Abstract
The management of a newborn with pure oesophageal atresia continues to be challenging. We started treating babies with pure oesophageal atresia by delayed primary anastomosis in 1977. The purpose of this study was to review the long-term outcome in infants with pure oesophageal atresia (EA) treated by delayed primary anastomosis with special emphasis on gastroesophageal reflux (GOR) related morbidity. The medical charts of all patients treated by delayed primary anastomosis between 1977 and 2004 were retrospectively reviewed. All survivors were followed up with completion of a questionnaire and personal/phone interviews. There were 26 patients in total admitted during the 27-year study period with the diagnosis of pure oesophageal atresia. Three died prior to surgery due to associated anomalies; two had almost no distal oesophageal segment and underwent oesophageal replacement surgery. The remaining 21 children were treated with delayed primary anastomosis and made up our study group. There were four deaths (19%) in this group, and all were prior to 1980. The median gestational age was 35.5 weeks and the median birth weight was 2.6 kg; median initial gap was 3.7 cm and median preoperative gap was 1.5 cm; median age at operation was 80 days and the median hospital stay was 5.5 months. The median follow-up period was 13.5 years. Fourteen children (66%) developed symptomatic gastroesophageal reflux and nine of these needed fundoplication (43%). Sixteen children developed strictures at the anastomotic site; ten responded to repeated dilatations while six needed resection and reanastomosis. At the time of this study, 15 out of the 17 survivors (88%) were on normal diet with no respiratory problems and 2 (12%) were dependent on gastrostomy feeds. Our long-term follow-up data shows that the delayed primary anastomosis provides excellent functional results in patients born with pure oesophageal atresia. The high incidence of gastroesophageal reflux and associated morbidity requires early intervention to prevent ongoing feeding problems due to oesophagitis and stricture formation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
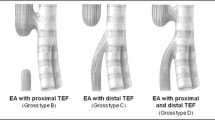
Pure oesophageal atresia (EA) without tracheoesophageal fistula is an uncommon anomaly with an estimated incidence of 1 in 40,000 live births [1]. In newborn with pure EA the oesophageal segments are usually too fart apart to permit an immediate primary anastomosis. It is commonly accepted that the child’s own oesophagus is infinitely better than any replacement that can be constructed [2]. During the past four decades, several methods have been employed to overcome the technical difficulties encountered in bringing the two oesophageal segments together [3–7].
In 1977 we started treating babies with pure oesophageal atresia by delayed primary anastomosis, and in 1981 reported our early experience in five cases treated between 1977 and 1979 [8]. We later reported our short-term follow-up results in 1998 [9]. The purpose of this study was to review our long-term outcome in infants with pure oesophageal atresia (EA) treated by delayed primary anastomosis with special emphasis on gastroesophageal reflux (GER) related morbidity.
Materials and methods
First part of the study consisted of a retrospective review of medical records of all patients with pure EA treated with delayed primary anastomosis from the two neonatal surgical centres in Ireland from 1977 to 2004. The initial management of the newborn with pure EA and the technique used to measure the gap between the two oesophageal segments are well standardized at our institutions and has been reported previously [8, 10]. Data examined included: sex, gestational age, birth weight, Apgar scores, maternal history of polyhydramnios, associated anomalies, age when gastrostomy was performed, gap size at initial assessment (1–2 weeks post gastrostomy), follow-up gap size (assessed every 2–3 weeks), age at delayed primary anastomosis, whether circular myotomy or upper pouch elongation was performed, duration of postoperative ventilatory support and paralysis, immediate complications and management, late complications and management, time when gastrostomy feeds were stopped, hospital stay and mortality.
Second part of the study consisted of follow-up by completion of a questionnaire and personal or telephone interview with all the surviving patients or their parents. Data collected by the questionnaire included: present weight and height, mode of feeding, symptoms related to gastroesophageal reflux or strictures, use of gastrostomy, mental developmental status, and frequency of respiratory infections, any need for bougienage and other unrelated medical concerns.
Results
There were 26 patients in total admitted during the 27-year study period (1977–2004) with the diagnosis of pure oesophageal atresia. Three died prior to surgery due to major associated anomalies. Two others were noted to have only a very small nub of oesophageal tissue and underwent oesophageal replacement surgery. All these five children were excluded from this study. Sixty-eight percent of the patients had associated anomalies (Table 1).
Delayed primary anastomosis was successful in all the remaining 21 children (11 males and 10 females). There was positive maternal history of polyhydramnios in ten children (48%). Median Apgar scores were six at 1 min and nine at 5 min. Sixty-two percent of the patients had associated anomalies (Table 1). Gastrostomy was performed on day 1 to 3 of life. The median gestational age was 35.5 weeks (range 28–42 weeks) and the median birth weight was 2.6 kg (range 1.2–3 kg); median initial gap was 3.7 cm (range 2.5–5.5 cm) and median preoperative gap was 1.5 cm (range 0.5–2.5 cm)(Figs. 1, 2); median age at delayed primary anastomosis was 80 days (range 35–270 days) and the median hospital stay was 5.5 months (range 2–14 months). The median follow-up period was 13.5 years (range 28 months to 27 years). Gastrostomy feeds were stopped after a median period of 50 days (range 14–255 days). Circular myotomy was performed in the first seven patients, and all remaining children had a single layer end-to-end anastomosis.
There were four deaths (19%), all prior to 1980, within this group. One girl had a cardiac arrest perioperatively requiring open heart massage. She developed pulmonary oedema and died of respiratory failure 3 months later. Autopsy in this child did not reveal an obvious cause of death, but a tracheal stenosis at the cricoid level and a poorly developed left main bronchus was noted. The second child, a girl, died 3 months post surgery with respiratory infection. Post-mortem examination in this child showed an ulcer in the gastric fundus that had eroded into the left pleural cavity causing collapse of the left lung and empyema; the calibre of the oesophagus was noted to be normal. The third child, who had successfully undergone resection and reanastomosis of her oesophageal stricture, died at 15 months of age due to unrelated causes. Autopy on this child showed a normal calibre oesophagus. The fourth child was a boy, who developed an anastomotic leak on fifth postoperative day. A cervical oesophagostomy was fashioned, but he died after an episode of aspiration, one week after discharge from the hospital. Autopsy confirmed death due to aspiration.
Sixteen out of 21 children in the study group (76%) developed a stricture at some stage necessitating multiple dilatations (between 2 and 17 dilatations over a period of up to 2 years) in all. If the children became symptomatic within 2–3 weeks of a dilatation or the diameter is noted to be decreasing, it is considered to be a failure, and resection anastomosis was planned. Nine of these strictures were associated with GOR, and all these children had fundoplication as part of their management. Six children with strictures (28.5%) failed to respond to dilatations alone, and needed resection–reanastomosis between 8 months and 5.5 years after the original surgery. Two of these strictures that needed resections were from the fundoplication group. Severe oesophageal motility disturbances were noticed on follow-up contrast study in 7 patients (33%). Four of these seven patients had circular myotomy at the time of their primary surgery.
Two children (9.5%) underwent ligation of an initially undiagnosed proximal pouch fistula at 2 and 4 months after their initial operation. They were repaired using a right-sided cervical approach. Aortopexy was performed for persistent tracheomalacia in two patients (9.5%) 6 months after delayed primary anastomosis.
Fourteen children (66%) developed symptomatic gastroesophageal reflux (GOR) and nine of these needed fundoplication (43%) at 3 months to 9 years after the initial anastomosis. Five of the fundoplication group were noted to have an associated hiatus hernia. In 2 children (9.5%) Barrett’s oesophagus had been diagnosed at 7 and 16 years after their initial surgery, respectively. The GOR symptoms persisted in one patient after a Thal fundoplication, and a Nissen fundoplication was carried out 6 months later. In another child the Nissen fundoplication wrap became undone and slid into a paraesophageal hernia over a period of 16 years. In this child, the hernia was repaired and a redo Nissen fundoplication was performed. Only one child with an initial gap length of 2.5 cm developed no subsequent problems.
At the time of this study, 15 out of the 17 surviving children (88%) were on normal diet with no respiratory problems and had no dietary restrictions (Fig. 3). One 26-year-old Down’s syndrome patient with severe mental handicap and another 5-year-old boy with significant oral food aversion were dependent on gastrostomy feeds. The latter child is on oral stimulation program. The median weight in the 17 survivors was at 20th percentile (range <P3 to P50) and the median height at 50th centile (<P3 to P90).
Discussion
Managing a newborn with pure EA remains a surgical challenge for most paediatric surgeons because it is nearly always associated with a long gap between the two segments. Moreover, the associated anomalies and high incidence of prematurity complicates the care of these children [11]. Earlier management options consisted of an early creation of a cervical oesophagostomy, a feeding gastrostomy, and a delayed oesophageal replacement with colon, stomach or gastric tube [12–15].
In 1977 we started treating babies with pure oesophageal atresia by delayed primary anastomosis, and in 1981 reported our early experience in five cases treated between 1977 and 1979 [8]. This was based on the observation that spontaneous growth and hypertrophy of the oesophageal segments in pure oesophageal atresia occurs at a rate faster than overall somatic growth in the absence of any form of mechanical stretching. This is believed to be the result of the swallowing reflex on the upper pouch and reflux of gastric contents into the lower pouch. It was also noted that the maximal natural growth of oesophageal segments occurred during the first 8–12 weeks of life, and this correlated usually with a doubling of the birth weight. Subsequent investigators have confirmed these observations [16, 17]. In 1994 Ein et al. [17] reported that the delayed primary anastomosis had the best long-term outcome compared to all other previously adopted techniques.
Though oesophageal continuity is achieved by all the various techniques, mobilizing the stomach into the thorax results in displacement of the gastroesophageal junction into the chest, leading to a persistent GOR and strictures in virtually all cases [18–20]. Long-term complications also are described with these techniques [21, 22]. The best management in children with long gap EA is still undetermined, but children whose oesophagus is preserved seem to have a better long-term outcome in relation to swallowing and GOR related symptoms [18]. At present, most paediatric surgeons agree that delayed oesophageal anastomosis with an end-to-end anastomosis is the procedure of choice in the management of pure EA as it offers the most physiological reconstruction possible [16, 23, 24].
Since 1977, we have accomplished delayed primary anastomosis in all children, except in two cases with very small distal pouch, in our institutions and, thus, have avoided oesophageal replacement. Although delayed primary anastomosis is feasible in the majority of children with pure EA, GOR and its complications have been recognized as a major source of morbidity [2, 10, 11, 16]. GOR has been diagnosed in 66% of the patients in our series and the majority of these required fundoplication to improve their symptoms. This is slightly higher than the reported incidence in the literature [2, 10, 11, 16]. Barrett’s oesophagus was seen in two of our children, and has been reported by others following surgery for EA with or without fistula [25, 26]. Both of these patients had fundoplication and are being followed-up regularly with endoscopic surveillance.
The incidence of strictures in our series was 76%, and those needing resection was 28%. We recommend early fundoplication for GOR symptoms, particularly when there is any anastomotic stricture is noted. As long as reflux is not dealt with, the child will continue to suffer from oesophagitis and subsequent recurrent strictures. GOR regularly is the cause of inhalation of gastric contents with secondary bronchial spasm, pneumonia and long-term bronchopulmonary dysplasia. Whether symptoms of GOR may have contributed to food refusal and food aversion in one child cannot be decided upon from our study. Similarly, whether circular myotomy is partly the cause of the motility disturbances seen or not is also unknown. Other authors have suggested that all esophageal atresias have abnormal motility in the lower segment in the past [27, 28].
Pure oesophageal atresia is a congenital defect with significant associated morbidity, and this is highlighted by the fact that only 1 child with an initial gap length of 2.5 cm developed no subsequent problems in our series. Despite the high incidence of GOR and its associated complications in the immediate postoperative period, this study shows that the long-term outcome in this specialised group of children who were managed with delayed primary anastomosis is satisfactory. At a median follow-up period of 13.5 years, 90% of our children were able to eat any item they desired orally with very acceptable growth parameters. However, complications such as Barrett’s oesophagus highlight the need for continued long-term follow-up for these children.
References
Manning PB (1994) Long-gap esophageal atresia. Semin Thorac Cardiovasc Surg 6:216–220
Lindahl H, Rintala R, Louhimo I (1987) Oesophageal anastomosis without bougienage in isolated atresia—do the segments really grow while waiting? Z Kinderchir 42:221–223
Lafer DJ, Boley SJ (1966) Primary repair in esophageal atresia with elongation of the lower segment. J Pediatr Surg 1:585–587
Rehbein F, Schweder N (1971) Reconstruction of the esophagus without colon transplantation in cases of atresia. J Pediatr Surg 6:746–752
Shafer AD, David TE (1974) Suture fistula as a means of connecting upper and lower segments in esophageal atresia. J Pediatr Surg 9:669–673
Thomasson BH (1972) Congenital esophageal atresia: mercury bag stretching of the upper pouch in a patient without tracheoesophageal fistula. Surgery 71:661–663
Hendren WH, Hale JR (1976) Esophageal atresia treated by electromagnetic bougienage and subsequent repair. J Pediatr Surg 11:713–722
Puri P, Blake N, O’Donnell B, Guiney EJ (1981) Delayed primary anastomosis following spontaneous growth of esophageal segments in esophageal atresia. J Pediatr Surg 16:180–183
Puri P, Khurana S (1998) Delayed primary esophageal anastomosis for pure esophageal atresia. Semin Pediatr Surg 7:126–9
Puri P, Ninan GK, Blake NS, Fitzgerald RJ, Guiney EJ, O’Donnell B (1992) Delayed primary anastomosis for esophageal atresia: 18 months’ to 11 years’ follow-up. J Pediatr Surg 27:1127–1130
Chahine AA, Ricketts RR (2000) Esophageal atresia in infants with very low birth weight. Semin Pediatr Surg 9:73–78
Stone MM, Fonkalsrud EW, Mahour GH, Weitzman JJ, Takiff H (1986) Esophageal replacement with colon interposition in children. Ann Surg 203:346–351
West KW, Vane DW, Grosfeld JL (1986) Esophageal replacement in children: experience with thirty-one cases. Surgery 100:751–757
Ahmed A, Spitz L (1986) The outcome of colonic replacement of the esophagus in children. Prog Pediatr Surg 19:37–54
Spitz L (1992) Gastric transposition for esophageal substitution in children. J Pediatr Surg 27:252–257; discussion 257–259
Boyle EM Jr, Irwin ED, Foker JE (1994) Primary repair of ultra-long-gap esophageal atresia: results without a lengthening procedure. Ann Thorac Surg 57:576–579
Ein SH, Shandling B (1994) Pure esophageal atresia: a 50-year review. J Pediatr Surg 29:1208–1211
Maksoud-Filho JG, Goncalves ME, Tannuri U, Maksoud JG (2002) An exclusively intraabdominal distal esophageal segment prevents primary delayed anastomosis in children with pure esophageal atresia. J Pediatr Surg 37:1521–1525
Foker JE, Linden BC, Boyle EM Jr, Marquardt C (1997) Development of a true primary repair for the full spectrum of esophageal atresia. Ann Surg 226:533–541; discussion 541–533
Guo W, Fonkalsrud EW, Swaniker F, Kodner A (1997) Relationship of esophageal anastomotic tension to the development of gastroesophageal reflux. J Pediatr Surg 32:1337–1340
Davenport M, Hosie GP, Tasker RC, Gordon I, Kiely EM, Spitz L (1996) Long-term effects of gastric transposition in children: a physiological study. J Pediatr Surg 31:588–593
Lindahl H, Rintala R, Sariola H, Louhimo I (1990) Cervical Barrett’s esophagus: a common complication of gastric tube reconstruction. J Pediatr Surg 25:446–448
Varjavandi V, Shi E (2000) Early primary repair of long gap esophageal atresia: the VATER operation. J Pediatr Surg 35:1830–1832
Howell CG, Davis JB Jr, Parrish RA (1987) Primary repair of esophageal atresia: how long a gap? J Pediatr Surg 22:42–43
Lindahl H, Rintala R, Sariola H (1993) Chronic esophagitis and gastric metaplasia are frequent late complications of esophageal atresia. J Pediatr Surg 28:1178–1180
Somppi E, Tammela O, Ruuska T, Rahnasto J, Laitinen J, Turjanmaa V, Jarnberg J (1998) Outcome of patients operated on for esophageal atresia: 30 years’ experience. J Pediatr Surg 33:1341–1346
Cumming WA (1975) Esophageal atresia and tracheoesophageal fistula. Readiol Clin North Am 13:277–95
Desjardins JG, Stephens CA, Moes CAF (1964) Results of surgical treatment of congenital tracheoesophageal fistula, with note on cine-fluorographic findings. Ann Surg 160:141–145
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sri Paran, T., Decaluwe, D., Corbally, M. et al. Long-term results of delayed primary anastomosis for pure oesophageal atresia: a 27-year follow up. Pediatr Surg Int 23, 647–651 (2007). https://doi.org/10.1007/s00383-007-1925-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-007-1925-7