Abstract
Purpose
Transcranial Doppler (TCD) has been used for more than 30 years in clinical practice. Although adult intensive care is relatively well covered, pediatric cases are still underrepresented. We intend to review a series of pediatric cases where TCD was determinant in clinical decisions and a literature review on this topic.
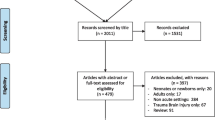
Methods
We describe cases with different pathologies where TCD had an important role in clinical management of the patients. We discuss TCD utility and potential role both in the emergency department and the intensive care unit.
Results
Five patients with different neurologic insults are presented. TCD was useful in the identification of intracranial hypertension in traumatic brain injury, hydrocephalus and central nervous system infection; identification of decreased cerebral perfusion pressure in hypovolemic shock and the diagnosis of impending cerebral circulatory arrest in a child with meningococcal septicemia. We discuss how TCD can be used in emergency and intensive care settings, reviewing relevant literature and our own experience.
Conclusions
Non-invasive testing using TCD can aid clinical decisions. More widespread use of this technique will allow for better care of children with neurologic insults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since its introduction in 1982, many authors have used transcranial Doppler (TCD) to assess cerebral blood flow velocities [1]. This technique is well established in cases of vasospasm after subarachnoid hemorrhage, arterial stenosis or occlusion, and for the diagnosis of brain death [2]. More recently, some authors have used it as an indirect and noninvasive method to estimate intracranial pressure (ICP). TCD-derived pulsatility index (PI) has been shown to have a decent correlation with cerebral perfusion pressure (CPP), ICP, and outcome in patients with severe head injury [3,4,5,6], but other reports state that these points are still controversial [7, 8]. Nevertheless, with TCD, it is possible to estimate the severity of cerebral hemodynamic disturbance after traumatic brain injury (TBI) at admission in order to establish prognosis and help deciding the level of care to be provided. However, current guidelines for treatment of these patients do not recommend its use in clinical practice because of the lack of evidence. The Brain Trauma Foundation 2012 guidelines for TBI in children states that more studies are needed to determine the optimal monitoring of these patients. It specifically includes TCD as one of the techniques that should be considered [9]. However, the feasibility of this technique is limited in the pediatric population because of the paucity of studies in children with TBI [8, 10,11,12,13].
With this case series and literature review, we intend to give further support to the use of TCD in children with TBI and other diseases where cerebral blood flow could be compromised.
All images were acquired and recorded with RIMED® Digi-Lite, using a 2 MHz pulsed wave probe.
Case reports
Case 1
A 17-year-old boy with known hydrocephalus and a ventriculoperitoneal shunt presented to the emergency department with headache. He had been diagnosed with migraine by the pediatric neurologist, but the headache persisted despite medical treatment. Ophthalmologic examination and CT scan were inconclusive and the neurosurgeon asked for a TCD. PI was increased (1.6), blood pressure was normal (123/66 mmHg), and the TCD waveform suggested intracranial hypertension. The decision to operate was based on this result and after reviewing the ventriculoperitoneal shunt, the PI normalized (Fig. 1; Table 1) and headache improved.
Case 2
A 17-year-old girl was transferred from a district hospital with severe TBI after a road traffic accident. A computed tomography (CT) scan at the referring hospital showed a subdural hematoma on the left side. At admission in the emergency department, she was sedated and ventilated (PaCO2 = 39.5 mmHg), with high arterial blood pressure (168/96 mmHg) and an urgent TCD was performed revealing severely compromised blood flow in the left middle cerebral artery (Mean flow = 18 cm/s, diastolic flow = 10 cm/s, PI = 3.6). The initial plan of monitoring ICP in the PICU was changed and she was immediately transferred to the operating room. After draining a large intracranial hematoma, TCD showed normal velocities and PI (Fig. 2; Table 1).
Case 3
A 16-year-old girl suffered a TBI and extensive abrasion lesions after falling from a horse and being dragged for several minutes. An ICP bolt was inserted and invasive monitoring revealed an ICP of 8 mmHg. Nonetheless, a TCD was performed and PI was increased (1.6) (Fig. 3; Table 1). Blood pressure was low (85/44 mmHg) due to hypovolemic shock and PI was reflecting decreased cerebral perfusion pressure. Measured CPP (ABP-ICP) was 51 mmHg. In this case, TCD results prompted treatment with fluid boluses in order to increase blood pressure and optimize cerebral blood flow. After restoring normovolemia, blood pressure normalized and so did the flow velocities and PI that decreased to 0.9 (Table 1).
Case 4
An 11-year-old boy was admitted to the pediatric intensive care unit (PICU) with severe meningococcal septicemia. After 48 h of intensive treatment with fluid boluses, inotropes, steroids, blood transfusions, and extensive fasciotomies of the lower limbs, he had a sudden neurologic deterioration with dilated pupils, absence of spontaneous respiratory trigger, and no reaction to external stimuli. An urgent TCD confirmed very high PI (7.3) with arterial hypertension (154/102 mmHg), compatible with severe intracranial hypertension and severe compromise to cerebral blood flow with no diastolic flow (Fig. 4). CT scan of the brain confirmed severe cerebral edema and the patient eventually died.
Case 5
An infant was admitted to the infectious diseases ward with pneumococcal meningitis and a subdural empyema. The neurosurgeons were reluctant to operate on such a small child due to lack of clear indications for drainage in this age group. The child was awake and showed signs of irritability, but was otherwise stable. As she was not improving, a TCD was performed and the decision to drain the empyema was based on a raised PI (1.9) with mild arterial hypertension (100/68 mmHg) and normocapnia, which was interpreted as a sign of raised ICP. After drainage, TCD was repeated and the PI was normal (Fig. 5; Table 1).
Discussion
Evaluating cerebral blood flow is essential in many disease processes. TCD is a noninvasive, bedside technique that allows direct measurement of blood flow velocities in intracranial arteries. Assuming the diameter of the insonated artery is constant, changes in the Doppler acquired flow velocities reflect changes in cerebral blood flow through that artery.
Measuring blood flow velocities allows us to calculate indices based on systolic, mean and diastolic flow velocities. One of those is the Gosling PI that is calculated from the relationship between systolic and diastolic flow velocities divided by the mean flow velocity [14]. PI has been extensively used as an estimate of ICP in adults, but its use in children is still limited. A recent review study has only found three papers between 2005 and 2015 addressing this particular interaction in children [13]. Although it has been largely interpreted as a measure of cerebral vascular resistance (CVR), it has been suggested that PI is a complex function of various hemodynamic factors and not only of CVR [7]. First of all, it is an inverse function of cerebral perfusion pressure (CPP), so, it increases both with low MAP or raised ICP. It also increases with low PaCO2, as hypocapnia raises CVR. As our case 3 shows, PI can be increased even in face of normal ICP. In this case, it reflects CPP better than ICP and even if in most cases ICP and CPP will be inversely related, we must take arterial blood pressure into account in order to correctly interpret PI. In our opinion, PI is a good measure of CPP and the higher the PI, the lower the CPP. These have been previously demonstrated by others [5, 8, 11]. Some authors use a formula to estimate CPP based on mean arterial pressure and flow velocities. Czosnyka et al. have suggested the formula “MAP x FVd/FVm +14” to estimate CPP [15]. This formula has since been used and validated by others [16, 17]. In clinical practice, being able to estimate CPP is extremely important because ultimately what matters to the patient is assuring adequate perfusion of the brain tissue.
In neurocritical care, TCD has been used in many different settings including TBI, subarachnoid hemorrhage, stroke, hydrocephalus, brain tumors, sickle cell disease, brain death, cardiac shunts, carotid surgery, central nervous system infection, liver failure, preeclampsia, and sepsis [18].
In this paper, we focus on its use in the pediatric emergency department and intensive care unit. It is a valuable tool to assess cerebral blood flow in these settings. A qualified doctor or technician can quickly evaluate the patient providing it has a good acoustic window. Fortunately, most pediatric patients do. This means that in a few minutes, with the proper equipment and expertise, one can tell how compromised perfusion is to the brain.
If used judiciously in the emergency department, it can help to make quick decisions in cases where it is not obvious what the best approach would be. It has been shown to effectively predict which patients with no severe brain lesions on CT after mild to moderate traumatic brain injury were at risk for secondary neurologic deterioration [19]. Others have demonstrated an association with poor outcome if the TCD performed in children with moderate to severe head injury at admission in the emergency department showed an end-diastolic velocity less than 25 cm/s and a PI more than 1.31 [20]. We have also used it many times to decide if children with hydrocephalus presenting to the emergency room with clinical symptoms of raised ICP need revision of their shunt or if they can be managed conservatively. In every case where TCD was suggestive of raised ICP, this was confirmed by the neurosurgeon during surgery.
Traumatic brain injury is definitely one of the major indications for using TCD in the PICU, but we have also used it successfully in many other scenarios like hydrocephalus, shock, brain death, central nervous system infections, and stroke. In the case of an acute ischemic stroke, it is possible to document the occlusion of the affected vessel and in selected cases monitor reperfusion while treating with intravenous thrombolysis [21]. We have done it successfully in a 14-year-old boy with an acute ischemic stroke. The treatment was performed under transcranial Doppler ultrasound monitoring, and recanalization of the left middle cerebral artery was documented during the first 5 min of r-TPA perfusion [22]. We have also used it in patients during extracorporeal membrane oxygenation (ECMO). These patients are not easy to move and a bedside test is of utmost importance. In these cases, we have to take into consideration the nonpulsatile flow of the ECMO system, particularly in patients with veno-arterial ECMO. Nonetheless, it could be determinant in cases of suspected stroke that unfortunately is one of the risks of the patients submitted to this technique of extracorporeal circulation. Others have also studied the role of TCD in ECMO patients, although there are no studies in children [23, 24].
Another well-established role for TCD is diagnosis and monitoring of vasospasm after subarachnoid hemorrhage (SAH). The study from Lindegaard et al. showed that there was a clear inverse relationship between the MCA diameter and MCA flow velocity [25]. He also established the limit of a mean flow velocity above 140 cm/s to define a significant vasospasm. At this velocity, the diameter of the MCA reduces to one half of its original diameter, decreasing from 3 to 1.5 mm. Many authors have validated these results and assessing vasospasm after SAH is probably the most common indication for TCD in neurocritical care [26,27,28]. Nonetheless, results should be interpreted cautiously because intermediate velocities—mean flow velocity in MCA 120–200 cm/s—may not have a good correlation with angiographic findings [29]. In our unit, we monitor every child with SAH with alternate day TCD and daily if there is vasospasm, although there are no normative values for children with SAH. We use the reference values for adults and the Lindegaard ratio to exclude hyperemia in selected cases.
In our study, we present paradigmatic cases where TCD aided clinical management. We selected these cases because they are examples of daily conditions that require an understanding of cerebral hemodynamics to guide therapy. These cases include frequent causes of intracranial hypertension like traumatic brain injury, hydrocephalus, and central nervous system infection; we also describe a case of decreased cerebral perfusion pressure in hypovolemic shock to draw attention to the fact that PI can be increased with normal ICP if CPP is compromised due to low arterial blood pressure; finally, we also give an example of a common application of TCD in diagnosing impending cerebral circulatory arrest or even complete circulatory arrest where it can aid in the establishment of brain death. This is particularly useful in cases where the clinical criteria of brainstem death cannot be applied on their own, for example is sedative substances are in circulation.
TCD is not a replacement for other established techniques of neuromonitoring, but should be included in the multimodal monitoring as a useful tool to estimate cerebral blood flow. TCD is inexpensive, noninvasive, real-time, harmless, easy to perform with the correct training, and can be done in almost all environments without having to move the patient. It can be repeated as needed, but continuous monitoring for more than 30–60 min is still challenging. New technologies are currently being developed and tested that will probably allow continuous monitoring to be feasible in the near future.
Conclusions
This case series demonstrates how TCD, a noninvasive, bedside test, can be used in different settings and aid clinical decisions. We believe that more widespread use of this inexpensive technique would allow a better care of children with neurologic insults and that it truly represents a noninvasive window to cerebral blood flow.
References
Aaslid R, Markwalder TM, Nornes H (1982) Noninvasive transcranial Doppler ultrasound recording of flow velocity in basal cerebral arteries. J Neurosurg 57(6):769–774
American Academy of Neurology (1990) T and TAS. Assessment: transcranial Doppler. Neurology 40:680–681
Goraj B, Rifkinson-Mann S, Leslie DR, Lansen TA, Kasoff SS, Tenner MS (1994) Correlation of intracranial pressure and transcranial Doppler resistive index after head trauma. AJNR Am J Neuroradiol 15:1333–1339
Moreno JA, Mesalles E, Gener J, Tomasa A, Ley A, Roca J et al (2000) Evaluating the outcome of severe head injury with transcranial Doppler ultrasonography. Neurosurg Focus 8(1):e8
Bellner J, Romner B, Reinstrup P, Kristiansson K-A, Ryding E, Brandt L (2004) Transcranial Doppler sonography pulsatility index (PI) reflects intracranial pressure (ICP). Surg Neurol 62(1):45–51 Available from: http://linkinghub.elsevier.com/retrieve/pii/S0090301904000448
Vieira F, Cardoso K, Abecasis F, Batista P, Boto L, Quintas S et al (2012) Doppler transcraniano na monitorização do traumatismo craniencefálico grave em pediatria. Acta Pediatr Port 43(6):239–245
de Riva N, Budohoski KP, Smielewski P, Kasprowicz M, Zweifel C, Steiner LA et al (2012) Transcranial Doppler pulsatility index: what it is and what it isn’t. Neurocrit Care 17(1):58–66. https://doi.org/10.1007/s12028-012-9672-6
Figaji AA, Zwane E, Fieggen AG, Siesjo P, Peter JC (2009) Transcranial Doppler pulsatility index is not a reliable indicator of intracranial pressure in children with severe traumatic brain injury. Surg Neurol. Elsevier Inc. 72(4):389–394. https://doi.org/10.1016/j.surneu.2009.02.012
Kochanek PM, Carney N, Adelson PD, Ashwal S, Bell MJ, Bratton S et al (2012) Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents—second edition. Pediatr Crit Care Med 1(1):S1–S82 Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00130478-201201001-00001
O’Brien NF, Maa T, Reuter-Rice K (2015) Noninvasive screening for intracranial hypertension in children with acute, severe traumatic brain injury. J Neurosurg Pediatr 16(4):420–425. https://doi.org/10.3171/2015.3.PEDS14521
Melo JRT, Di Rocco F, Blanot S, Cuttaree H, Sainte-Rose C, Oliveira-Filho J et al (2011) Transcranial Doppler can predict intracranial hypertension in children with severe traumatic brain injuries. Child’s Nerv Syst 27(6):979–984. https://doi.org/10.1007/s00381-010-1367-8
Reuter-Rice K (2017) Transcranial Doppler ultrasound use in pediatric traumatic brain injury. J Radiol Nurs 36(1):3–9 Available from: http://linkinghub.elsevier.com/retrieve/pii/S1546084316301900
LaRovere KL, O’Brien NF, Tasker RC (2016) Current opinion and use of transcranial Doppler ultrasonography in traumatic brain injury in the pediatric intensive care unit. J Neurotrauma 33(23):2105–2114. https://doi.org/10.1089/neu.2015.4344
Gosling R, King D (1974) Arterial assessment by Doppler-shift ultrasound. Proc R Soc Med 67:447–449
Czosnyka M, Matta BF, Smielewski P, Kirkpatrick PJ, Pickard JD (1998) Cerebral perfusion pressure in head-injured patients: a noninvasive assessment using transcranial Doppler ultrasonography. J Neurosurg 88(5):802–808. https://doi.org/10.3171/jns.1998.88.5.0802
Schmidt EA, Czosnyka M, Gooskens I, Piechnik SK, Matta BF, Whitfield PC et al (2001) Preliminary experience of the estimation of cerebral perfusion pressure using transcranial Doppler ultrasonography. J Neurol Neurosurg Psychiatry 70(2):198–204 Available from: http://eutils.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&id=11160468&retmode=ref&cmd=prlinks%5Cnpapers2://publication/uuid/A6F19E20-AF9C-4C7C-836B-124522FD4785
Gura M, Silav G, Isik N, Elmaci I (2011) Noninvasive estimation of cerebral perfusion pressure with transcranial Doppler ultrasonography in traumatic brain injury. Turk Neurosurg 22(4):411–415. https://doi.org/10.5137/1019-5149.JTN.4201-11.1
Robba C, Cardim D, Sekhon M, Budohoski K, Czosnyka M (2018) Transcranial Doppler: a stethoscope for the brain-neurocritical care use. J Neurosci Res 96(4):720–730. https://doi.org/10.1002/jnr.24148
Bouzat P, Francony G, Declety P, Genty C, Kaddour A, Bessou P et al (2011) Transcranial doppler to screen on admission patients with mild to moderate traumatic brain injury. Neurosurgery 68(6):1603–1609
Trabold F, Meyer PG, Blanot S, Carli P, Orliaguet G (2004) The prognostic value of transcranial Doppler studies in children with moderate and severe head injury. Intensive Care Med 30(1):108–112 Available from: http://www.ncbi.nlm.nih.gov/pubmed/14600812
Levi C, Zareie H, Parsons M (2012) Transcranial Doppler in acute stroke management—a “real-time” bed-side guide to reperfusion and collateral flow. Perspect Med 1(1–12):185–193. https://doi.org/10.1016/j.permed.2012.02.044
Sampaio I, Abecasis F, Quintas S, Moreno T, Camilo C, Vieira M et al (2011) Successful intravenous thrombolysis in a 14-year-old boy with ischemic stroke. Pediatr Emerg Care 27(6):541–543
Kavi T, Esch M, Rinsky B, Rosengart A, Lahiri S, Lyden PD (2016) Transcranial Doppler changes in patients treated with extracorporeal membrane oxygenation. J Stroke Cerebrovasc Dis. Elsevier Inc. 25(12):2882–2885. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.07.050
Marinoni M, Cianchi G, Trapani S, Migliaccio ML, Bonizzoli M, Gucci L et al (2018) Retrospective analysis of transcranial doppler patterns in veno-arterial extracorporeal membrane oxygenation patients. ASAIO J 64(2):175–182 Available from: http://insights.ovid.com/crossref?an=00002480-900000000-99032
Lindegaard K-F, Nornes H, Bakke SJ, Sorteberg W, Nakstad P (1988) Cerebral vasospasm after subarachnoid haemorrhage investigated by means of transcranial Doppler ultrasound. In: Proceedings of the 8th European Congress of Neurosurgery Barcelona, September 6–11, 1987. Springer Vienna, Vienna, pp 81–4. https://doi.org/10.1007/978-3-7091-8975-7_16
Saqqur M, Zygun D, Demchuk A (2007) Role of transcranial Doppler in neurocritical care. Crit Care Med 35(Suppl):S216–S223 Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00003246-200705001-00014
Lysakowski C, Walder B, Costanza MC, Tramèr MR (2001) Transcranial Doppler versus angiography in patients with vasospasm due to a ruptured cerebral aneurysm: a systematic review. Stroke 32(10):2292–2298
Burch CM, Wozniak MA, Sloan MA, Rothman MI, Rigamonti D, Permutt T et al (1996) Detection of intracranial internal carotid artery and middle cerebral artery vasospasm following subarachnoid hemorrhage. J Neuroimaging 6(1):8–15
Vora YY, Suarez-Almazor M, Steinke D, Martin M (1999) Role of transcranial Doppler monitoring in the diagnosis of cerebral vasospasm after subarachnoid hemorrhage. Neurosurgery 44(6):1237–1247
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Abecasis, F., Oliveira, V., Robba, C. et al. Transcranial Doppler in pediatric emergency and intensive care unit: a case series and literature review. Childs Nerv Syst 34, 1465–1470 (2018). https://doi.org/10.1007/s00381-018-3877-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-018-3877-8