Abstract
Objectives
In this study, we investigated Ommaya reservoir among pediatric patients, its infection rate, and the predisposing factors. We also investigated its role in the reduction of CSF protein. Finally, we explored other factors that would influence the decision to insert an Ommaya in comparison to external ventricular drainage.
Methods
This is a 6-year retrospective cohort study from a tertiary hospital in Saudi Arabia.
Results
In our study, females were 48.9 % (n = 22) while males were 51.1 % (n = 23). The mean age at insertion was 2.9 days, SD of 1.67 day. The mean weight at insertion was 0.98 kg, SD of 0.57 kg. The total duration of Ommaya days was 2523 days. The median duration of the reservoir was 21 days. The Ommaya reservoir infection rate was 6.6 %. We found an association between organisms cultured from urinary tract and the organisms cultured from the CSF. We also found that CSF protein level is lower in non-infected reservoirs in comparison to those with infection. The number of Ommaya days and the number of days of infection could not explain the mean CSF protein.
Conclusions
Ommaya reservoir has a low infection rate. Although CSF protein increased by infection, we failed to prove that Ommaya tapping provides a reduction in the CSF protein and, hence, reduction of shunt malfunctions thereafter. We conclude with expert opinions that take into account the psychological factors in addition to the clinical sense in choosing between Ommaya reservoir and external ventricular drainage (EVD).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hydrocephalus has an adverse neurological outcome when proper management is delayed; hence, the use of ventriculoperitoneal shunts as a permanent CSF diversion is warranted. Ommaya reservoir and external ventricular drainage (EVD) both can achieve the goal of diverging CSF as a temporary measure. In this study, we are investigating Ommaya reservoir in acute hydrocephalus among pediatric patients, its infection rate, and the predisposing factors for the infection associated with the reservoirs. Furthermore, we are examining the role of Ommaya reservoir in the reduction of CSF protein, and finally, we explore other factors that would influence the decision to insert an Ommaya in comparison to EVD.
Methods
Type of study
This is a retrospective cohort study from a single medical institute of Riyadh City, Saudi Arabia, during the period of 6 years. The study is not comprised of a comparison group; however, a comparison group is not imperative in the design of cohort studies [3]. Based on the medical records and the medical city database, every patient who underwent Ommaya reservoir insertion at our institute was eligible to be part of the study. Inclusion and exclusion criteria were then applied. Patients were selected from the database based on their medical record numbers by a third party. The third party enrolled patients by searching the anesthesia records for “Ommaya reservoir” titles. The third party has neither clinical knowledge nor knowledge about the study or the clinical status or outcome status of those patients.
Inclusion and exclusion criteria
The inclusion criteria were patients who underwent Ommaya reservoir insertion at King Fahad Medical City for the management of acute hydrocephalus and were followed at our institute during the entire period from the insertion to the removal of the reservoir. Hydrocephalus diagnosed based on the neuro-imaging investigation through a CT or MRI.
The exclusion criteria are adult patients, patients who underwent Ommaya reservoir insertion for chemotherapy, patients with missing files, and patients who were loss to follow-up. Sixty-seven patients were enrolled based on their records of Ommaya reservoir insertion. However, based on the inclusion criteria, 65 patients were included in the study and 2 were excluded. One has Ommaya inserted outside our institute and the second one was followed outside after the reservoir was inserted. Based on the exclusion criteria, 20 patients were excluded, 10 were adults, and 10 have an Ommaya reservoir for chemotherapy purposes. No missing files were encountered. Therefore, 45 patients were enrolled in our study.
Procedure and tapping
The procedure for Ommaya reservoir insertion done under full aseptic technique and a dressing were applied afterward. Each and every patient receives intravenous 1 g cefazolin pre-operatively and two doses post-operatively. Tapping is done every day or every other day depending on the clinical status of the patients. Tapping has been carried out under full aseptic technique through the use of sterile gloves in addition to chlorhexidine swab sticks and dressings were applied thereafter.
Data collection
Based on the patient’s MRN, data were collected in the form of patient’s date of birth, the age and the weight at the time of the reservoir insertion, and the date of the insertion and the date of removal. The duration of Ommaya reservoir was calculated afterwards. The CSF analysis was done in our lab and includes the protein level at the time of reservoir insertion and at the time of removal. Furthermore, reports on the culture and microscopy for every CSF sample investigated. Based on that, the number of days of infection was then calculated. Moreover, we explored the final disposition of the patients at the time of reservoir removal. This includes the insertion of VP shunt, EVD or Ommaya removal, revision, or death. Finally, any pre-Ommaya systemic infection has been investigated for every case.
CSF parameters and infection
The CSF analysis includes protein, glucose, cells, culture, and microscopy. Because CSF glucose needs to be correlated with the blood glucose and because of the high sensitivity of the protein CSF to infection [2], the focus of this study is on the CSF protein as a marker for infection. The normal range for CSF protein level is between 0.15 and 0.45 g/L. Additionally, the CSF sample is labeled infected when culture and microscopy are positive for a bacterium or a fungus in multiple consecutive occasions. This is to avoid confounding of contaminated samples. In addition, cases were labeled infected only when CSF aspirated from the reservoir has a positive culture and microscopy. Patients with coexisting infection that has the same organism isolated from Ommaya aspirate is not considered infected; however, it will be investigated as well. The reason is that because of the uncertainty and ambiguity surrounding temporal association between systemic infections and an infected CSF [6], those cases were not counted as infected. The number of the days of infection was calculated from the first positive culture and microscopy until the first negative culture and microscopy. The first negative culture and microscopy after the infection was included in the calculation.
We have used the Statistical Package for Social Science version 21 for the analysis. All the variables in the study were tested for normality, and the assumptions for statistical techniques were ensured.
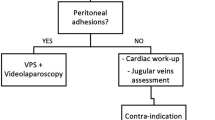
Clinical criteria and rationale for the placement of the reservoir
There are two patient categories in relation to our clinical criteria for the placement of the Ommaya reservoir. Category A includes extreme cases of spina bifida. Most of those cases are myeloschisis with a large skin defect that requires plastic surgeons joining us during the procedures for an extensive repair with skin flaps. Our patients have a higher risk for developing post-operative infection and that is the rationale behind placing an Ommaya reservoir instead of a VP shunt. Those patients apart from being referred late to our service after 48 h of birth required extensive, bilateral skin flaps, which put traction on the skin of the abdominal wall. They are nursed in the prone position, and if shunts are placed, it will compromise the skin more. Because of the high risk for infection, the shunt needs to be removed after infection and then require an EVD. When skin flaps have healed after the repair and infants are free of infections in which they have passed the high-risk window, 2–3 weeks on average, the Ommaya reservoir is replaced by a permanent shunt. However, we proceed with a ventriculoperitoneal shunt within 48 h after birth in small myelomeningoceles MMC cases that do not require skin flaps and in infants who have good skin, lax abdomen with a clear hydrocephalus. In contrary, cases with small defects that were underweight with a very thin skin that is unable to hold the shunt hardware are instead put in Ommaya reservoir.
Besides, the choice to place a reservoir instead of a VP shunt and later on converted to shunt is used in patients with other congenital anomalies requiring more diagnostic and management decisions that were not yet finalized within 48 h by the time of MMC repair. Our placement of the Ommaya reservoir in cases of MMCs and hydrocephalus is not specifically for Dandy-Walker cysts or Chiari malformations. Nevertheless, category B includes cases of prematurity and IVH requiring CSF diversion. These cases need CSF drainage for a longer period to clear the CSF from the blood due to their small weights in addition to the presence of comorbidities. Instead of placing an EVD for that long duration, we are placing an Ommaya reservoir.
Results
Patients’ characteristics
In our study, female patients were 48.9 % (n = 22) while male patients were 51.1 % (n = 23). The mean age at insertion was 2.9 days (95 % CI of 2.43 to 3.44) with SD of 1.675 day. The mean weight at insertion was 0.98 kg (95 % CI 0.79 to 1.16) with SD of 0.573 kg. However, the weight of 8.9 % of patients (n = 4) at the time of Ommaya insertion was missing from their charts.
Follow-up rate
The follow-up rate is 93.33 % with 6.67 % expired before the removal of Ommaya reservoir (n = 3). None of those three had a positive CSF culture from the time of the reservoir insertion to the last CSF tap. Those patients died due to multiple congenital anomalies based on the mortality reports.
Diagnosis and indication for Ommaya reservoir insertion
Figure 1 illustrates the diagnosis at the time of Ommaya insertion. Hydrocephalus secondary to intra-ventricular hemorrhage comprises the highest percentage of patients 35.6 % (n = 16). Arnold Chiari malformation II comprises the second highest percentage of 22.2 % of patients (n = 10). Congenital hydrocephalus has been seen in 20 % of patients (n = 9). Aqueductal stenosis has been seen in 15.6 % (n = 7), while Dandy-Walker syndrome and Arnold Chiari malformation I both have similar percentages of 2.2 % (n = 1).
The duration of Ommaya reservoir
The total duration of Ommaya days was 2523 days. The median duration of the reservoir was 21 days with IQR [7.5 to 52 days].
The infection rate
Patients with positive CSF culture were 13.3 % comprising six cases of documented CSF organisms while 39 patients have no documented infection. However, based on our criteria for Ommaya reservoir infection, three of the cases are considered infected. This is because only three cases have documented organism seen in the CSF aspirated from Ommaya. Hence, the Ommaya reservoir infection rate is 6.66 %.
The isolated organisms
Pie chart shows the isolated CSF organisms in relation to the days of infection. Enterobacter cloacae was cultured in the majority of infected CSF (Fig. 2).
Predisposing factors
The age of the patients at the time of Ommaya insertion and their weights were investigated in relation to infection and the number of Ommaya days. Neither do the age nor the weight of the patients at the time of reservoir insertion showed a significant correlation with the number of days of infection or the number of Ommaya days (P > 0.05).
CSF protein and Ommaya reservoir
A one-way between-group analysis of variance was conducted to investigate the influence of infection on the level of CSF protein. We found that there is a statistically significant result P < 0.05 of the mean CSF protein for patient with and without a documented infection. The mean CSF protein level is lower for patients without infection (M = 2.51, SD = 3.42) than those with infection (M = 6.13, SD = 4.55) with an effect size of 0.11 using the calculated eta squared. Means plot illustrating the difference in the mean for CSF protein between those with infection and non-infection reservoir (Fig. 3).
An investigation of the CSF protein at the time of Ommaya insertion and removal showed a mean value of CSF protein at the time of removal to be higher than the mean at insertion. The effect of tapping on reducing the amount of CSF protein was investigated thereafter. Paired t test analysis was used to compare the CSF protein at that time of insertion and at the time of removal. The study showed a negligible difference between the two (M = 3.06 g/L versus M = 2.92 g/L with a SD of 4.61 versus 4.13) and the difference is not statistically significant P > 0.05. In addition to that, the mean CSF protein as an outcome failed to be explained by the number of Ommaya days or the number of days of infection using regression analysis P > 0.05.
Post-Ommaya reservoir
All cases of Ommaya reservoir infection underwent EVD (100 %). While non-infected cases had either VP shunts (66.7 %) or revision or removal (20.5 %) in addition to those who expired. Bar chart illustrates the difference in the percentage for post-Ommaya between those with infection and those without (Fig. 4).
Discussion
The incidence rate of Ommaya reservoir infection: notes about the infected cases
The CSF-positive cultures in our study were 13.3 %, which resemble 6 cases out of 45 patients. However, based on our criteria for infected cases, only three out of the six patients fulfilled the criteria. In the first case, the patient already had an EVD before Ommaya reservoir was inserted. The EVD was on the right during the Ommaya duration and Ommaya was inserted on the left side. The CSF-positive culture came from the EVD, not from the Ommaya reservoir. The CSF aspirated from the Ommaya reservoir was sterile. Moreover, the same patient was considered immuno-compromised based on the immunological assessment. In the second case, the patient had a VP shunt in one site, at the same time, the Ommaya reservoir was on the other site. The positive CSF culture showed yeast infection, yet it was sampled from the VP shunt, not the Ommaya. Interestingly, these patients had septicemia just before the insertion of the reservoir in the form of positive urine culture for yeast in addition to Enterobacter aerogenes. The patient blood culture showed E. aerogenes as well. In the third case, the patient had a positive CSF culture of E. cloacae. However, 3 days later, the patient had a urine culture that showed E. cloacae. This would raise a question of temporal association and whether such organism was there on the urine before the CSF, but urine analysis has not been done earlier.
The fourth, fifth, and sixth cases were all infected cases in which the patients developed a CSF-positive culture sampled from the reservoir without having another shunt, drain, or systemic illness. Therefore, the Ommaya reservoir infection rate is 6.66 %. An infection rate of 6.6 % was reported in one study of 15 patients and a 7.7 % was seen in 48 patients out of 618 patients [8, 11]. The percentage of the Ommaya reservoir infection in our study represents one tertiary hospital in Saudi Arabia. The percentage we report is consistent with the reservoir infection rate in the USA [11] and in China [8]. Such consistency argues that even in different contexts with different policies and procedures, the percentage is still low. Despite that, the 16 years period of a study of reservoir infection was targeting patients with Ommaya inserted for chemotherapy purposes [11]. The immuno-compromised factors in those patients did not inflate the infection rate beyond the infection rate seen in patients with Ommaya for hydrocephalus purposes like the case in our study. The consistency of the low infection rate of the Ommaya reservoir gains the reservoir superiority to EVD, especially when EVD studies lack such consistency [7, 10].
Factors associated with Ommaya reservoir infection
We found no association between the age of the patient and their weight at the time of reservoir insertion and infection. However, we found an association in the organisms cultured elsewhere and the organisms cultured from the CSF.
CSF analysis: the association between Ommaya and CSF protein from repeated tapping
The high amount of protein within the CSF is linked to the shunt malfunction and CSF ascites [1, 12], although the linear association between CSF protein level and shunt malfunction has been questioned [4]. A study reported a trace of carbon within obstructed shunts that indicate a high level of protein within the CSF [12]. We hypothesized that Ommaya reservoir has a role in decreasing CSF protein, as argued in one study [9], and, hence, influence the percentage of shunt malfunctions.
CSF protein and Ommaya tapping
Our study fails to prove the claim that Ommaya has a role in reducing the amount of CSF protein from the continuous tapping. In addition to that, the CSF protein was investigated in terms of infection, number of Ommaya days, and number of infected days. We found a statistically significant result with a higher amount of CSF protein seen in infected reservoirs while no significant association between the number of Ommaya days and the number of infected days.
The impact of systemic infection
Two out of the six patients with positive CSF cultures had a coexisting systemic infection. Here, those two cases had organisms cultured from the urine that were similar to the organisms cultured from the CSF. This finding had been reported in one study in which 50 % of the cases had similar organisms [6]. In contrary, four out of the non-infected cases had a systemic infection and did not have a positive CSF culture. One can argue that patients with the same organisms cultured from CSF and from elsewhere in the body can be due to under-treatment or simply the antibiotic was not consistent with the sensitivity result. Similarly, those with positive urine culture for instance did not show the organisms in the CSF. The reason we contend is because they were already treated with antibiotic and that may distort the CSF culture result. Unfortunately, the small number of cases threatens the generalizability of our study and further analysis is imperative. Nonetheless, this may advocate for a vigorous treatment of urinary tract infection and infection that has a tendency for septicemia in patients with reservoir.
Furthermore, there a dilemma of temporal association between the presence of the organisms in the urine and in the CSF. The uncertainty can be explained by the fact that the first culture takes several days and we cannot be sure that the urine and the CSF samples were taken on the same day. This applies also to the other studies that reported similar results. The question that arises here is whether systemic infection is a predisposing factor to the development of Ommaya reservoir infection. This warrants further large scale studies to investigate such linkage.
Complications of Ommaya reservoir
In our study, the rate of reservoirs blockage was 6.6 % (n = 3). One of the blocked reservoirs was preceded by a positive CSF culture. The blockage of the reservoir in this particular case may be attributed to infection as argued in another article [12]. However, this was only noted in one of the three cases. The rate of skin dehiscence and CSF leakage was also 6.6 % (n = 3). Skin dehiscence was a predisposing factor in one study [5]. In our study, the infection was not related to skin dehiscence while the number of tapping in relation to infection has not been investigated.
Conclusion
Ommaya reservoir and external ventricular drainage (EVD) both can achieve the goal of diverging CSF in acute hydrocephalus. Our low infection rate is consistent with the literature. Although CSF protein increased by infection, we fail to prove that Ommaya tapping provides a reduction in the CSF protein and hence shunt malfunction thereafter. To conclude, the question that we raise is whether Ommaya reservoir is preferable to EVD. Both EVD and Ommaya reservoir can be used to drain CSF and provide accessibility to CSF for repeated analyses. The Ommaya reservoir infection rate that we found is 6.66 %. The consistency of the low infection rate of Ommaya reservoir between our study and studies from different countries gain the reservoir superiority to EVD, especially when EVDs lack such consistency.
All of the infected Ommaya reservoirs were removed and replaced by an EVD. This clearly outlines the significance of using EVD as a replacement of Ommaya. However, the secondary gain from having the Ommaya reservoirs hidden is its cosmetic effect. This has an impact on the patient’s self-image and would have more parental acceptance. There are psychological and anxiety factors associated with EVDs. Having a tube, the EVD, draining next to the patient creates a context of anxiety. This is seen from the repeated questions raised by the parents in whether the tube is draining, the quantity drained in comparison to yesterday, and the change of its color, all were concerns of patients’ watchers. A superiority of Ommaya to EVD is that a patient with Ommaya can be discharged home and followed up as an outpatient. This is not applicable to patients with EVDs. In deciding between Ommaya and EVDs, we advocate for outweighing the advantages of both in addition to their psychosocial factors.
References
Adegbite AB, Khan M (1982) Role of protein content in CSF ascites following ventriculoperitoneal shunting. Case report. J Neurosurg 57:423–425. doi:10.3171/jns.1982.57.3.0423
Deisenhammer F, Bartos A, Egg R, Gilhus NE, Giovannoni G, Rauer S, Sellebjerg F (2006) EFNS Task Force: guidelines on routine cerebrospinal fluid analysis. Report from an EFNS task force. Eur J Neurol 13:913–922. doi:10.1111/j.1468-1331.2006.01493.x
Dekkers OM, Egger M, Altman DG, Vandenbroucke JP (2012) Distinguishing case series from cohort studies. Ann Intern Med 156:37–40. doi:10.7326/0003-4819-156-1-201201030-00006
Fulkerson DH, Vachhrajani S, Bohnstedt BN, Patel NB, Patel AJ, Fox BD, Jea A, Boaz JC (2011) Analysis of the risk of shunt failure or infection related to cerebrospinal fluid cell count, protein level, and glucose levels in low-birth-weight premature infants with posthemorrhagic hydrocephalus. J Neurosurg Pediatr 7:147–151. doi:10.3171/2010.11.PEDS10244
Jian L, Hang-song S, Zheng-lang L, Li-sheng Y, Heng W, Nu Z (2012) Implantation of Ommaya reservoir in extremely low weight premature infants with posthemorrhagic hydrocephalus: a cautious option. Childs Nerv Syst 28:1687–1691. doi:10.1007/s00381-012-1847-0
Kim JH, Desai NS, Ricci J, Stieg PE, Rosengart AJ, Härtl R, Fraser JF (2012) Factors contributing to ventriculostomy infection. World Neurosurg 77:135–140. doi:10.1016/j.wneu.2011.04.017
Kitchen WJ, Singh N, Hulme S, Galea J, Patel HC, King AT (2011) External ventricular drain infection: improved technique can reduce infection rates. Br J Neurosurg 25:632–635. doi:10.3109/02688697.2011.578770
Lin ZL, Yu B, Liang ZQ, Chen XW, Liu JQ, Chen SQ, Zhang ZY, Zhang N (2009) Role of Ommaya reservoir in the management of neonates with post-hemorrhagic hydrocephalus. Zhonghua Er Ke Za Zhi 47:140–145 (Chinese)
Lin J, Zhou H, Zhang N, Yin B, Sheng HS (2012) Effects of the implantation of Ommaya reservoir in children with tuberculous meningitis hydrocephalus: a preliminary study. Childs Nerv Syst 28:1003–1008
Lwin S, Low SW, Choy DK, Yeo TT, Chou N (2012) External ventricular drain infections: successful implementation of strategies to reduce infection rate. Singapore Med J 53:255–259. doi:10.1007/s00381-012-1748-2
Mead P, Safdieh J, Nizza P, Kiehn T, Tuma S, Sepkowitz K (2010) Ommaya reservoir infections: a 16-year retrospective analysis. Presented at the 4th Annual Meeting of Healthcare and Community-Acquired Infections and Infection Control. Available via IDSA. https://idsa.confex.com/idsa/2010/webprogram/Paper4173.html
Sgouros S, Dipple SJ (2004) An investigation of structural degradation of cerebrospinal fluid shunt valves performed using scanning electron microscopy and energy-dispersive x-ray microanalysis. J Neurosurg 100:534–540
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper. There has been no financial or material support for conducting this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bin Nafisah, S., Ahmad, M. Ommaya reservoir infection rate: a 6-year retrospective cohort study of Ommaya reservoir in pediatrics. Childs Nerv Syst 31, 29–36 (2015). https://doi.org/10.1007/s00381-014-2561-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-014-2561-x