Abstract
Purpose
Paediatric spine trauma is uncommon and is managed differently from adults due to the anatomical differences of the paediatric spine. The paediatric spine is less ossified, with lax ligaments and a higher fulcrum in the c-spine which results in a different pattern of injuries. The aim of this study is to provide a contemporary audit of paediatric spinal trauma.
Methods
A retrospective review was conducted using the Trauma and Audit Research Network database at a major trauma centre (2011–2018). All patients < 18 years old with a spine injury underwent case note and radiology review.
Results
A total of 72 patients (37, 51.4% male with an average age of 13.3 (± 5.9) years old) were identified. The most common mechanism of injury was road traffic collisions (n = 39, 54.2%). The most common sporting cause was motocross accidents (n = 6, 8.3%), and a further 6 (8.3%) patients had a suspected inflicted injury. Eight patients (11.1%) sustained a spinal cord injury. Twenty-seven (37.5%) patients underwent surgical intervention to treat their spinal injury.
Conclusion
This series demonstrates the profile of injury mechanisms causing paediatric spinal injuries. Paediatric spine injuries continue to have the potential for lifelong disability and require careful, specialist management. This series also highlights certain causes such as motocross accidents and suspected inflicted injury which are more frequent than expected and raise potential public health concerns.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Paediatric spinal trauma occurs rarely and represents 2.7–9% of all spinal injuries [1]. However, the significance of the injuries must not be overlooked as they often affect the cervical spine and result in devastating medical and socioeconomic consequences [2, 3].
The paediatric and adult spines have different biomechanical properties resulting in different injury profiles. In young children (0–4 years), their head is much larger relative to their body size which leads to occipito-atlantal instability and a susceptibility to spinal injuries between C0 and C2 [4, 5]. By the age of 14, the spine has developed such that the injury pattern is similar to adults, with the majority of injuries affecting the lower cervical and thoracolumbar region [6].
Patient age influences not only the type of injury but also the aetiology. Whilst the most common cause for paediatric spine trauma in all ages is road traffic collision (RTC), as children grow older, trauma caused by falls decreases and spinal trauma caused by sport increases [7]. Unfortunately, there also remains a cohort of very young paediatric patients who suffer from spinal trauma after suspected inflicted injury [8].
Previous studies investigating paediatric spinal trauma have often focused on specific types and/or severities of injury [9,10,11,12]. The aim of this study was to present a cohort of all paediatric spinal trauma patients who presented to a UK major trauma centre over an 8-year period and determine the demographics, management, and outcomes of this cohort.
Method
A retrospective review was conducted using the Trauma and Audit Research Network (TARN) database to identify patients who presented to a single tertiary neurosurgical centre. This neurosurgical centre is located in the South of England and covers a population of approximately 3 million people. The inclusion criteria were children < 18 years old at the time of presentation who were admitted between January 2011 and December 2018 with a spine Abbreviated Injury Scale (AIS) score ≥ 2. Both isolated spinal injuries and polytrauma were included. Polytrauma was defined as spine injury (AIS ≥ 2) plus injury to a non-spine region with an AIS ≥ 2. Paediatric patients within the catchment area of the neurosurgical centre who remained in their district general hospital were not included.
The TARN database provided data on demographics, mechanism of injury, injury intent, injuries sustained, Injury Severity Score (ISS), Glasgow Coma Score (GCS), length of stay (LOS), and Glasgow Outcome Score (GOS) at discharge and at 3 months after injury. The mechanism of injury was classified as follows: fall < 2 m, fall > 2 m, RTC, blow, and other. A blow includes being stuck by any blunt object including weapons or body parts. Injury intent was classified as follows: non-intentional, sport, suspected high-risk behaviour, suspected child abuse, suspected self-harm, and intent uncertain, as per the TARN database. High-risk behaviour includes any intentional activity with a foreseeable risk of sustaining injury above routine day-to-day activities.
The hospital’s electronic record system was also reviewed for details on neurological examination, management of the spinal injury, and complications. Additionally, the Picture Archive and Communication System was reviewed and the spinal injury and neurological injury were classified according to the AOSpine tool (Tables 1 and 2) [13, 14].
To allow for subgroup analysis, age groups were split into infants and toddlers (0–4 years), young children (5–13 years), and teenage children (14–18 years). These age groups were used to maintain consistency with previous case series and reflect the different stages of development of the paediatric spine [5, 9]. The GOS was dichotomised into favourable outcome (GOS 4–5) and unfavourable outcome (GOS 1–3).
Statistical analysis used a combination of descriptive methods (mean, standard error, frequency, and percentages) and quantitative analysis using t test and chi-squared tests. Statistical significance was set at p < 0.05. All data was analysed using IBM SPSS Statistics (Version 25).
Results
Demographics
The search of the TARN database found 72 eligible patients who attended the University Hospital Southampton between January 2011 and December 2018. The average age was 13.3 (± 5.9) years old and 37 (51.4%) of the patients were male. The age distribution of the cohort was skewed towards teenage years with 51 patients (67.7%) aged 14–18 years old (Fig. 1).
Mechanism of injury
The most common mechanism of injury was RTC (n = 39, 54.2%), followed by fall > 2 m (n = 14, 19.4%), fall < 2 m (n = 10, 13.9%), blow(s) (n = 6, 8.3%), and other (n = 3, 4.2%). The most common age group in RTCs was children aged 14–18 years old (n = 32, 82.1%). Eleven of the patients involved in an RTC were pedestrians or cyclists. The most common age group to be injured following blow(s) was children aged 0–4 years old (n = 4, 66.7%) (Fig. 1). There was a difference (p < 0.0001) in the distribution of mechanisms between genders with female patients sustained more spinal trauma from falls and male patients sustained more spinal trauma from RTC and blow(s) (Table 3).
The majority of the intent were either non-intentional (n = 45, 62.5%) or the result of sport (n = 11, 15.3%). The other intents were suspected child abuse (n = 6, 8.3%), self-harm (n = 5, 6.9%), and high-risk behaviour (n = 5, 6.9%) (Fig. 2). The most common sport to cause injury was motocross (n = 6), followed by trampolining (n = 3), cycling (n = 2), and rugby (n = 2). The most common age group for injury caused by sports was 14–18 years old (n = 11, 84.6%). Suspected child abuse was only seen in children aged 0–4 years old (n = 6, 100%) (Fig. 3).
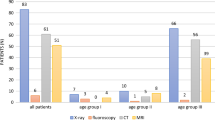
Spinal injuries
Sixty-three patients had a total of 150 fractures consisting of the following: one fracture (n = 26, 36.1%), two fractures (n = 15, 20.8%), three fractures (n = 9, 12.5%), four fractures (n = 6, 8.3%), five fractures (n = 4, 5.6%), seven fractures (n = 1, 1.4%), and eight fractures (n = 2, 2.8%). The most common region of the spine to sustain a fracture was thoracic (n = 82, 54.7%) followed by lumbar (n = 36, 24.0%), subaxial (C3–7) cervical (n = 29, 19.3%), and upper (C1–2) cervical (n = 3, 2.0%) (Fig. 4). The relationship between the spinal injury present and the resulting neurological injury classified by the AOSpine system is shown in Table 4.
Three patients had ligamentous injuries without bony fracture, all of which affected the upper cervical spine resulting in atlanto-axial subluxation. These three patients had a younger mean age than those with fractures (n = 3, 4.5 years vs n = 63, 14.25 years, p = 0.012). Only one of the three had an MRI with the others having their injury identified on CT, and none of the three required surgical intervention. Six patients suffered from an isolated subdural haematoma of the spine, all of which were the result of suspected child abuse. In these patients, the spinal subdural haematomas were found in conjunction with traumatic brain injuries.
Neurological injury
No neurological injury (N0) was reported for 29 patients (40.3%) following their spinal trauma, with a further 8 patients (11.1%) suffering from transient neurology (N1) and 15 patients (20.8%) suffering from radicular symptoms only (N2). Eight patients (11.1%) suffered from a spinal cord injury. In 12 (16.7%) patients, it was not possible to establish the neurological injury immediately after injury because of sedation or head injury (NX). Of these patients, three were never assessed due to death and the remainder had GOS 5 (n = 2), GOS 4 (n = 3), and GOS 3 (n = 4) at a 3-month follow-up. The distribution of the most severe neurological deficit of each patient, and its corresponding spinal injury, is shown in Table 4.
Associated injuries
Twenty patients (27.8%) had a clinically isolated spine injury, and the remaining patients (n = 52, 72.2%) had an injury to at least one other body part. Based on the AIS, in 32 of the patients with polytrauma (61.5%), their most severely injured body region was not the spine. These patients had the most severe injuries to the head (n = 23), multiple areas (n = 10), and chest (n = 6).
The mean ISS was 22.0 ± 13.4 and the mean GCS at presentation was 12.9 ± 4.2. The mean LOS was 17.6 days ± 26.5 days, and 38 (52.8%) patients were admitted to the intensive care unit during their time in hospital. The patients with an isolated spine trauma (n = 20) had a significantly lower ISS score than the polytraumas (9.7 ± 4.2 vs 27.2 ± 12.1, p < 0.001). The isolated spinal injury group also had a significantly higher GCS at presentation compared to patients with polytrauma (15.0 ± 0.2 vs 12.0 ± 4.8, p < 0.001).
Management
Forty-one patients (56.9%) were managed conservatively, 27 patients (37.5%) were treated surgically, and four patients (5.6%) were treated palliatively due to associated catastrophic brain injury. Patients who had thoracic or lumbar fractures underwent surgical fixation via posterior screw/rod instrumentation (n = 21, 77.8%). The patients with fractures in the cervical spine underwent either anterior cervical discectomy and fusion (n = 4, 14.8%), corpectomy with strut graft (n = 1, 3.7%), or corpectomy with iliac graft and lateral mass screws (n = 1, 3.7%).
Outcome
Thirty-five (48.6%) patients achieved a GOS of 5 at the 3-month follow-up. The remaining outcomes were GOS 4 (n = 21, 29.2%), GOS 3 (n = 12, 16.7%), and GOS 1 (n = 4, 5.6%). Of the 16 patients with an unfavourable outcome (GOS 1–3), 15 patients suffered from polytrauma and one patient had suffered from isolated spinal injury. Unfavourable outcome was significantly more likely in polytrauma (p = 0.021). Additionally, the need for surgical intervention was not associated with a lower rate of favourable outcomes compared to patients managed conservatively (n = 22, 81.4% vs n = 33, 80.5%; p = 0.92).
There is a trend that patients in the youngest age group (0–4 years) had the lowest GOS scores; however, it was not possible to confirm this with statistical methods due to low patient numbers in this group (Fig. 5). All 6 patients with suspected child abuse and a spinal injury were in the 0–4 years age group and had an outcome of GOS 1 (n = 3), GOS 3 (n = 1), GOS 4 (n = 4), and GOS 5 (n = 1) (Table 5).
At 3 months post-injury, 48 (66.7%) patients were able to walk unaided and seven (9.7%) patients ambulated with assistance. Ten (13.9%) patients were using a wheelchair and one (1.4%) patient was bed bound. It was not possible to assess the effect of spinal injury on ambulation status in six (8.3%) patients due to death, significant lower limb trauma, or severe head injury.
The mean length of follow-up after injury was 5.7 months ± 4.7 months. Six (8.3%) patients did not attend follow-up due to either death (n = 4) or lack of symptoms on discharge (n = 2). The majority of patients were discharged to their usual residence (n = 43, 59.7%), with the remaining patients being discharged to neurorehabilitation services (n = 16, 22.2%), repatriated to a local hospital for further care (n = 5, 6.9%), referred to Child and Adolescent Mental Health Services (CAMHS) (n = 2, 2.8%), and other (n = 2, 2.8%) (Fig. 6).
Discussion
Spinal trauma is uncommon in children and is estimated to represent only 2.7–9.0% of all spinal injuries [1]. Spinal trauma in children carries significant morbidity and mortality for affected children [2, 3]. Given the uncommon nature of paediatric spinal trauma, the current literature is limited to case series often focussing on a particular type of injury [11, 15, 16]. The aim of this study was to describe the injuries, management, and outcome of paediatric spinal trauma in a single UK major trauma centre.
The most common age group in this study population was children in their teenage years (14–18 years old). In this age group, children act independently often without adult supervision and have access to road traffic vehicles. Subsequently, the most common cause of spinal trauma was RTCs, particularly males aged 14–18 years old. In developed countries, safer cars (crumple zones, air bags, and three-point seat belts), safer roads, mandatory licencing tests, and alternative methods of transport have led to an overall decrease in adult spinal injury from RTCs [17]. In a study describing paediatric spinal trauma between 1988 and 1998, 61% of injuries were due to RTCs [15]. This is similar to the proportion of spinal trauma caused by RTCs observed in this contemporary study. It has previously been shown that the majority of spinal trauma caused by RTCs occurs in children aged 16–17 who are occupants in the vehicle and seated in either the driver’s or front-passenger seat [12]. It is legal to drive from the age of 17 in the UK, and therefore, it is possible that more stringent driving tests and safety regulations are required to reduce paediatric spinal trauma caused by RTCs.
Sports-related paediatric spine trauma was most commonly due to motocross or gymnastics. In the UK, children as young as 7 years old can participate in motocross which is high risk for injuries when you combine high speeds, risk of falling onto a hard surface, and immature spinal development. In light of the high proportion of paediatric injuries due to a single sport, the safety guidelines may need reviewing. All three cases of gymnastics involved children using a trampoline, which is a known risk of paediatric spinal trauma, especially when there is no protective netting [16]. Spinal trauma from team sports such as rugby occurred less frequently. In recent years, organised sport has benefitted from an increase in safety measures such as teaching safe tackling technique from an early age in rugby [18]. Future targeted prevention strategies may be appropriate in reducing injuries from organised sport, and longitudinal studies will show the impact of these rules in reducing paediatric sporting spine injuries.
There was a group of patients in this cohort with spinal trauma caused intentionally which has scarcely been described in the literature. Intentional intent causing spinal trauma observed in this study was due to suspected inflicted injury, self-harm, and high-risk behaviour such as jumping from large heights. In all children below the age of 1 year, spinal trauma was caused by suspected inflicted injury. This is consistent with a previous study which showed that child abuse disproportionately affects young children below 2 years old [19]. As a result, clinicians should suspect inflicted injury in young child with spinal trauma to identify children at risk.
The fractures seen in the study population predominately occurred in the thoracic and lumbar spine, whilst subluxation/dislocation injuries occurred in the cervical spine. Some previous studies have reported the cervical spine as the most common region [5, 20]; however, in studies with similar age distributions to the present one, i.e. older teenagers, thoracic and lumbar fractures were also the most common [1, 2]. As a result of the teenage population with mature, adult-like spines, the fractures that occurred in the study were predominantly compression fractures which are not typically associated with severe neurological injury [21].
Due to the elasticity of the bony-ligamentous spine, children less than 8 years old may also sustain a Spinal Cord Injury Without Radiological Abnormality (SCIWORA). The term SCIWORA was originally applied to the absence of injury on plain radiographs, tomography, or myelography in the pre-MRI era [22]. In this series, 3 patients had signs of only ligamentous injury but none of the patients was diagnosed with SCIWORA. The addition of MRI to the assessment of traumatic spinal cord injuries is likely to find a radiological abnormality not visible with x-rays resulting in the diagnosis of SCIWORA becoming much less common in the modern era. Higher resolution CT scanning can also identify malalignment which signifies underlying ligamentous injury, and the use of CT alone may be appropriate in low energy mechanisms. There is limited evidence to support the choice of MRI or CT to rule out spine injury, and the current NICE guidelines (NG41) suggest a combination of the Canadian C-spine rules and clinical judgement on an individual patient basis to guide the decision upon whom to perform an MRI.
When deciding on the management of fractures, a systematic approach was taken considering the stability of the fracture, the severity of neurological injury present, the burden of associated injuries, and the propensity for healing. In this study, the majority of spinal trauma was managed conservatively (n = 43, 57.3%) which is consistent with previous studies [4, 10, 23]. In a 47-year follow-up of thoracic and lumbar vertebral fractures, Karlsson et al. observed that a fractured growing spine has the capacity to remodel and reduce fracture deformities [24]. This is in stark contrast with adult spinal fractures that are at risk of developing post-traumatic kyphosis [21]. There was no significant difference between the outcomes of surgically and conservatively managed patients.
The majority of patients had a GOS showing a good or moderate recovery 3 months after the initial injury. Patients in the youngest age group (0–4 years) appeared to have worse outcomes than older children and a strong association with child abuse. NAI is often accompanied by traumatic brain injury and thus high mortality.
The limitations of the study are that it is a retrospective analysis of cases from a single trauma centre. Minor paediatric spine injuries managed in district general hospitals will not be represented, and thus, the results skewed towards more severe injuries. As a single-centre series, it may not be a representative of other regions in the UK and the results affected by local management preferences.
Conclusion
This study describes paediatric spinal trauma in heterogenous population that presented to a single tertiary neurosurgical centre. RTCs were the principal cause of spinal trauma, which disproportionately affected children aged 14–18 years old. The majority of spinal fractures occurred in the thoracolumbar region and were managed conservatively with good outcomes, 3 months after injury. Patients with isolated spinal trauma had significantly better short- and long-term outcomes than patients with polytrauma.
References
Saul D, Dresing K (2018) Epidemiology of vertebral fractures in pediatric and adolescent patients. Pediatr Rep 10:17–23. https://doi.org/10.4081/pr.2018.7232
Kim C, Vassilyadi M, Forbes JK, Moroz NWP, Camacho A, Moroz PJ (2016) Traumatic spinal injuries in children at a single level 1 pediatric trauma centre: report of a 23-year experience. Can J Surg 59:205–212. https://doi.org/10.1503/cjs.014515
Zonfrillo MR, Zaniletti I, Hall M, Fieldston ES, Colvin JD, Bettenhausen JL, Macy ML, Alpern ER, Cutler GJ, Raphael JL, Morse RB, Sills MR, Shah SS (2016) Socioeconomic status and hospitalization costs for children with brain and spinal cord injury. J Pediatr 169:250–255. https://doi.org/10.1016/j.jpeds.2015.10.043
Cirak B, Ziegfeld S, Knight VM, Chang D, Avellino AM, Paidas CN (2004) Spinal injuries in children. J Pediatr Surg 39:607–612. https://doi.org/10.1016/j.jpedsurg.2003.12.011
Dickman CA, Rekate HL, Sonntag VKH, Zabramski JM (1989) Pediatric spinal trauma: vertebral column and spinal cord injuries in children. Pediatr Neurosurg 15:237–256. https://doi.org/10.1159/000120476
Resid Onen M, Naderi S (2015) J Spine Pediatr Spine Trauma:4. https://doi.org/10.4172/21657939.1000211
Bilston Lynne E, Brown Julie E (2007) Pediatric spinal injury type and severity are age and mechanism dependent. Spine (Phila Pa 1976) 32:2339–2347. https://doi.org/10.1097/BRS.0b013e3181558886
Barnes PD, Krasnokutsky MV, Monson KL, Ophoven J (2008) Traumatic spinal cord injury: accidental versus nonaccidental injury. Semin Pediatr Neurol 15:178–184. https://doi.org/10.1016/j.spen.2008.10.009
Dauleac C, Beuriat PA, Di Rocco F et al (2019) Surgical management of pediatric spine trauma: 12 years of experience. World Neurosurg 126:e1494–e1502. https://doi.org/10.1016/j.wneu.2019.03.134
Dogan S, Safavi-Abbasi S, Theodore N, Chang SW, Horn EM, Mariwalla NR, Rekate HL, Sonntag VKH (2007) Thoracolumbar and sacral spinal injuries in children and adolescents: a review of 89 cases. J Neurosurg Pediatr 106:426–433. https://doi.org/10.3171/ped.2007.106.6.426
Mortazavi M, Gore PA, Chang S, Tubbs RS, Theodore N (2011) Pediatric cervical spine injuries: a comprehensive review. Childs Nerv Syst 27:705–717. https://doi.org/10.1007/s00381-010-1342-4
Castranova V, Asgharian B, Sayre P et al (2016) Motor vehicle crash–related injury causation scenarios for spinal injuries in restrained children and adolescents MARK. 15:1922–2013. https://doi.org/10.1080/15389588.2014.934959.Motor
Vaccaro AR, Koerner JD, Radcliff KE, Oner FC, Reinhold M, Schnake KJ, Kandziora F, Fehlings MG, Dvorak MF, Aarabi B, Rajasekaran S, Schroeder GD, Kepler CK, Vialle LR (2016) AOSpine subaxial cervical spine injury classification system. Eur Spine J 25:2173–2184. https://doi.org/10.1007/s00586-015-3831-3
Vaccaro AR, Oner C, Kepler CK, Dvorak M, Schnake K, Bellabarba C, Reinhold M, Aarabi B, Kandziora F, Chapman J, Shanmuganathan R, Fehlings M, Vialle L, AOSpine Spinal Cord Injury & Trauma Knowledge Forum (2013) AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976) 38:2028–2037. https://doi.org/10.1097/BRS.0b013e3182a8a381
Patel JC, Tepas JJ, Mollitt DL, Pieper P (2001) Pediatric cervical spine injuries: defining the disease. J Pediatr Surg 36:373–376. https://doi.org/10.1053/jpsu.2001.20720
Babcock L, Olsen CS, Jaffe DM, Leonard JC (2016) Cervical spine injuries in children associated with sports and recreational activities. Pediatr Emerg Care 00:1–10
Lee BB, Cripps RA, Fitzharris M, Wing PC (2014) The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord 52:110–116. https://doi.org/10.1038/sc.2012.158
Freitag A, Kirkwood G, Scharer S, Ofori-Asenso R, Pollock AM (2015) Systematic review of rugby injuries in children and adolescents under 21 years. Br J Sports Med 49:511–519. https://doi.org/10.1136/bjsports-2014-093684
Knox J, Schneider J, Wimberly RL, Riccio AI (2014) Characteristics of spinal injuries secondary to nonaccidental trauma. J Pediatr Orthop 34:376–381. https://doi.org/10.1097/BPO.0000000000000111
Knox JB, Schneider JE, Cage JM, Wimberly RL, Riccio AI (2014) Spine trauma in very young children: a retrospective study of 206 patients presenting to a level 1 pediatric trauma center. J Pediatr Orthop 34:698–702
Sayama C, Chen T, Trost G, Jea A (2014) A review of pediatric lumbar spine trauma. Neurosurg Focus 37:1–9. https://doi.org/10.3171/2014.5.FOCUS1490
Pang D, Pollack IF (1989) Spinal cord injury without radiographic abnormality in children-the SCIWORA syndrome. J Trauma - Inj Infect Crit Care 29:654–664
Erfani MA, Pourabbas B, Nouraie H, Vadiee I, Vosoughi AR (2014) Results of fusion and instrumentation of thoracic and lumbar vertebral fractures in children: a prospective ten-year study. Musculoskelet Surg 98:107–114. https://doi.org/10.1007/s12306-014-0313-4
Magnus KK, Anders M, Ralph H, Jack B, Caroline K, Acke O (2003) A modeling capacity of vertebral fractures exists during growth - an up to 47-year follow-up. Spine (Phila Pa 1976) 28:2087–2092. https://doi.org/10.1097/01.BRS.0000084680.76654.B1
Author information
Authors and Affiliations
Contributions
The drafting of the manuscript was done by Booker J, Hall S, and Dando A. In addition, the analysis and interpretation of data were done by Booker J and Hall S. The remaining authors participated in the conception and design of the study as well as the review of the manuscript. Each author participated sufficiently to meet the criteria for authorship according to ICMJE.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study did not require ethics approval because the data was collected retrospectively and presented anonymously, and had no impact on the care received by each patient.
Consent for publication
Not applicable.
Conflict of interest
The authors report no conflict of interest.
Preliminary publication
None
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Booker, J., Hall, S., Dando, A. et al. Paediatric spinal trauma presenting to a UK major trauma centre. Childs Nerv Syst 37, 1949–1956 (2021). https://doi.org/10.1007/s00381-021-05044-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-021-05044-8