Abstract
Congenital heart disease (CHD) has a major impact on the survival of babies with esophageal atresia (EA). The present study assesses whether early diagnosis influences the management strategies in a large series of EA. Cases of EA treated between 1982 and 2002 were retrospectively divided into groups according to the presence or absence of CHD and to whether this was diagnosed or not prior to tracheo-esophageal fistula repair. Patients were also staged according to Spitz’s classification in which major congenital heart disease (MCHD) are those associated with cyanosis and/or heart failure requiring surgery. Comparisons between groups of patients were made by standard statistical tests. Among 195 babies with EA (99 boys and 96 girls), 82 (42%) had CHD (31 boys, 39% and 51 girls, 61%, χ2 P<0.05) and 43 out of these 82 (52%) had MCHD. Six children died without treatment. CHD was diagnosed prenatally in six cases and before EA repair in 26 cases. The diagnoses were missed in 12 instances (in five it was a MCHD). Regardless of preoperative diagnosis of right aortic arch in 3/6 cases, the oesophagus was approached from the right thorax in all cases and only in one of them the operation was not completed due to hemodynamic instability. There were 145/195 (75%) Spitz group I patients; 44/195 (22%) were group II and 6/195 (3%) group III. The mortality was respectively 9.5, 59 and 83%. We lost 15/113 (13%) babies with EA without CHD, 4/39 (10.2%) with EA and CHD and 26/43 (60%) with EA and MCHD. In children with CHD diagnosed prior to the esophageal operation 8/26 (30.7%) died and among those without diagnoses 3/12 (25%) died, (χ2 P>0.1).
-
1.
CHD was diagnosed after EA repair in one-third of cases.
-
2.
Preoperative diagnosis of CHD changed the operative indication only in one case.
-
3.
Survival after treatment for EA was not influenced by the moment or the accuracy of the diagnosis of CHD in this series.
-
4.
With only a few exceptions, associated CHD should not change the strategies of EA repair.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Among the malformations associated with esophageal atresia (EA) congenital heart disease (CHD) is only second after skeletal defects [1–3] and it is widely accepted that, together with birth weight, it largely conditions survival [4, 5].
Prognostic classification of EA proposed by Waterston in 1962 was based on birth weight, presence or absence of associated malformations and status of the lungs. This grouping system was used for years until it became obsolete because earlier diagnosis of the esophageal defect decreased the incidence of pneumonitis and improvements of neonatal care dramatically increased survival in all babies. In 1994, Spitz proposed a new prognostic classification more adapted to the current circumstances. It was based only on the influence on survival of birthweight below 1,500 g and the presence or absence of major congenital heart disease (MCHD). He divided EA patients into three groups: group I (weight above 1,500 without MCHD), group II (weight below 1,500 or MCHD) and group III (weight below 1,500 with MCHD). Mortality has been reported below 10% in group I, below 50% in group II and higher in group III [6–8].
Although accurate prenatal or early postnatal diagnosis of CHD in patients with EA should likely have an influence on the timing and strategy of EA repair or on the ensuing mortality, this issue has not been specifically investigated to this day.
The present study examines the impact of CHD diagnosis on the strategies of treatment and on the results of EA repair in a large group of patients.
Materials and methods
We studied the charts of patients treated for EA at our institution during the period 1982 to 2002 retrospectively, with particular attention paid to cardiologic diagnoses and mortality. We separately studied patients in whom prenatal ultrasonography had been carried out and those in whom CHD had been prenatally diagnosed by these means. We also separated patients in whom postnatal cardiologic assessment had been done prior to EA repair and those in whom this step was not taken. Among the patients with diagnosed CHD, we distinguished those with MCHD (those in which cyanosis and/or heart failure requiring surgical treatment were present) and those with non-threatening CHD. We also classified our patients according to the Spitz grouping system. CHD were classified into heart and great vessel malformations for descriptive purposes (Table 1). Obviously, both types of defects were often present in the same patient. Right aortic arch (RAA) and isolated dextrocardia were particularly considered because of their potential for interference with the standard surgical approach for EA repair. MCHD were separated from the non-threatening ones (Table 2).
The possible modifications of the strategy of surgical repair of EA in the different groups and for the specific cardiac defects were individually examined. Mortalities in all groups were compared by Chi square tests (χ2) with Yates’ correction when appropriate and a threshold of significance of P<0.05.
Results
One hundred and ninety-five children (99 boys, 50.5% and 96 girls, 49.5%) were included in the study; Out of these 195, 82 (42%) suffered CHD and, interestingly a significant majority (51 or 61%) were girls (χ2, P<0.05 vs 31 boys or 39%). One hundred and sixty-four (84%) had EA with distal tracheo-esophageal fistula (TEF), 19 (9.7%) had isolated EA, 8 (4.1%) had an H-type TEF, 2 (1%) had EA with proximal and distal TEF and 2 (1%) had EA with proximal TEF; incidence of CHD in each type of atresia was 71/164 (43%), 6/19 (31%), 3/8 (37%), 1/2 (50%), respectively, and there was no CHD in the last group. Differences in CHD incidence between isolated EA, H-type TEF and EA with distal TEF were not statistically significant (P>0.1).
Among the 82 children with CHD, 43 (52%) suffered MCHD (Table 2) and the remaining 39 had non-threatening CHD. In five babies diagnosed at birth with EA and CHD, esophageal repair was not attempted because they had multiple or very severe associated conditions (four trisomies and one Di George Syndrome) and died. Four out of these five children had MCHD and were excluded from the study because the possible influence of the cardiologic diagnosis on the treatment of EA could not be assessed in them. In consequence, only 78 children with CHD were considered for this purpose.
Only 32/78 pregnancies of children with CHD were ultrasonographically controlled and six of them (18.7%) had prenatal diagnosis of heart malformation that was confirmed after birth in all cases (3 VSD, 1 Fallot, 1 transposition of the great vessels and 1 coarctation of the aorta).
Thirty-eight of 78 babies (48.7%) including the 6 prenatally diagnosed had complete cardiologic assessment before EA repair and the CHD was appropriately identified in 26 (68%) while the diagnoses was incomplete in 12 (32%). Five of these 12 (41%) suffered MCHD (2 VSD, 1 Fallot, 1 complete atrioventricular canal and 1 truncus arteriosus). The pattern of CHD diagnosis changed over time. Between 1982 and 1992, 30/104 (28%) babies with EA had a diagnosis of CHD whereas 48/94 (51%) had such diagnoses between 1993 and 2002 (χ2 P<0.05).
Six children (3%) had an RAA and three of them were diagnosed prior to EA repair in three. In spite of this, right thoracotomy approach was preferred for EA with distal TEF repair except in one patient in whom hemodynamic instability due to MCHD precluded thoracotomy. This baby had only gastrostomy and died in the first week of life.
Overall, 15/113 babies with EA without CHD (13%), 4/39 with EA and CHD (10%) and 26/43 with EA and MCHD (60%) died. In this respect, differences in mortality in the groups without CHD and with threatening CHD were not statistically significant (P>0.1) whereas they were significant (P<0.05) between the group with MCHD and the other two groups.
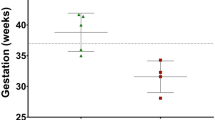
Overall survival was 150/195 (77%) and when the patients were classified according to Spitz groups, mortality was 14/145 (9.5%) for group I, 26/44 (59%) for group II and 5/6 (83%) for group III (Table 3).
Apparently, an accurate diagnosis of the CHD before EA repair had no significant influence in the results because among patients with an accurate diagnosis, mortality was 30.7% (8/26) and among those without preoperative diagnosis, it was 25% (3/12) (ns).
Discussion
Our series of EA is comparable to most other published in the literature in terms of incidence of CHD that has been reported to range between 13.2 and 41% [2, 9–17]. Our 42% is slightly higher perhaps because we included some malformations of the great vessels, like RAA or aberrant subclavian arteries (ARSA) due to their potential impact on the choice of the surgical approach for EA repair [9, 10]. The previously unreported higher incidence of CHD in girls with EA in comparison with boys came as a surprise. High proximal pouch in EA has been reported to be associated with aortic-arch, skeletal and azygos vein anomalies [11–13]. However, in our series, the incidence of CHD was similar in all EA types. The MCHD diagnosed in our series (Table 2) had a distribution similar to that in other series [15–20]. Our prevalence of MCHD (52%) was similar to that published by Spitz [4] and the distribution of the clinical material among the three groups and the mortality in each one was comparable as well (Table 3). The analysis of the nature of CHD in this series reveals a pattern consistent with the involvement of neural crest cell dysregulation in the pathogenesis [21, 22].
The relatively low rate of prenatal diagnosis of CHD is in part explained by the long period of time covered by the present study. Most diagnoses are concentrated in the most recent years. The relatively low rate on postnatal, preoperative diagnosis of some of the cardiovascular defects can be explained by the poor clinical expression of some of the defects with increased pulmonary flow during the first 3 or 4 days of life due to the high pressures in the lung vascular bed.
The increased diagnosis of CHD in the last years has also been noticed by other authors [7, 23] and it may reflect the increased use of ultrasonography as a routine diagnostic tool in the NICU as well as an increasing severity of the associated defects.
Six children (3%) had RAA, a proportion similar to that reported in other series (1.8–5%) [24–26]. Although it has been claimed that the finding of tracheal displacement at a certain level in plain X-ray of the thorax suffices the diagnosis of RAA [26, 27] other investigators disagree [28] and our experience goes in the same direction because no baby in our series was diagnosed on this basis. MRI [28–30] or aortography [28, 31] can accurately delineate the position of the aortic arch but they are not available everywhere around the clock and it is not realistic to pretend that that their routine use in newborns with EA is required. On the contrary, ultrasonography is the best non-invasive method of diagnosis of RAA [14] as attested by the high rate of preoperative diagnosis in our series (50%) in comparison with other series (8–15%) [24–26]. Nevertheless, since like other authors [24, 25] we used a right approach in all operated cases without any major technical problem related to the RAA, we do not believe that this diagnosis is determinant prior to EA repair. The same can be applied to our two cases of dextrocardia or ARSA.
As previously stated, only one 1,500 g baby had the treatment of the esophageal malformation delayed because of the presence of MCHD. His obvious hemodynamic instability precluded primary anastomosis and he died 10 days after gastrostomy under vigorous ventilatory and hemodynamic support. All other patients were managed by primary anastomosis and fistula ligation or feeding gastrostomy with continuous suctioning of the upper pouch depending on the malformation irrespective of the presence or not of CHD; the fact that mortality in 68% of patients with associated CHD diagnosed preoperatively was not different from that in those in whom the diagnosis was missed or wrong illustrates the relative importance of this diagnosis for repair and survival.
In summary, based on our experience we do believe that there is room for improving prenatal diagnosis of CHD. All patients with EA should be investigated ecographically prior to EA repair. With only a few exceptions, the diagnosis of CHD does not change the timing and the modalities of EA repair. Finally, the presence of an RAA, ARSA or dextrocardia does not change the chances of a successful esophageal anastomosis by the usual approach.
References
Chittmittrapap S, Spitz L, Kiely EM, Brereton RJ (1989) Oesophageal atresia and associated anomalies. Arch Dis Child 64:364–368
Myers NA, Beasley SW, Auldist AW (1992) Oesophageal atresia and associated anomalies: a plea of uniform documentation. Pediatr Surg Int 7:97–100
Okada A, Usui N (1992) Esophageal atresia in Osaka: a review of 39 years of experience. J Pediatr Surg 32:1570–1574
Spitz L, Kiely EM, Morecroft JA (1994) Oesophageal atresia: at risk groups for the 1990. J Pediatr Surg 29:723–725
Waterston DJ, Bonham Carter RE, Aberdeen E (1962) Oesophageal atresia: tracheoesophageal fistula. A study of survival of 218 infants. Lancet 1:819–822
Mellins RB, Blumenthal S, Sheppard M (1964) Cardiovascular anomalies and esophageal atresia. Am J Child Dis 107:96–100
Ein SH, Shandling B, Newcastle R (1994) Pure esophageal atresia: a 50 years review. J Pediatr Surg 29:1208–1211
Holder TM, Ashcraft KW, Sharp RJ, Amoury RA (1987) Care of infants with oesophageal atresia, tracheoesophageal fistula and associated anomalies. J Thorac Cardiovasc Surg 94:828–835
Tulloh RMR, Tansey SP, Parashar K (1994) Echocardiographic screening in neonates undergoing surgery for gastrointestinal malformations. Arch Dis Child Fetal Neonatal 70:206–208
Abu-Harb M, Hey E, Wren C (1993) Death in infancy from unrecognised heart disease. Arch Dis Child 71:3–7
Touloukian RJ, Keller MS (1988) High proximal pouch esophageal atresia with vertebra, rib and sternal anomalies: an additional component to the VATER association. J Pediatr Surg 23:76–79
Gupta DK, Arora M, Srinivas M (2001) Azygos vein anomaly: the best predictor of a long gap in esophageal atresia and tracheoesophageal fistula. Pediatr Surg Int 17:101–103
Kulkarni B, Rao RS, Oak S, Upadhyaya MA (1998) 13 pairs of ribs-a predictor of long gap atresia in tracheoesophageal fistula. J Pediatr Surg 33:1328
Hoffman JL (1995) Incidence of congenital heart disease. Pediatr Cardiol 106:103–113
Bull C, Ashcraft KW, Sharp RJ (1999) Current and potential impact of fetal diagnosis prevalence and spectrum of serious congenital heart disease at term in the UK. Lancet 354:1242–1247
Choudhury R, Ashcraft K, Sharp R, Murphy J, Snyder CH, Sigalet D (1999) Survival of patients with esophageal atresia: influence of birth, weight, cardiac anomaly and late respiratory complications. J Pediatr Surg 34:70–74
Greenwood A, Rosenthal A (1974) Cardiovascular malformations associated with tracheoesophageal fistula and esophageal atresia. Pediatrics 1:87–91
Louhimo I (1999) Esophageal atresia: primary results of 500 consecutively treated patients. J Pediatr Surg 18:823–828
Bishop PJ, Klein MD, Philippart Al, Hixson DS (1983) Transpleural repair of esophageal atresia without primary gastrostomy: 240 patients treated between 1951 and 1983. J Pediatr Surg 20:823–828
Ferenz C (1990) On the birth prevalence of congenital heart disease. J Am Coll Cardiol 21:1701–1702
Otten C, Migliazza L, Xia H, Rodriguez J, Diez-Pardo JA, Tovar JA (2000) Neural crest-derived defects in experimental esophageal atresia. Pediatr Res 47:178–183
Morini F, Ilari M, Casati F (2001) Pattern of cardiovascular anomalies associated with esophageal atresia: support for a caudal pharyngeal arch neurocristopathy. Pediatr Res 50:565–568
Driver CP, Shankar KR, Jones MO, Lamont GA, Turnok RR, LLoyd DA, Losty PD (2001) Phenotypic presentation and outcome of esophageal atresia in the era of Spitz classification. J Pediatr Surg 36:1419–1422
Stringel G, Coln D, Guerrin L (1990) Esophageal atresia and right aortic arch: right or left thoracotomy. Pediatr Surg Int 5:103–105
Bowett B, Beasley SW, Myers NA (1999) The frequency, significance and management of right aortic arch in association with esophageal atresia. Pediatr Surg Int 15:28–31
Burrows P, Mc Donald C, Morecroft JA (1999) Magnetic resonance imaging of the pediatric thoracic aorta. Semin Ultrasound 14:129–144
Berdon WE, Baker DH, Neilson IR (1974) Plain film detection of a right aortic arch in infants with esophageal atresia and tracheoesophageal fistula. J Pediatr Surg 14:436–437
Van Son J (1993) Demonstration of vascular ring anatomy with CT. Thorac Cardiovasc Surg 36:277–279
Harrison R, Weithman J, Waterston DJ (1980) Localization of the aortic arch prior to repair of esophageal atresia. J Pediatr Surg 15:312
van Son J (1994) Imaging strategies for vascular rings. Ann Thorac Surg 57:604–607
Hands LJ, Dudley NE (1986) A comparison between gap length and Waterston classification as guides to mortality and morbidity after surgery for esophageal atresia. J Pediatr Surg 21:404–406
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Encinas, J.L., Luis, A.L., Avila, L.F. et al. Impact of preoperative diagnosis of congenital heart disease on the treatment of esophageal atresia. Ped Surgery Int 22, 150–153 (2006). https://doi.org/10.1007/s00383-005-1595-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-005-1595-2