Abstract
Purpose
To evaluate long-term outcomes of pure esophageal atresia (EA) repair with preservation of native esophagus.
Methods
Infants with pure EA treated at our institution (2000–2010) and with minimum 5-year follow-up were reviewed (REB:1000046653). Data analysed included demographics, management and outcomes and are reported as mean ± SD/median (range).
Results
Of 185 infants with EA, 12 (7 %) had pure EA (gestational age: 36 ± 2.4 weeks, birth weight: 2353 ± 675 g). Ten had associated anomalies, including trisomy-21 (n = 2) and duodenal atresia (n = 1). Surgery: 1 patient (short gap) underwent primary thoracoscopic anastomosis, 11 had gastrostomy (Stamm, n = 5; image-guided, n = 6) as initial procedure. At definitive repair (age: 128 ± 91 days; weight 5.5 ± 2.3 kg): ten had primary anastomosis and 1 had Collis gastroplasty. No patient had esophageal replacement surgery. Outcomes: three patients had gastrostomy dehiscence requiring re-operation. At post-operative esophagram, seven had anastomotic leak successfully treated conservatively. Seven patients developed strictures requiring balloon dilatations (median two dilatations, range 1–10), six received antireflux surgery. At 7-year follow-up (range 5–15 years), all patients had the gastrostomy closed and were on full oral feeds.
Conclusions
The management of pure EA continues to be challenging. The preservation of native esophagus is possible with significant morbidity. The long-term outcomes are favourable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
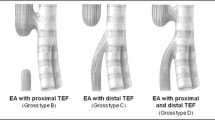
Pure or isolated esophageal atresia (EA) is a rare congenital condition characterized by a gap between two esophageal stumps and absence of a tracheoesophageal fistula [1]. This anomaly corresponds to type A of the Gross classification of EA anatomic patterns [2]. Commonly, the esophageal gap is long such that initial surgical repair by primary anastomosis is difficult. The general consensus is that preservation of the native esophagus should be attempted whenever possible [3–6]. Although the prognosis for these infants has improved over the last decades [7, 8], the management of pure EA still remains challenging. In 1994, Ein and Shandling reported the evolution over five decades (1942–1991) of the surgical treatment of infants with pure EA at The Hospital for Sick Children [8]. The authors reported that the survival rate for pure EA increased from 0 % in the 1940s to 100 % in the 1990s, mainly due to the timing of the procedure, which in the 1990s was delayed primary anastomosis [7, 8]. The aim of the present study is to review the management of pure EA at The Hospital for Sick Children in the third millennium, and to evaluate the post-operative morbidity and long-term outcomes of patients with pure EA who underwent repair with preservation of native esophagus.
Methods
Following ethical approval (REB:1000046653), the clinical charts of all infants with pure EA treated between 2000 and 2010 at our institution were analysed. Only patients with a minimum 5 years’ follow-up were included in the study. Patient demographics, surgical management, and postoperative and long-term outcomes morbidity were reviewed.
Data were reported as mean ± SD or median (range) as appropriate.
Results
During the study period, 185 infants with EA were treated at our institution. Of these, 12 (7 %) neonates were born with pure EA.
Demographics
Seven (58 %) were males. At antenatal screening, nine (75 %) infants had polyhydramnios and absent stomach and one showed a double bubble which proved later to be due to duodenal atresia. The mean gestational age was 36 ± 2.4 weeks and the mean birth weight was 2353 ± 675 g. Associated anomalies were present in 10 (83 %) infants. These included cardiac (n = 7; 58 %), vertebral (n = 2; 17 %), anorectal (n = 1; 8 %), renal (n = 1; 8 %), duodenal atresia (n = 1; 8 %), trisomy-21 (n = 2; 17 %), limb (n = 2; 17 %) and neurological (n = 1; 8 %) anomalies.
Surgery
One (8 %) patient with a birth weight of 3 kg and a radiological appearance of short gap (<2 vertebral bodies) underwent an early primary thoracoscopic anastomosis at 12 days of age (Fig. 1). At surgery, the two portions of esophagus were found to be very close so the anastomosis was successfully performed without complications.
The remaining 11 patients (delayed repair group) underwent gastrostomy as the initial procedure at a median age of 2 days (range 1–12 days). Of these, one patient at the time of gastrostomy simultaneously underwent duodeno-jejunostomy and colostomy for associated duodenal atresia and rectovestibular fistula. The gastrostomy was accomplished as Stamm surgical gastrostomy in five patients and as image-guided percutaneous gastrostomy in six. Image-guided percutaneous gastrostomy was technically unsuccessful in one patient who required an open Stamm gastrostomy. There were 3 (27 %) post-operative dehiscences of the gastrostomy tract (two after Stamm gastrostomy) resulting in peritonitis requiring laparotomy and re-do gastrostomy. One patient underwent elongation of esophageal ends by traction (Foker procedure) and gastrostomy as initial procedures. Traction started on day 3 but by day 4 no resistance on the sutures was felt so that the traction was stopped.
In the delayed repair group, 1 (9 %) patient had an episode of apnea and bradycardia and 1 (9 %) had multiple episodes of aspiration while awaiting esophageal anastomosis. Three (25 %) patients were managed at home using portable suction equipment before the esophageal repair. At definitive repair, the mean age was 128 ± 91 days and mean weight 5.5 ± 2.3 kg. Initial gap length was 4 (range 0–5) vertebral bodies and pre-operative gap length was 2.5 (range 0–5) vertebral bodies.
Ten (83 %) patients underwent delayed primary anastomosis (one following Foker procedure failure), one using a thoracoscopic approach. Lower pouch dissection to the level of diaphragm was performed in 5 (50 %) patients and hiatal dissection in 4 (40 %). One patient with right aortic arch and patent ductus arteriosus (PDA) had a left thoracotomy, PDA closure and esophageal anastomosis; during the proximal pouch dissection a small hole on the trachea was made and repaired. One patient with extremely small lower esophagus underwent a delayed Collis gastroplasty. No patient required an esophageal replacement.
During the post-operative period, 7 (58 %) patients had an anastomotic leak, with all successfully managed non-operatively with antibiotic and chest tube drainage. The chest tube was removed after a median of 14 days (range 11–65 days). One patient had an esophageal stent inserted which was removed after 37 days. Three patients had the temporary gastrostomy tube advanced to become a gastro-jejunostomy. The patient who had the Collis gastroplasty had a feeding jejunostomy created at the time of the esophageal repair and it was closed at 33 months of age. The average duration of hospital stay was 4.1 ± 2.3 months.
Outcomes
Seven (58 %) patients developed esophageal strictures requiring multiple dilatations (median 2; range 1–10). Of the nine (75 %) patients with clinically significant gastroesophageal reflux (GER), six (50 %) underwent antireflux surgery (Nissen, n = 2; Toupet, n = 3; Thal, n = 1). One patient required pyloroplasty for delayed gastric emptying. Associated surgical procedures were required in six (50 %) patients including posterosagittal anorectoplasty (n = 1), orchidopexy (n = 2) and cardiac surgery (n = 3).
At a median follow-up of 7 years (5–15), all patients were alive. All children with gastrostomies had closure of the gastrostomy at a median of age of 16 months (range 6–72 months) and were on full oral feeds. Three (25 %) patients had weights <10th percentile, including one patient with liver cirrhosis secondary to autoimmune hepatitis. Gastrointestinal symptoms (severe dysphagia for solid foods, early satiety) were reported in 2 (17 %) children and respiratory problems (recurrent pneumonia, night-time coughing) in 2 (17 %). Two (17 %) patients with increasing dysphagia underwent endoscopy and biopsy and were diagnosed with eosinophilic esophagitis.
Discussion
The present study shows that although the management of pure EA continues to be challenging for paediatric surgeons, preservation of native esophagus is possible and their long-term outcomes are favourable.
Overall, our findings for the incidence and demographics of pure EA patients are in line with previously reported series. The incidence of pure EA in the present study (7 %) parallels the one collectively reported by Harmon and Coran in more than 2200 cases of EA from six large series (7.8 %) [1]. Likewise, the rate of prenatal ultrasound diagnosis of EA in our series (75 %) was very similar to that reported recently in a study from a tertiary care fetal center (78 %) [9]. It has been reported that associated anomalies are more common in cases of pure EA [1, 10]. This is confirmed in our series where 83 % of infants presented with at least one associated anomaly, which is a higher rate than the overall incidence of 50–70 % associated anomalies reported in the literature for other forms of EA [1], and than the 28 % of VACTERL association recently reported at our institution [11].
When a pure EA is diagnosed pre-operatively, a long gap between the two esophageal ends is assumed. Therefore, the surgical management of pure EA engages the same long-standing debate of the management of long-gap EA [1]. The classic approach is to proceed with the operative placement of a gastrostomy tube through which bolus feeds help to lengthen the distal esophageal end and increase the stomach size in the event that a Collis is required. After a period of observation, delayed primary repair is attempted [1]. The rationale for this delayed approach is that during the first months of life, the gap between the esophageal ends becomes shorter with growth, allowing for a shorter gap and primary repair [1, 7]. A recent international survey on the management of EA reported that the majority of surgeons manage pure EA by delayed primary anastomosis with gastrostomy formation without esophagostomy [12]. A meta-analysis on patients with long-gap EA managed by delayed primary anastomosis concluded that this approach provides good long-term functional results [13]. This confirms the findings from a previous study at our institution, which reported that the delayed primary esophageal repair had the best long-term results compared to other techniques [7]. The timing of the repair is variable according to surgeons and institutions. The conservative approach of waiting at least 3 months before attempting definitive repair allows the spontaneous elongation of the esophageal stumps and successful achievement of primary anastomosis [14]. Most surgeons responding to the international survey on EA perform the delayed primary anastomosis at 3 months of age [12], which corresponds to 11.9 weeks reported in the meta-analysis study [13], and is similar to the 4 months of age of our series.
In our series, all patients with EA and gasless abdomen received tube drainage of the proximal pouch using a Replogle tube without an esophagostomy. In addition, 25 % of patients were treated safely at home with Replogle drainage and gastrostomy feeds while awaiting definitive repair. Discharge from hospital to home management was considered, according to family social circumstances, when the child was stable and maintained on full enteral feeding by gastrostomy. As previously reported, this approach is successful in cases with motivated, reliable families, and adequate support from community health care providers [15].
Gastrostomy formation was the initial procedure in all our infants. The gastrostomy was fashioned either via an open surgical procedure (Stamm technique) or via image-guided percutaneous technique as previously reported [16], depending on surgeon preference and availability of the interventional radiologist. As the stomach of babies with pure EA is typically small, the complication rate in our series is not negligible regardless of the technique used: in three patients (two after Stamm), who experienced early gastrostomy dehiscence and peritonitis, a re-do open gastrostomy was required and in 1 patient the image-guided percutaneous gastrostomy was technically unsuccessful.
In pure EA, primary esophageal anastomosis should be considered in patients with a short gap, when the distance is estimated to be within two vertebral bodies [7, 17]. One patient in our series who underwent primary thoracoscopic repair had a favourable birth weight (3 kg) and was expected pre-operatively to have <2 vertebral bodies gap. Early primary thoracoscopic anastomosis was successfully performed in this patient without complications.
In this series, patients considered not suitable for primary anastomosis underwent a delayed primary repair, which was feasible in 92 % of cases with 100 % overall survival rate. At surgery, a fibrous cord-like segment connecting the two esophageal stumps was found in four patients and a tracheal diverticulum in one, thus confirming that the anatomy of pure EA can be variable as previously described [18, 19].
One of our patients underwent elongation of esophageal ends by traction (Foker procedure), which was abandoned after 4 days. The “growth induction” by traction described by Foker [20, 21] remains an attractive but controversial primary approach for long-gap EA. Other previous series of pure EA reported that the Foker procedure was unsuccessful [5, 6]. In a recent study, the Foker technique was reported to be successful in achieving a primary anastomosis in 80 % of the patients, but had a 75 % re-operation rate for strictures [22]. Thus, the Foker technique for long-gap EA remains a procedure for selected patients.
In the present series, only two patients underwent thoracoscopic repair. The minimally invasive approach was based on surgeon preference and gap length. Although some surgeons advocate the thoracoscopic approach even in long-gap EA [23, 24], the preferred approach for pure EA by the majority of the respondents to an international survey was open surgery [12]. Hence, thoracoscopic repair of long-gap EA remains an option for a highly selective cohort of patients and surgeons.
In the only case where a primary anastomosis was not possible, a Collis gastroplasty was performed. This patient at the age of 7 months had a pre-operative gap study showing an unvaried almost absent lower esophagus. This technique, originally described by Collis in 1957 for adult patients with hiatus hernia and a short esophagus [25], was employed as means of lengthening the distal stump to avoid esophageal replacement. The length of the lower esophagus is the key to success. In fact, in long-gap EA the distal esophagus can be dissected to the level of diaphragm and freed from the surrounding structures (hiatal dissection) to achieve an appropriate length for anastomosis [26]. Attempts to lengthen the proximal pouch by circular myotomy should be discouraged because of diverticula formation and esophageal motility disturbances [4, 6, 7, 13]. Alternatively, patients with an absent or extremely small lower esophagus are candidate for esophageal replacement [1, 4, 5, 13, 17], which can also include a laparoscopic assisted gastric transposition [5, 27].
Post-operative complications of primary esophageal anastomosis are typically leaks and strictures. In a meta-analysis of complications and long-term outcomes of delayed primary anastomosis for long-gap EA, the reported leak rate was 29 % and the stricture rate, 57 % [13]. In our series, the leak rate was higher (58 %), possibly because all patients received routinely a post-operative esophagram thus allowing the diagnosis of small but clinically insignificant leaks. In our series, all anastomotic leaks were managed conservatively with intravenous broad-spectrum antibiotic coverage, chest tube drainage and, in cases with significant GER, advancement of gastrostomy tube feeds to gastro-jejunostomy feeds to allow the spontaneous healing of the esophageal leak. The incidence of strictures in our series (58 %) was similar to the one reported in the meta-analysis study (58 %) [13]. All esophageal strictures responded to serial balloon dilatations, contrary to other series where resection and re-anastomosis were required [4, 6, 13]. This outcome may have been influenced by the routine administration of anti-gastro-esophageal reflux medications after repair of the atresia. Symptomatic GER may contribute to the formation of esophageal strictures, and in our series GER was diagnosed radiologically in 75 % of patients and fundoplication was performed in 50 %. The high incidence of GER in long-gap EA may be related to the extensive lower esophageal pouch dissection required to achieve adequate length to perform the anastomosis, resulting in the loss of the anatomic angle of His [4, 28].
In our institution, after hospital discharge, all EA infants are followed up in a multidisciplinary esophageal atresia clinic. At the 5-year follow-up, all patients have been able to achieve full oral feeding and the gastrostomy removed. Despite associated defects such as congenital heart anomalies and chromosomal abnormalities, 75 % of pure EA patients achieved satisfactory growth (>10th centile). These findings indicate that long-gap EA patients can maintain reasonable oral intake sufficient to sustain childhood growth despite the complexity of their condition.
In conclusion, patients with pure EA can be successfully treated with delayed primary anastomosis without esophagostomy and achieve good long-term functional results. In spite of a high post-operative morbidity, the survival rate is 100 % and esophageal replacement surgery could be avoided.
References
Harmon CM, Coran AG (1998) Congenital anomalies of the esophagus. In: St Louis KY (ed) Pediatric Surgery, vol 5. Elsevier Science Health Science Division, Oxford
Gross RE (1953) Surgery of infancy and childhood. WB Sauders, Philadelphia
Bagolan P, Iacobelli BD, De Angelis P et al (2004) Long gap esophageal atresia and esophageal replacement: moving toward a separation? J Pediatr Surg 39:1084–1090
Sri Paran T, Decaluwe D, Corbally M et al (2007) Long-term results of delayed primary anastomosis for pure oesophageal atresia: a 27-year follow up. Pediatr Surg Int 23:647–651
Holland AJA, Ron O, Pierro A et al (2009) Surgical outcomes of esophageal atresia without fistula for 24 years at a single institution. J Pediatr Surg 44:1928–1932
Burjonrappa S, Thiboutot E, Castilloux J et al (2010) Type A esophageal atresia: a critical review of management strategies at a single center. J Pediatr Surg 45:865–871
Ein SH, Shandling B, Heiss K (1993) Pure esophageal atresia: outlook in the 1990. J Pediatr Surg 28:1147–1150
Ein SH, Shandling B (1994) Pure esophageal atresia: a 50-year review. J Pediatr Surg 9:1208–1211
Kunisaki SM, Bruch SW, Hirschl RB et al (2014) The diagnosis of fetal esophageal atresia and its implications on perinatal outcome. Pediatr Surg Int 30:971–977
Holder TM, Cloud DT, Lewis JE Jr et al (1964) Esophageal atresia and tracheoesophageal fistula. A survey of its members by the Surgical Section of the American Academy of Pediatrics. Pediatrics 34:542–549
Zamiara P, Thomas KE, Connolly BL et al. (2015) Long-term burden of care and radiation exposure in survivors of esophageal atresia. J Pediatr Surg 50:1686–1690
Zani A, Eaton S, Hoellwarth M et al (2014) International survey on the management of esophageal atresia. Eur J Pediatr Surg 24:3–8
Friedmacher F, Puri P (2012) Delayed primary anastomosis for management of long-gap esophageal atresia: a meta-analysis of complications and long-term outcome. Pediatr Surg Int 28:899–906
Puri P, Blake N, O’Donnel B et al (1981) Delayed primary anastomosis following spontaneous growth of esophageal segments in esophageal atresia. J Pediatr Surg 16:180–183
Aziz D, Shiller D, Gerstle JT et al (2003) Can long-gap esophageal atresia be safely managed at home while awaiting anastomosis. J Pediatr Surg 5:705–708
Aziz D, Chait P, Kreichmn F et al (2004) Image-guided percutaneous gastrostomy in neonates with esophageal atresia. J Pediatr Surg 11:1648–1650
Spitz L (2006) Esophageal atresia. Lesson I have learned in a 40-year experience. J Pediatr Surg 41:1635–1640
Kluth D (1976) Atlas of esophageal atresia. J Pediatr Surg 11:901–919
Sanal M, Haeussler B, Tabareli W et al (2007) Pure esophageal atresia with normal outer appearance: case report. J Pediatr Surg 42:E1–E3
Foker JE, Linden BC, Boyle EM et al (1997) Development of a true primary repair for the full spectrum of esophageal atresia. Ann Surg 226:533–543
Foker JE, Kendall Krosch TC, Catton K et al (2009) Long-gap esphageal atresia treated by growth induction: the biological potential and early follow-up results. Semin Pediatr Surg 18:23–29
Bobanga ID, Barksdale EM (2015) Foker technique for the management of pure esophageal atresia: long-term outcomes at a single institution. Eur J Pediatr Surg [Epub ahead of print] PubMed PMID: 25774957
Lobe TE, Rothemberg SS, Waldshmitt J et al (1999) Thoracoscopic repair of esophageal atresia in an infant: a surgical first. Pediatr Endosurg Innov Tech 3:141–148
MacKinlay GA (2009) Esophageal atresia surgery in the 21st century. Seminars Pediatr Surg 18:20–22
Collis JL (1957) An operation for hiatus hernia with short oesophagus. Thorax 12:181–188
Al-Shanafey S, Harvey J (2008) Long gap esophageal atresia: an Australian experience. J Pediatr Surg 43:597–601
Ng J, Loukogeorgakis SP, Pierro A et al (2014) Comparison of minimally invasive and open gastric transposition in children. J Laparoendosc Adv Surg Tech 24:742–749
Thakkar HS, Cooney J, Kumar N et al (2014) Measured gap lenght and outcomes in oesophageal atresia. J Pediatr Surg 49:1343–1346
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zani, A., Cobellis, G., Wolinska, J. et al. Preservation of native esophagus in infants with pure esophageal atresia has good long-term outcomes despite significant postoperative morbidity. Pediatr Surg Int 32, 113–117 (2016). https://doi.org/10.1007/s00383-015-3821-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-015-3821-x