Abstract
Introduction
Chronic subdural hematoma (cSDH) is a disease of the elderly population. Incidence in paediatric population is relatively uncommon. Child abuse, birth trauma, coagulopathy and shunt surgeries represent major causes. Major impact of the disease on life of patient due to recurrence and repeat surgical procedure is significant, not to mention the burden on health care system.
Material and methods
We retrospectively reviewed our institute data for chronic sub-dural cases for the past 10 years (2008–2018) and collected data on the demography, clinical features, metabolic workup, mode of treatment, recurrence rates, predisposing factors, laterality, hematoma characteristics and factors associated with recurrence in all cases with less than or equal to 18 years of age.
Results
A total of 30 such cases were found in a period of 10 years (2008–2018). The mean patient age was 7.3 years (range 2 months–17 years), with 20 males (66.67%) and 10 females (33.33%). Raised intracranial pressure (n = 9) was the commonest presenting symptom in 30% of cases followed by seizures in 26.67% (n = 8). The previous shunt was the commonest predisposing factor seen in 43.33% (n = 13). cSDHs were unilateral in 56.67% cases (n = 17) and bilateral in 43.33% (n = 13). Burr hole craniostomy was done in 27 cases (90%), and conservative management was done in three cases (10%). Follow up was available for 27 cases (90%) with a mean follow up duration of 24 months. Recurrence rate was 30% (n = 9). Shunt surgery contributed to 77% of bilateral disease (p = 0.009). Child abuse was not reported in our series.
Conclusion
Presence of paediatric cSDH is alarming, and the physician should be alerted to look for underlying cause and rule out child abuse. Detailed metabolic, skeletal workup is required. Treatment of primary pathology should be the goal as CSF diversion is not the solution to all problems, but can definitely be the cause of all the problems.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chronic subdural hematoma (cSDH) is a common disease of the geriatric population. In the paediatric age group, the incidence of this condition is relatively uncommon, and literature is sparse on this topic. The English literature search revealed only four major case series in the recent past [1,2,3,4]. The common underlying factor of diffuse brain atrophy or anticoagulant, which is predominant in elderly cSDH, is rare in paediatric population. Child abuse, birth trauma, coagulopathy and shunt surgeries are the major predisposing factors in this age group. Long bone and fundus examination along with skin bruises at various stages of healing are invaluable findings pointing to the underlying child abuse.
There are no specific presenting symptoms. The usual presenting symptoms are headache, vomiting, seizure, focal neurological deficit or altered sensorium. In infants, it can present in the form of refusal to feed, increased head circumference and delayed or regression of milestones [4]. Imaging forms the cornerstone for the diagnosis and guides the treatment strategy along with the clinical findings.
Various treatment options have been suggested for the management of paediatric cSDH ranging from expectant management, subdural-peritoneal shunt (SPS), subdural-subgaleal shunt, twist drill tapping and burr hole evacuation with or without subdural drain to craniotomy with membrane excision. In neonates/infants, fontanelle tapping remains an important procedure for drainage of sub-dural haematomas. Recently, the role of dexamethasone and atorvastatin has been suggested in the management of recurrent paediatric cSDH [5]. Here, we report our experience of 30 cases of paediatric cSDH managed at our institute over a period of 10 years. The detailed demographic, clinical, imaging, histopathological features and outcome have been studied. We also tried to analyse the factors predicting the recurrence of the disease.
Materials and methods
This is a retrospective study performed in a single tertiary care referral institute. All the cases of paediatric cSDH with age less than 18 years who were managed surgically or medically at our institute between the years 2008 and 2018 were included. The recurrent cases of cSDH were excluded from the current study. Data was obtained from the hospital’s medical record section. The relevant demographic, clinical details, imaging features, surgical details and outcome were studied using chi-square analysis. Computed tomography (CT) or magnetic resonance imaging (MRI) of the brain was done in all the patients. All the attempts were made to find out the underlying predisposing factors especially child abuse. Chest X-ray and spine and extremity X-rays were done along with fundus examination in the suspicious cases of child abuse. Metabolic work up was done when genetic diseases like mucopolysaccharidosis were considered in the differential diagnosis. Routine blood investigations like haemogram, ESR, renal and liver function tests and coagulation profile were done in all the patients.
Decision for surgery was taken based on the clinical presentation and/or radiological progression of the disease. Standard surgical procedure of burr holes with evacuation of chronic SDH was performed under general anaesthesia. The number of burr holes made was decided based on the imaging findings. Wherever membrane was seen during the surgery, biopsy was taken from the membrane and sent for histopathological examination. Decision to keep the subdural drain was left to the surgeon’s discretion or lack of brain surfacing at the end of surgery. Drain was removed in 48 h after obtaining a plain CT head. Clinical follow up was obtained at the interval of 3 months to look for recurrence in which re-surgery was performed. Follow up was obtained from the case sheet or, in some cases, telephonic conversation to know their current status.
Results
Clinical presentation
A total of 30 cases of paediatric cSDH were included in the study. The mean patient age was 7.3 years (range 2 months–17 years). The study consisted of 20 males (66.67%) and 10 females (33.33%). Raised intracranial pressure (n = 9) was the commonest presenting symptom in 30% of cases followed by seizures in 26.67% (n = 8) and headache and altered sensorium in 13.33% each (n = 4). Here, raised ICP was defined as any symptom suggestive of increased intracranial pressure such as vomiting, increased head circumference, papilledema or up-gaze restriction. Hemiparesis was seen in two cases: increase in head circumference, regression of milestones and behaviour disturbance in one child each (Tables 1 and 2).
Predisposing factors
Twenty-five cases (83.33%) had underlying predisposing factors. Previous shunt was the commonest predisposing factor seen in 43.33% (n = 13). History of trauma was found in 23.33% (n = 7) including one birth trauma induced by forceps delivery, followed by one case of coagulopathy, infective (HIV with TB), brain atrophy (mucopolysaccharidosis) (Fig. 1), antiplatelet therapy and post occipital encephalocele surgery each (Table 3).
Our centre usually does not operate on neonates; hence, the usual indications for shunts such as preterm delivery or intraventricular haemorrhage was not contributory. In 11 out of the 13 cases (84.6%), the shunts (Fig. 2) were inserted as a result of obstructive hydrocephalus, i.e. due to tumours either posterior fossa, brain stem or thalamic lesions. All of these shunts were fixed medium pressure ventriculoperitoneal shunts. Interestingly, the period between shunt insertion and presentation as a chronic sub-dural was less than 3 months in all cases and ranged from 1 to 3 months, further lending credence to our hypothesis of shunts leading to hematoma formation. In two cases of congenital hydrocephalus where a medium pressure shunt was inserted, the latency period between the index shunt and presentation of the chronic sub-dural was 28 months and 20 months respectively, with the former having undergone 2 shunt revisions. In both cases, the shunt was ligated and sub-dural evacuated with no symptoms of hydrocephalus at follow-ups.
Imaging features
CT brain was done in 25 cases (83.33%) and MRI in five cases (16.67%). Abnormal skeletal X-rays were seen in three cases with history of trauma. One case had the acute component on CT brain with history of recent trauma. cSDHs were unilateral in 56.67% cases (n = 17) and 43.33% in bilateral (n = 13) (Table 4).
Treatment
Few patients (n = 3) were managed medically, as the symptoms were not severe, and there was no deficit on examination. For those children who underwent surgery, burr hole and evacuation of cSDH were done: 27 cases (90%). Conservative management was done in three cases (10%) with minimal symptoms and no midline shift/mass effect on imaging. Subdural drain was kept in three of the operated cases (Table 5). In five cases, membrane was seen during surgery, and biopsy was performed. All the materials were sent for histopathological examination. None of the biopsy samples revealed evidence of infection or malignancy. All those cases presented with chronic subdural in conjunction with a shunt; the shunt was ligated and primary pathology, i.e., tumour, was dealt with directly.
One case which highlights the need for direct management of the tumour was that of a 9-year-old boy who presented to the emergency department with a headache and vomiting for 3 days. On doing a computed tomography (CT) scan, there was a posterior fossa lesion with hydrocephalus. Since the primary was not dealt with directly, the child was shunted. Subsequently, the child returned a month later with similar complaints of drowsiness and poor feeding and the post-ventriculoperitoneal shunt showing collapsed ventricles with chronic subdural haematoma (Fig. 3). The posterior fossa lesion was removed and the shunt ligated in the same procedure. Postoperatively, the plain CT scan showed decompression of the posterior fossa lesion with a ligated shunt in situ; however, the chronic sub-dural remained, and the child did not improve in sensorium. Burr hole and evacuation of the chronic SDH did not result in improvement in sensorium (Fig. 3e, f). A diffusion-weighted imaging and apparent diffusion coefficient MRI images showed multiple venous infarcts secondary to compression by chronic hematoma causing ischemic encephalopathy. The histopathology was that of pilocytic astrocytoma. This case highlights the need for direct management of the lesion or reduction in the time interval between shunting and tumour surgery.
a Axial cut of a plain CT scan showing a posterior fossa lesion with supratentorial hydrocephalus; b post-ventriculoperitoneal shunt showing collapsed ventricles with chronic subdural hematoma; c axial cut of a plain CT scan showing decompression of the posterior fossa lesion with a ligated shunt in situ; d post-burr hole and evacuation of chronic SDH with a shunt in situ; e, f axial cuts of diffusion-weighted imaging and apparent diffusion coefficient MRI images showing multiple venous infarcts secondary to compression by chronic hematoma causing ischemic encephalopathy
Follow up and outcome
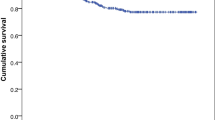
There was no new post-operative morbidity or mortality in any of the patients. Hemiparesis improved in both the cases, and post-operative period was seizure free for all those presenting with seizures. Follow up was available for 27 cases (90%) with mean follow up duration of 24 months (range: 3 months–10 years) with a median follow up of 15 months. Recurrence was seen in 30% of the available follow up (n = 9). All the recurrent cases underwent second surgery. Re-exploration of the burr hole and evacuation were done in six cases, SPS in two cases, and one case required craniotomy and evacuation of SDH.
Recurrence and factors
All the demographic details and other imaging/surgical parameters were analysed to look for the factors predicting the recurrence. Gender, history of trauma, use of subdural drain, laterality and acute component in SDH did not have any significant correlation predicting the recurrence. The trend of recurrence was more in bilateral disease (55.6% vs 44.4%, p = 0.075) and those who had undergone shunt in the past (55.6% vs 44.4%, p = 0.57); however, the results were not statistically significant, which may be due to the small sample size.
As noted above, a total of 13 patients had a history of undergoing shunt procedure before presentation; the majority (n = 10), approximately 77%, had bilateral disease (p = 0.00943), which is statistically significant, and out of 9 recurrent cases, 5 patients had a history of undergoing shunt, and out of these 5 cases, 4 cases had hematoma as collection, and 1 patient had hygroma which was managed with SPS.
Discussion
Pathophysiology
Among the paediatric age group, cSDH is more prone to occur under the age of 2 years because of physiological craniocerebral disproportion [8, 18] which can cause traversing veins to tear and form a subdural collection. Arachnoid villi consist of its capsule, fibroblasts and endothelium. These arachnoid villi connect the column of arachnoid cells to venous sinuses. The shear strain at this attachment, which is produced by acceleration/deceleration of the brain, results in disruption of arachnoid column. So, CSF from exposed subarachnoid space communicates freely with the subdural space leading to subdural collection [19].
Predisposing factors
In our study, as noted above, the most common predisposing factor is history of shunt for various pathologies, and it is shown that the presence of shunt predisposes the child to bilateral disease which is responsible for macrocrania, but will cause delay in cerebral development; the presence of shunt has caused maximum number of recurrences in our study, but it was statistically insignificant which may be attributed to the small sample size, which begs the question, should shunt be done when primary pathology can be handled without it?
It is pertinent to mention the 5 cases which had no predisposing factors. One possible explanation could be an unnoticed trauma which was not reported. Many infants with TBI have no clinical symptoms of brain injury [20,21,22,23,24,25,26,27,28,29], and even if these are present, the child may essentially be asymptomatic. It is only after weeks have passed and the hematoma has converted into a chronic sub-dural do these children present with headache, seizures or altered sensorium. Another explanation can be rupture of an unnoticed arachnoid cyst which has presented directly as a chronic sub-dural hematoma [30]. Minor head trauma often precedes complications causing rupture of small bridging vessels between the dura and outer membrane of an arachnoid cyst. Burr hole and evacuation done initially may relieve the child of the symptoms while the arachnoid cyst may go unnoticed [30].
Clinical feature
Wang et al. have reported a case of cSDH in a 9-year-old child with history of dodge ball injury [20]. The above study has suggested that diagnosis of cSDH should be suspected for any patient with or without a history of trauma presenting with the following: (1) any change in the neurological state, (2) focal neurological deficit and (3) progressive severe headache. In the series from the most recent decade [14, 17, 25,26,27], some cases had minimal headaches or were asymptomatic shunted hydrocephalic patients scanned during routine follow-up. Our series has reconfirmed the male preponderance similar to other study [3]. Most cases presented with symptoms of seizures, bulging fontanelles, anorexia, and lethargy. At least 40% of cases from the study by Parent [3] were related to child abuse, which is in contrast to many authors [21, 22]. Birth trauma, on the other hand, accounted for only a few cases in other series. We had one such case of birth trauma related to forceps delivery.
Imaging
MRI is superior to CT scanning for differentiating subdural from subarachnoid collections. Zourous et al. have explained the theory of dynamic CSF hemato-hygroma of traumatic origin based on the MRI findings [1]. Suh et al. demonstrated that diffusion-weighted MRI was more sensitive in detecting white matter injury as compared to standard MRI and also for predicting the outcome [23]. In our series, MRI was done in only 5 cases, mainly in those with suspicion of metabolic cause or non-traumatic origin. CT was predominant modality of imaging done in 25 cases. CT provides useful information for calvarial fracture in case of traumatic brain injury especially in cases of child abuse. Ultrasound through the anterior fontanelle has important role in infant when undergoing evaluation of macrocephaly. It can reveal the amount of fluid in the subdural fluid and also the septations within it. Its utility might increase in the future because of ease of availability, can be done bedside, better logistic aspects and also lack of sedation as compared to MRI [4]. The role of ultrasound in normal-sized infants for the detection of subdural hematomas is limited by its lateral location which hampers its correct visualization. Indeed, ultrasound has a limited value for both initial diagnosis and postoperative assessments.
Treatment
The various treatment options described in the literature are percutaneous tapping, burr hole drainage with or without subdural drain, craniotomy and evacuation, SPS or subdural-subgaleal shunt. SPS has been supposed by many to have the least recurrence for the paediatric cSDH; however, it often requires second look surgery to remove the shunt at a later date [8, 24, 25]. The use of modern high-viscosity programmable valves offers the possibility to avoid the second surgical procedure, which is not risk-free. In a systematic review by Xu et al. [31], programmable shunts had significantly lower rate of revision ((RR = 0.56, 95%CI (0.45,0.69), p < 0.01) in favour of programmable valves) in hydrocephalus as compared to fixed pressure shunts due to the lower incidence of blockage in presence of high-viscosity fluids. Hence, the same may also be applied in drainage of chronic sub-durals. There are few studies which mention that burr hole with subdural drain placement is a better option for management of cSDH in adults [26,27,28,29]. The implementation of the same procedure is not feasible in the paediatric age group especially infants because of difficulty in keeping the patients restricted to bed. This leads to accidental removal of the drain and also increasing the risk of infection [2].
We have used burr hole evacuation method for 27 patients, and three patients were managed medically. Subdural drain was used only in three of our patients, and all three had recurrence. The decision to put drain during surgery was decided intra-operatively by the treating physician depending on whether or not the brain was surfacing. Interestingly, recurrence with the use of drain was higher in our series (100% vs 30%). This may be due to the selective use of the same in cases where the brain was atrophic and was not surfacing after hematoma evacuation. Matsuo et al. have reported that burr-hole craniotomy without subdural drain has a higher recurrence rate but lower complication as compared to SPS [2].
Huang et al. have used atorvastatin (daily 2.5–5 mg) and dexamethasone (tapering dose for 4 weeks) to treat recurrent paediatric cSDH with good results [5]. There was no further recurrence at 4 years of follow up. No adverse events were noted during the medical management in the above recurrent cases. According to the above authors, atorvastatin can promote cSDH absorption by reducing local inflammation and promoting angiogenesis. In a recent randomised controlled trial [32] in adults with chronic sub-durals which included 748 patients — 375 were assigned to the dexamethasone group and 373 to the placebo group — a favourable outcome was reported in 286 of 341 patients (83.9%) in the dexamethasone group and in 306 of 339 patients (90.3%) in the placebo group. It was thus concluded that treatment with dexamethasone resulted in fewer favourable outcomes and more adverse events than placebo at 6 months, but fewer repeat operations were performed in the dexamethasone group. The same idea may be worth exploring in future cases of paediatric sub-durals.
Recurrence and outcome
The recurrence rate in our study was 30% irrespective of the use of subdural drain in three cases. Matsuo et al. have reported recurrence rate of 20% in their study of children under age of 2 years [2]. The above authors also could not find any predictive factors of recurrence in their study. Zouros et al. have studied 5 infants of cSDH, who were treated with burr hole and subdural drain with good outcome [1]. So, there is no large study in paediatric cSDH to guide the use of subdural drain after burr hole drainage. Clearly, these patients need to be followed for a longer period to determine socio-economic and academic outcome; not only the surgical and radiological outcome, prospective longitudinal study is the need of these patients.
Conclusion
cSDH in the paediatric population is rare and should always alert the physicians to look for the underlying cause especially child abuse. Detailed haematological, coagulation profile, skeletal X-rays and fundus examination should be performed whenever child abuse is suspected. Surgery forms the main stay of intervention. However, recent study has shown the promising result by use of dexamethasone and atorvastatin for selected group of recurrent cSDH. Recurrence rate is quite high irrespective of use of subdural drain. Gender, laterality, coagulopathy, previous shunts or none of the other predisposing factors were predictive for the recurrence in the current study, but larger sample size is required to be certain. Shunt patients had significant number of bilateral cases; hence, primary tumour excision with avoidance of shunt surgery should be the goal, and more enquiry should be done specifically on shunt-induced cSDH as these are essentially iatrogenic; timely intervention in this age group is as vital as their adult counterpart or may be more in case of infants where the brain is still developing to achieve the best outcome and to prevent any permanent long-term sequelae.
References
Zouros A, Bhargava R, Hoskinson M, Aronyk KE (2004) Further characterization of traumatic subdural collections of infancy. Report of five cases. J Neurosurg 100:512–518. https://doi.org/10.3171/ped.2004.100.5.0512
Matsuo K, Akutsu N, Otsuka K et al (2016) The efficacy and safety of burr-hole craniotomy without continuous drainage for chronic subdural hematoma and subdural hygroma in children under 2 years of age. Child’s nervous system: ChNS: official journal of the International Society for Pediatric Neurosurgery 32:2369–2375. https://doi.org/10.1007/s00381-016-3233-9
Parent AD (1992) Pediatric chronic subdural hematoma: a retrospective comparative analysis. Pediatr Neurosurg 18:266–271. https://doi.org/10.1159/000120674
Swift DM, McBride L (2000) Chronic subdural hematoma in children. Neurosurg Clin N Am 11:439–446. https://doi.org/10.1016/S1042-3680(18)30106-2
Huang J, Li L, Zhang J et al (2019) Treatment of relapsed chronic subdural hematoma in four young children with atorvastatin and low‐dose dexamethasone. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy 39:783–789. https://doi.org/10.1002/phar.2276
Erşahin Y, Mutluer S, Kocaman S. Continuous external subdural drainage in the management of infantile subdural collections: a prospective study. Childs Nerv Syst. 1997 Oct;13(10):526-9. https://doi.org/10.1007/s003810050131. PMID: 9403200
Hwang SK, Kim SL. Infantile head injury, with special reference to the development of chronic subdural hematoma. Childs Nerv Syst. 2000 Sep;16(9):590-4. https://doi.org/10.1007/s003810000312. PMID: 11048634.
Vinchon M, Noulé N, Soto-Ares G, Dhellemmes P (2001) Subduroperitoneal drainage for subdural hematomas in infants: results in 244 cases. J Neurosurg 95:249–255. https://doi.org/10.3171/jns.2001.95.2.0249
Mori K, Yamamoto T, Horinaka N, Maeda M (2002) Arachnoid cyst is a risk factor for chronic subdural hematoma in juveniles: twelve cases of chronic subdural hematoma associated with arachnoid cyst. J Neurotrauma 19:1017–1027. https://doi.org/10.1089/089771502760341938
Lin CL, Hwang SL, Su YF et al (2004) External subdural drainage in the treatment of infantile chronic subdural hematoma. Journal of Trauma - Injury, Infection and Critical Care 57:104–107
Kurschel S, Puget S, Bourgeois M et al (2007) Factors influencing the complication rate of subduroperitoneal shunt placement for the treatment of subdural hematomas in infants. J Neurosurg 106:172–178. https://doi.org/10.3171/ped.2007.106.3.172
Blauwblomme T, di Rocco F, Bourgeois M et al (2015) Subdural to subgaleal shunts: alternative treatment in infants with nonaccidental traumatic brain injury?. J Neurosurg Pediatr 15:306–309. https://doi.org/10.3171/2014.9.PEDS1485
Murat A, Murat Musluman A, Ozoner B et al (2018) Chronic subdural hematoma associated with arachnoid cyst of the middle fossa: surgical treatment and mid-term results in fifteen patients. Turk Neurosurg 28(5):776–782. https://doi.org/10.5137/1019-5149.JTN.21513-17.3
Nguyen VN, Wallace D, Ajmera S et al (2020) Management of subdural hematohygromas in abusive head trauma. Clin Neurosurg 86:281–287. https://doi.org/10.1093/neuros/nyz076
Tinois J, Bretonnier M, Proisy M et al (2020) Ruptured intracranial arachnoid cysts in the subdural space: evaluation of subduro-peritoneal shunts in a pediatric population. Child’s Nervous System 36:2073–2078
Wright JN, Feyma TJ, Ishak GE et al (2019) Subdural hemorrhage rebleeding in abused children: frequency, associations and clinical presentation. Pediatr Radiol 49:1762–1772. https://doi.org/10.1007/s00247-019-04483-5
Palmer AW, Albert GW (2019) Minicraniotomy with a subgaleal pocket for the treatment of subdural fluid collections in infants. J Neurosurg Pediatr 23:480–485. https://doi.org/10.3171/2018.11.PEDS18322
Caldarelli M, Di Rocco C, Romani R (2002) Surgical treatment of chronic subdural hygromas in infants and children. Acta neurochirurgica 144:581–588; discussion 588. https://doi.org/10.1007/s00701-002-0947-0
Hasegawa M, Yamashima T, Kida S, Yamashita J (1997) Membranous ultrastructure of human arachnoid cells. J Neuropathol Exp Neurol 56:1217–1227. https://doi.org/10.1097/00005072-199711000-00006
Wang H-K, Chen H-J, Lu K et al (2010) A pediatric chronic subdural hematoma after dodgeball head injury. Pediatr Emerg Care 26:667–668. https://doi.org/10.1097/PEC.0b013e3181f05475
Aoki N (1990) Chronic subdural hematoma in infancy. Clinical analysis of 30 cases in the CT era. J Neurosurg 73:201–205. https://doi.org/10.3171/jns.1990.73.2.0201
Christensen E, Husby J (1963) Chronic subdural hematoma in infancy. Acta Neurol Scand 39:323–342. https://doi.org/10.1111/j.1600-0404.1963.tb05334.x
Suh DY, Davis PC, Hopkins KL et al (2001) Nonaccidental pediatric head injury: diffusion-weighted imaging findings. Neurosurg 49:309–318; discussion 318–20. https://doi.org/10.1097/00006123-200108000-00011
Litofsky NS, Raffel C, McComb JG (1992) Management of symptomatic chronic extra-axial fluid collections in pediatric patients. Neurosurgery 31:445–450. https://doi.org/10.1227/00006123-199209000-00009
Melo JRT, Di Rocco F, Bourgeois M et al (2014) Surgical options for treatment of traumatic subdural hematomas in children younger than 2 years of age. J Neurosurg Pediatr 13:456–461. https://doi.org/10.3171/2014.1.PEDS13393
Almenawer SA, Farrokhyar F, Hong C et al (2014) Chronic subdural hematoma management. Ann Surg 259:449–457. https://doi.org/10.1097/SLA.0000000000000255
Liu W, Bakker NA, Groen RJM (2014) Chronic subdural hematoma: a systematic review and meta-analysis of surgical procedures. J Neurosurg 121:665–673. https://doi.org/10.3171/2014.5.JNS132715
Santarius T, Kirkpatrick PJ, Ganesan D et al (2009) Use of drains versus no drains after burr-hole evacuation of chronic subdural haematoma: a randomised controlled trial. The Lancet 374:1067–1073. https://doi.org/10.1016/S0140-6736(09)61115-6
Tsutsumi K, Maeda K, Iijima A et al (1997) The relationship of preoperative magnetic resonance imaging findings and closed system drainage in the recurrence of chronic subdural hematoma. J Neurosurg 87:870–875. https://doi.org/10.3171/jns.1997.87.6.0870
Wright D, Pereira EA, Magdum SA (2015) A pediatric chronic subdural hematoma: more than meets the eye. J Pediatr Neurosci 10(4):376–378. https://doi.org/10.4103/1817-1745.174451
Xu H, Wang ZX, Liu F, Tan GW, Zhu HW, Chen DH (2013) Programmable shunt valves for the treatment of hydrocephalus: a systematic review. Eur J Paediatr Neurol 17(5):454–461. https://doi.org/10.1016/j.ejpn.2013.04.001 (Epub 2013 Jul 3 PMID: 23830575)
Hutchinson PJ, Edlmann E, Bulters D, Zolnourian A, Holton P, Suttner N, Agyemang K, Thomson S, Anderson IA, Al-Tamimi YZ, Henderson D, Whitfield PC, Gherle M, Brennan PM, Allison A, Thelin EP, Tarantino S, Pantaleo B, Caldwell K, Davis-Wilkie C, Mee H, Warburton EA, Barton G, Chari A, Marcus HJ, King AT, Belli A, Myint PK, Wilkinson I, Santarius T, Turner C, Bond S, Kolias AG (2020) British Neurosurgical Trainee Research Collaborative; Dex-CSDH Trial Collaborators. Trial of Dexamethasone for Chronic Subdural Hematoma. N Engl J Med. 31;383(27):2616–2627. https://doi.org/10.1056/NEJMoa2020473. Epub 2020 Dec 16
Author information
Authors and Affiliations
Contributions
HD, AJ: collection of data and writing of manuscript; HD, RG: concept and idea and critical revisions; DS: study supervision and critical revisions; VV: supervision and critical revisions; SK: supervision and critical revisions; ARP: supervision and critical revisions; AS: supervision and critical revision.
Corresponding author
Ethics declarations
Ethics approval
Study design is retrospective; hence, approval of ethical committee was not sought.
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Deora, H., Mishra, A., Gupta, R. et al. Paediatric chronic subdural haematoma: what are the predisposing factors and outcomes in management of these cases?. Childs Nerv Syst 38, 123–132 (2022). https://doi.org/10.1007/s00381-021-05341-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-021-05341-2