between the two groups. The Spearman rank correlation was used to analyze all correlations (compensatory sweating, palmar sweating, and patient satisfaction). Differences were considered significant at p < 0.05. Results were expressed as mean ± standard deviation values.
Results
No conversion to an open surgical technique was necessary during the procedure, and there were no cases of operative mortality. Moreover, there were no patients who experienced pneumothorax requiring postoperative chest-tube drainage. In all patients, bilateral palmar sweating improved by the next day after the procedure.
Ninety-two patients (31.8 %) responded to our questionnaire. The demographic data of the patients are listed in Table 1. Of the 92 patients, 54 underwent cutting of the sympathetic chain at T3 (cutting group) and 38 underwent clamping of the sympathetic chain at T3 (clamping group).
The two groups were similar with regard to gender distribution and response rate to the questionnaire but differed with regard to mean age and follow-up period. The follow-up period appeared longer in the cutting group; this may be because we used the clamping technique more frequently over time, such that many of the cutting procedures were done prior to the clamping procedures. Patients in the clamping group were, on an average, younger compared to those in cutting group.
The incidence of postoperative compensatory sweating in the cutting group was significantly higher than that in the clamping group (96.2 and 84.2 %, respectively). However, whereas no patient in the cutting group had complete recurrence of palmar sweating, 5 patients (13.1 %) in the clamping group did exhibit complete recurrence of symptoms. There were no significant differences with regard to the incidence of gustatory sweating, dysgeusia, transient slightly ptosis, or postoperative persisting pain between the two groups (Table 2).
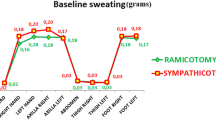
Postoperative outcomes are shown in Fig. 2. The degree of postoperative palmar sweating was significantly lower in the cutting group (1.8 ± 0.8) than in the clamping group (2.3 ± 0.9). However, postoperative compensatory sweating was significantly more severe in the cutting group (3.3 ± 0.8) than in the clamping group (2.7 ± 1.0). No significant difference in the degree of patient satisfaction was observed between the cutting (2.0 ± 1.0) and clamping groups (2.2 ± 1.0). However, the percentage of patients with lowest score of satisfaction (dissatisfied) was significantly higher in the cutting group (5.5 %) than in the clamping group (0 %). Not surprisingly, the degree of postoperative palmar sweating was inversely correlated with the degree of patient satisfaction (R = −0.26). A significant inverse correlation was similarly obtained between the severity of postoperative compensatory sweating and the degree of patient satisfaction (R = −0.36; Fig. 3).
Discussion
The present results demonstrate that bilateral sympathotomy by cutting at T3 reduced postoperative palmar sweating to a significantly greater degree than did sympathotomy by clamping at T3. In contrast, compensatory sweating after sympathectomy by cutting was significantly more severe than that experienced after sympathotomy by clamping.
Several authors have suggested that limiting the extent of sympathectomy/sympathotomy results in a lower incidence or severity of compensatory sweating and leads to increased patient satisfaction [3–5, 11]. With respect to patient satisfaction, the results of a meta-analysis also favored sympathectomy/sympathotomy at a single level [8]. Recently, several reports and reviews demonstrated that performing sympathectomy/sympathotomy at the T2 or T3 yields an excellent result for palmar hyperhidrosis and minimizes the risk of severe compensatory sweating [4, 7, 8, 12, 13]. Sympathectomy/sympathotomy at T4 alone is an acceptable treatment of palmar hyperhidrosis, but its efficacy is reduced. For these reasons, sympathectomy/sympathotomy at T2 or T3 alone is the recommended surgical treatment for patients with palmar hyperhidrosis [7, 12]. Based on this evidence, we have recently performed sympathotomy for palmar hyperhidrosis mainly at the T3 level.
Recent studies comparing the effects of sympathotomy at the T3 level by cutting or by clamping on postoperative palmar sweating, compensatory sweating, and patient satisfaction demonstrated that the two methods were comparable in terms of effectiveness and side effects [6, 9]. In contrast, our data showed that the degree of postoperative palmar sweating in the cutting group was lower than that in the clamping group and that compensatory sweating was more severe in the cutting group than in the clamping group. These differences may be explained by differences in the number of clips used in the clamping procedure to interrupt the sympathetic chain. In procedures used in previous studies, two clips were placed across the sympathetic chain near the third and fourth ribs [6, 9]. In contrast, we used one clip above or below the third rib, which might have resulted in a weaker interruption of the sympathetic chain.
The most important factor influencing postoperative patient satisfaction is known to be postoperative compensatory sweating, which interferes with patients’ quality of life and causes patient dissatisfaction [6, 14]. In the present study, a significant inverse correlation was observed between the severity of compensatory sweating and the degree of patient satisfaction, and then all the patients who felt dissatisfied with the cutting group complained of severe compensatory sweating. Previous studies have similarly demonstrated that the degree of patient satisfaction was significantly inversely related to the severity of compensatory sweating after sympathectomy/sympathotomy [15, 16].
The time elapsed after surgery and the recurrence of palmar sweating are the other important factors that negatively influence postoperative patient satisfaction [2, 14]. In fact, older age is associated with increased compensatory sweating [4, 17], which may indirectly decrease patient satisfaction. In the present study, the cutting group had more severe compensatory sweating, a longer follow-up time after surgery, and older mean age than the clamping group. However, no significant difference in the degree of patient satisfaction was observed between the cutting and clamping groups, possibly due to the greater recurrence of palmar sweating in the clamping group canceling out the adverse effect of increased compensatory sweating in the cutting group.
The main advantage of sympathotomy by clamping as an alternative method to cutting is its reversibility. Clip removal can be performed if severe compensatory sweating occurs and the patient is unsatisfied with the results. Although the beneficial effect of clip removal is not entirely assured, this method provides the possibility of reversing compensatory sweating in these patients [6, 9, 10]. In our series, none of the patients needed clip removal. Eight patients (21 %) in the clamping group had severe compensatory sweating, but none of them regretted undergoing the procedures because they were satisfied with the decrease of palmar sweating. On the basis of the findings of this study, we recommend thoracic sympathotomy by clamping at T3 rather than that by cutting for the treatment of refractory palmar hyperhidrosis.
This present study had two limitations. First, it was a retrospective study based on a questionnaire rather than a direct medical evaluation. On the other hand, this type of assessment has the merit that it allows patients to provide self-reported data in an environment free from medical influence [18]. Second, the response rate in this survey was very low (31.8 %). A low percentage of patient responses sometimes affects statistical accuracy and reduces the validity of the results obtained. We assume that this low response rate resulted from changes in the addresses of these mostly young patients and to the long follow-up time. However, there is also a possibility that patients were less likely to reply if they were dissatisfied with the sympathotomy. While recognizing this as a potential concern, we do not believe that this could significantly affect the validity of our results, since there was no significant difference in the response rate between the cutting and clipping groups and because responders were demographically similar to non-responders in terms of age, gender distribution, and follow-up period.
In conclusion, thoracic sympathotomy by clamping at T3 reduced postoperative palmar sweating in patients with palmar hyperhidrosis, but to a lesser degree, than did thoracic sympathotomy by cutting at T3; however, postoperative compensatory sweating was less severe in patients treated with the clamping method. Nevertheless, both methods were similar in terms of patient satisfaction. The degree of postoperative palmar sweating and the severity of postoperative compensatory sweating were inversely correlated with the degree of patient satisfaction.
References
Sugimura H, Spratt EH, Compeau CG, Kattail D, Shargall Y (2009) Thoracoscopic sympathetic clipping for hyperhidrosis: long-term results and reversibility. J Thorac Cardiovasc Surg 137:1370–1377
Rodríguez PM, Freixinet JL, Hussein M, Valencia JM, Gil RM, Herrero J, Caballero-Hidalgo A (2008) Side effects, complications and outcome of thoracoscopic sympathectomy for palmar and axillary hyperhidrosis in 406 patients. Eur J Cardiothorac Surg 34:514–519
Licht PB, Pilegaard HK (2004) Severity of compensatory sweating after thoracoscopic sympathectomy. Ann Thorac Surg 78:427–431
Miller DL, Bryant AS, Force SD, Miller JI Jr (2009) Effect of sympathectomy level on the incidence of compensatory hyperhidrosis after sympathectomy for palmar hyperhidrosis. J Thorac Cardiovasc Surg 138:581–585
Li X, Tu YR, Lin M, Lai FC, Chen JF, Dai ZJ (2008) Endoscopic thoracic sympathectomy for palmar hyperhidrosis: a randomized control trial comparing T3 and T2–4 ablation. Ann Thorac Surg 85:1747–1751
Yanagihara TK, Ibrahimiye A, Harris C, Hirsch J, Gorenstein LA (2010) Analysis of clamping versus cutting of T3 sympathetic nerve for severe palmar hyperhidrosis. J Thorac Cardiovasc Surg 140:984–989
Cerfolio RJ, De Campos JR, Bryant AS, Connery CP, Miller DL, DeCamp MM, McKenna RJ, Krasna MJ (2011) The Society of Thoracic Surgeons expert consensus for the surgical treatment of hyperhidrosis. Ann Thorac Surg 91:1642–1648
Deng B, Tan QY, Jiang YG, Zhao YP, Zhou JH, Ma Z, Wang RW (2011) Optimization of sympathectomy to treat palmar hyperhidrosis: the systematic review and meta-analysis of studies published during the past decade. Surg Endosc 25:1893–1901
Findikcioglu A, Kilic D, Hatipoglu A (2014) Is clipping superior to cauterization in the treatment of palmar hyperhidrosis? Thorac Cardiovasc Surg 62:445–449
Fibla JJ, Molins L, Mier JM, Vidal G (2009) Effectiveness of sympathetic block by clipping in the treatment of hyperhidrosis and facial blushing. Interact CardioVasc Thorac Surg 9:970–972
Yano M, Kiriyama M, Fukai I, Sasaki H, Kobayashi Y, Mizuno K, Haneda H, Suzuki E, Endo K, Fujii Y (2005) Endoscopic thoracic sympathectomy for palmar hyperhidrosis: efficacy of T2 and T3 ganglion resection. Surgery 138:40–45
Atkinson JL, Fode-Thomas NC, Fealey RD, Eisenach JH, Goerss SJ (2011) Endoscopic transthoracic limited sympathotomy for palmar-plantar hyperhidrosis: outcomes and complications during a 10-year period. Mayo Clin Proc 86:721–729
Katara AN, Domino JP, Cheah WK, So JB, Ning C, Lomanto D (2007) Comparing T2 and T2–T3 ablation in thoracoscopic sympathectomy for palmar hyperhidrosis: a randomized control trial. Surg Endosc 21:1768–1771
De Campos JR, Kauffman P, Werebe EC, Andrade Filho LO, Kusniek S, Wolosker N, Jatene FB (2003) Quality of life, before and after thoracic sympathectomy: report on 378 operated patients. Ann Thorac Surg 76:886–891
Chang YT, Li HP, Lee JY, Lin PJ, Lin CC, Kao EL, Chou SH, Huang MF (2007) Treatment of palmar hyperhidrosis: T4 level compared with T3 and T2. Ann Surg 246:330–336
Aoki H, Sakai T, Murata H, Sumikawa K (2014) Extent of sympathectomy affects postoperative compensatory sweating and satisfaction in patients with palmar hyperhidrosis. J Anesth 28:210–213
Baumgartner FJ, Reyes M, Sarkisyan GG, Iglesias A, Reyes E (2011) Thoracoscopic sympathicotomy for disabling palmar hyperhidrosis: a prospective randomized comparison between two levels. Ann Thorac Surg 92:2015–2019
Dumont P, Denoyer A, Robin P (2004) Long-term results of thoracoscopic sympathectomy for hyperhidrosis. Ann Thorac Surg 78:1801–1807
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hida, K., Sakai, T., Hayashi, M. et al. Sympathotomy for palmar hyperhidrosis: the cutting versus clamping methods. Clin Auton Res 25, 271–276 (2015). https://doi.org/10.1007/s10286-015-0293-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-015-0293-y