Abstract
Meckel’s diverticulum is the most common congenital gastrointestinal anomaly. 99m Technetium pertechnetate imaging (Meckel’s scan) is the best noninvasive method used to diagnose this condition when heterotopic gastric mucosa (HGM) is present. Although cimetidine enhancement has been shown to improve sensitivity of the Meckel’s scan, ranitidine enhancement has also been advocated; however, this recommendation is based on unpublished data. Thirty-seven children with confirmed Meckel’s diverticulum were reviewed retrospectively. Of eight children with HGM in the Meckel’s diverticulum who presented with profuse rectal bleeding and underwent the conventional Meckel’s scan, three of them (37.5%) had a false negative study. Ranitidine, when administered either intravenously or orally for 24 h prior to the Meckel’s scan, enhanced the sensitivity of this test to 87.5% in our patient cohort.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meckel’s diverticulum, a remnant of the omphalomesenteric duct, is the most common congenital gastrointestinal anomaly, with an estimated prevalence of 1–4% in the general population [1, 2]. The clinical presentation is variable and nonspecific, which can make diagnosis difficult. 99m Technetium pertechnetate imaging is the most useful method of detecting a Meckel’s diverticulum [2, 3] because the isotope is taken up and secreted by heterotopic gastric mucosa (HGM), the most common ectopic tissue in the diverticulum. However, the reported sensitivity of the test ranges from 50–92% [4]. Pharmacological intervention using histamine type-2 (H2) receptor antagonists has been reported to increase the sensitivity [5]. Ranitidine, which is associated with fewer adverse reactions than cimetidine, has been recommended as a possible pharmacological intervention [5]; however, supporting data are unpublished. We report our 5-year experience of Meckel’s diverticulum and the usefulness of ranitidine for improving Meckel’s scan sensitivity after failure of the conventional test.
Materials and methods
Case records of all children who had a confirmed diagnosis of Meckel’s diverticulum at the Royal Children’s Hospital for a 5-year period from December 1997 until December 2002 were reviewed retrospectively. Demographic data (including age at presentation and gender of patient), major presenting symptoms (gastrointestinal bleeding, bowel obstruction, inflammation, or others), results of 99m technetium pertechnetate Meckel’s scan, and histologic findings were recorded.
Statistical analysis was performed with Fisher’s exact test and the Mann-Whitney test; a p value <0.05 was considered significant.
Results
Thirty-seven children (70% male; mean age 6 years, range 0.1–17.7 years) with histopathologically confirmed Meckel’s diverticulum were included in the study. Major presenting symptoms of all patients are summarised in Table 1. The median age of patients presenting with per rectal bleeding was 4 years (interquartile range 1.4–14.8 years) compared with 3.6 years (interquartile range 0.2–10.8 years) of patients presenting with other symptoms. There were no significant differences in gender split between these two groups (67% male and 71% male, respectively).
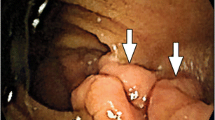
Nine children presenting with per rectal bleeding underwent 99m technetium pertechnetate imaging without prior barium studies. Eight out of nine did not receive H2-receptor antagonists prior to the Meckel’s scan. Five children (56%) had successful demonstration of a diverticulum, and four children (including one who received ranitidine) had a false negative scan. Of those with a negative Meckel’s scan, two children underwent the ranitidine-enhanced Meckel’s scan, in which either ranitidine 1 mg/kg intravenously every 8 h or 150 mg orally every 12 h for 24 h was used before the Meckel’s scan. Both of these children had HGM identified by this technique. One child who, due to severe abdominal pain, received four doses of ranitidine 0.5 mg/kg intravenously prior to the first study underwent a second conventional Meckel’s scan but still had a negative study. The patient underwent laparotomy a day later, and an inflamed Meckel’s diverticulum was resected. Another child underwent laparotomy because of ongoing gastrointestinal bleeding with a superimposed picture of clinical bowel obstruction. At operation, a Meckel’s diverticulum as the pathological lead-point of the intussusception was revealed. All except this last patient had HGM within the diverticulum (Table 1). Data of HGM size were unavailable. HGM was more commonly found in patients presenting with gastrointestinal bleeding than in patients presenting with other symptoms (87.5% and 46%, respectively; p =0.05).
The sensitivity of the conventional Meckel’s scan for diagnosis of HGM was 62.5% (five of eight patients). Combined with ranitidine enhancement, the sensitivity of the Meckel’s scan to detect HGM was increased to 87.5% (seven of eight patients).
Discussion
Although a Meckel’s diverticulum is the most common congenital gastrointestinal anomaly, it is usually asymptomatic [1, 3]. Symptomatic Meckel’s diverticulum is seen more frequently in males, as shown by a 70% incidence in the present study and 69–74% incidence in previous studies [6, 7]. Painless rectal bleeding, small bowel obstruction (intussusception or volvulus), and inflammation-related complications are the leading presenting symptoms reported in children: 31–34%, 24–31%, and 16–21%, respectively [6, 7], which is comparable with our study. The clinical presentation has been associated with the likelihood of the Meckel’s diverticulum containing HGM. While HGM is found in 50–62% of all symptomatic patients, this prevalence is increased to up to 95–100% in patients with bleeding [2, 8, 9]. In the present study, the percentages of HGM in all symptomatic patients (56%) and in patients with rectal bleeding (88%) are comparable with previous reports [2, 7, 9].
Confirmation of the diagnosis of Meckel’s diverticulum can be very difficult. Standard abdominal radiography, barium study, and computed tomography rarely make a preoperative diagnosis [1, 3, 10]. 99m Technetium pertechnetate, which is taken up and secreted by the mucous-secreting cells of the gastric mucosa, was first applied for detection of Meckel’s diverticulum in 1970 [11], with a high specificity of 95–100%. However, the sensitivity of the test has remained a problem. A cumulative sensitivity of 85% from multicentre studies has been reported [8], but this may vary from 50–92% [4]. The 62.5% sensitivity of the conventional Meckel’s scan in the present study is comparable with other reports in indicating the presence of a Meckel’s diverticulum containing HGM [4, 8]. A false negative scan result has been attributed to the small size of the island of HGM, recent barium study, or the lesion’s being obscured by the urinary bladder [2]. In the present study, none of the patients underwent a barium meal prior to a scan, and we did not have data concerning the size of HGM in each patient.
H2-receptor antagonist administration prior to Meckel’s scan has been advocated as a pharmacological enhancement of the test’s sensitivity [2, 5, 10]. It is postulated that the release of pertechnetate from mucous cells and/or parietal cells into the diverticular lumen [2, 5] is delayed; however, the exact mechanism that enhances visualisation remains unclear. Ranitidine, one of the H2-receptor antagonists, has been used extensively with proven safety [12]. Compared with cimetidine, it was reported to have less frequent and/or less severe adverse reactions and drug interactions. Recently, there was a recommendation to use ranitidine as a pharmacological enhancement for Meckel’s scan; however, this recommendation was based on unpublished data [5]. Heyman [12] also reported improved efficacy of Meckel’s scan by using ranitidine combined with pentagastrin after a false negative test with pentagastrin only. Up to the present time, there are limited data on ranitidine for improving test sensitivity.
We report here our experience of Meckel’s scan and the usefulness of the H2 antagonist ranitidine for improving the test’s sensitivity in children with suspected false-negative results. Two children who received an appropriate dose of ranitidine prior to the Meckel’s scan were successfully diagnosed after failure of the conventional method. Either intravenous administration of 1 mg/kg every 8 h or oral administration of 150 mg twice daily for 24 h before Meckel’s scan has been shown to be effective. Failure to identify a Meckel’s diverticulum (with HGM) in one patient may have been caused by the child’s receiving an inadequate dose of ranitidine (0.5 mg/kg/dose) [5]. In our experience, conventional Meckel’s scan combined with ranitidine enhancement can detect 87.5% of HGM-containing Meckel’s diverticula. Although it could be argued that our findings are consistent with performing sequential scans, it is difficult to attribute the perceived increase in the test’s sensitivity to anything but pretreatment with an H2 antagonist, as barium studies were not performed in any of the patients with HGM and the size of the HGM was constant between tests. The technique used to perform each study did not vary, and interpretation was provided by the same physicians. Because data of the HGM size were unavailable, we cannot comment on the role of the amount of HGM.
In summary, our findings would support the use of priming with an H2 antagonist before performing a 99m technetium pertechnetate scan, so as to increase the sensitivity of this diagnostic test that is both expensive and involves exposing the patient to radiation. However, our data do need to be cautiously interpreted within the limitations of a retrospective study. A large multicentre trial is required to definitively assess the effect of pretreatment with an H2 antagonist on the sensitivity of a Meckel’s scan.
Because there is significant prevalence of a false-negative Meckel’s scan, and because of the frequent use and acceptance of ranitidine as a safe medication, we suggest that ranitidine-enhanced 99m technetium pertechnetate imaging should be performed for the diagnosis of Meckel’s diverticulum, especially if suspected in a patient after a failed conventional scan. Ranitidine, either 1 mg/kg intravenously every 8 h or 150 mg orally every 12 h for 24 h prior to Meckel’s scan, is recommended.
References
Schwartz MZ (1999) Meckel’s diverticulum and other omphalomesenteric duct remnants. In: Wyllie R, Hyams JS (eds) Pediatric gastrointestinal disease, 2nd edn. Saunders, Philadelphia, pp 483–488
Emamian SA, Rana ES, Majd M (2001) The spectrum of heterotopic gastric mucosa in children detected by Tc-99m pertechnetate scintigraphy. Clin Nucl Med 26:529–535
Martin JP, Connor PD, Charles K (2000) Meckel’s diverticulum. Am Fam Physician 61:1037–1042
Fries M, Mortensson W, Robertson B (1984) Technetium pertechnetate scintigraphy to detect ectopic gastric mucosa in Meckel’s diverticulum. Acta Radiol Diagn (Stockh) 25:417–422
Datz F, Christian PE, Hutson WR, Moore JG, Morton KA (1991) Physiological and pharmacological interventions in radionuclide imaging of the tubular gastrointestinal tract. Semin Nucl Med 21:140–152
Mackey WC, Dineen P (1983) A fifty year experience with Meckel’s diverticulum. Surg Gynecol Obstet 156:56–64
Cooney DR, Duszynski DO, Camboa E, Karp KP, Jewtt TC (1982) The abdominal technetium scan (a decade of experience). J Pediatr Surg 17:611–619
Sfakianakis GN, Conway JJ (1981) Detection of ectopic gastric mucosa in Meckel’s diverticulum and in other aberrations by scintigraphy: I. Pathophysiology and 10-year clinical experience. J Nucl Med 22:647–654
Yamaguchi M, Takeuchi S, Awazu S (1978) Meckel’s diverticulum: investigation of 600 patients in Japanese literature. Am J Surg 136:247–249
Rossi P, Gourtsoyiannis N, Bezzi M, et al. (1996) Meckel’s diverticulum: imaging diagnosis. AJR Am J Roentgenol 166:567–573
Jewett TC Jr, Duszynski DO, Allen JE (1970) The visualization of Meckel’s diverticulum with 99mTc-pertechnetate. Surgery 68:567–570
Heyman S (1994) Meckel’s diverticulum: possible detection by combining pentagastrin with histamine H2 receptor blocker. J Nucl Med 35:1656–1658
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rerksuppaphol, S., Hutson, J.M. & Oliver, M.R. Ranitidine-enhanced 99m technetium pertechnetate imaging in children improves the sensitivity of identifying heterotopic gastric mucosa in Meckel’s diverticulum. Ped Surgery Int 20, 323–325 (2004). https://doi.org/10.1007/s00383-004-1189-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-004-1189-4