Abstract
Purpose
The aim was to compare the effects of propofol and desflurane anesthesia on transcranial motor evoked potentials (MEPs) from pediatric patients undergoing surgery for spinal deformities.
Methods
Desflurane and propofol cohorts (25 patients each) were obtained retrospectively and matched for patient characteristics and surgical approach. MEPs from the thenar eminence and abductor hallucis were compared during maintenance anesthesia on desflurane (0.6–0.8 MAC) or propofol infusion (150–300 μg/kg/min). MEP amplitudes and durations were obtained for successive 30-min intervals for 150 min, beginning 60 min after maintenance anesthesia.
Results
Mean peak to peak amplitudes of MEPs under desflurane anesthesia from the thenar eminence (419 μV) and abductor hallucis (386 μv) were not significantly different from those under propofol (608 μV, 343 μV, thenar, and abductor hallucis, respectively). Stimulation was greater by 42 V and 136 mA, and trains were slightly longer in the desflurane compared to the propofol group (p < 0.05). Most MEP amplitudes for the desflurane and propofol cohorts remained the same or increased (71 % of cases) when those after 150 min were compared to those in the first 30-min interval.
Conclusions
MEPs with good amplitudes were obtained under desflurane only anesthesia that were comparable to propofol only anesthesia in pediatric patients during surgery for spinal deformities. There was no evidence for anesthetic fade over the time period examined. When used by itself, desflurane can be considered a viable alternative to propofol anesthesia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anesthetic agents with a few exceptions have an adverse effect on electrophysiological signals used for intraoperative monitoring [18, 19]. Somatosensory evoked potentials (SEPs) generated in sensory cortices are reduced in amplitude and show increased latencies in a dose-dependent manner by most inhalational and intravenous agents. SEPs generated in subcortical structures are less affected and may serve as useful alternative recording sites. Motor-evoked potentials (MEPs), which are fast becoming an essential component of intraoperative monitoring [11, 17], are similarly affected by anesthetic agents [4, 13, 14].
As a general rule, SEPs are altered but not abolished by inhalational anesthetic levels up to 1.0 MAC or higher [2, 15, 22]. MEPs on the other hand, may be significantly reduced at anesthetic levels that still support SEPs [1]. Because of this deleterious effect on MEPs by inhalational agents, several studies have advocated the use of intravenous anesthesia involving a propofol/narcotic regimen [5, 12, 13]. MEPs under propofol are similarly reduced in amplitude in a dose-dependent manner but not as severely as with inhalational agents. In general, MEPs with propofol are larger amplitude and more stable than those under inhalational agents.
The benefits of propofol, however, are not without their drawbacks. Propofol has been shown to be potentially toxic [19]. Under normal operating room conditions, this is probably not a pressing issue but is potentially present nevertheless. A more concerning issue is the appropriate level of anesthesia. To date, there are no means to measure the blood levels of propofol to determine effective dosing. Awareness on the one hand and overdosing on the other are real possibilities. Intravenous administration can also be an issue with ruptured veins, blocked or dislodged lines, or human error of operation.
For these reasons, a motor-evoked potential compatible inhalational agent has been sought. Desflurane, one such candidate, has been available for some time. Early studies showed that desflurane has a modest, dose-dependent effect on SEPs, reducing amplitudes and increasing latencies [15, 21]. Studies of desflurane on MEPs, however, are limited. One group has reported MEPs with desflurane that are comparable to propofol [8, 9]. Because of this limited information and especially since there is no data in the pediatric population, this retrospective study of the effect of desflurane on motor-evoked potentials in children was undertaken. Furthermore, in contrast to previously reported data which used desflurane in combination with nitrous oxide, this study compared MEPs under propofol only and desflurane only conditions without background adjunct anesthetic agents.
Methods
This study was a retrospective analysis of motor evoked potential data collected on subjects during the course of standard spinal operations performed at Seattle Children’s Hospital between the years 2008 and 2011. Approval by the institutional review board of Seattle Children’s Hospital was obtained.
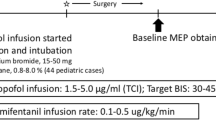
An initial pilot review was done on 14 subjects undergoing spine surgery that received a combination of desflurane (0.25 to 1.0 MAC) and propofol (100–300 μg/kg/min). MEPs could not be obtained from some patients, and amplitudes were reduced in others. Desflurane was then turned off and anesthesia maintained with propofol infusion alone. Significant recovery of amplitudes toward the end of the surgery was observed (Fig. 1). Since it was apparent that this combination of anesthetic agents had an adverse effect on MEPs, the study proceeded to a comparison of each agent in isolation.
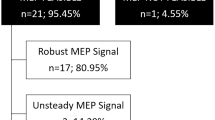
Subsequently, two cohorts of 25 pediatric patients each undergoing surgery for spinal deformities were selected. The desflurane group consisted of 25 consecutive cases which were then matched to a propofol group for age, gender, and type of surgical procedure as summarized in Table 1. Patients with absent MEP baselines and with MEP alerts during the surgery were excluded from the analysis. These exclusion criteria were obtained from our intraoperative neuromonitoring database. Otherwise, matching was blinded to the MEP monitoring during the case.
Both groups were induced either with an inhalational agent (sevoflurane or desflurane) plus a propofol bolus (30–300 mg) or with a propofol bolus alone. In the desflurane group, 20 patients were induced with a combination of inhalational agent (sevoflurane or desflurane), propofol bolus and narcotic, and 5 with propofol bolus only. In the propofol group, 17 patients were induced with a combination of inhalational agent (sevoflurane or desflurane), propofol bolus and narcotic and 8 with propofol bolus only. For analgesia, both groups were induced with narcotic boluses (fentanyl) and maintained on a narcotic infusion (remifentanil). No neuromuscular blockade was used in order to optimize motor responses. After induction, the inducing anesthetic agents were discontinued and maintenance anesthetic agent administered. A desflurane group of 25 patients was maintained on desflurane (0.6–0.8 MAC) for the remainder of the procedure. A propofol group of 25 patients received a propofol infusion (150–300 μg/kg/min).
As part of our standard monitoring protocol for spine cases, all patients were monitored with MEPs, SEPs, and free running electromyography (EMG). Cadwell Cascade equipment was used throughout. MEPs were stimulated with a train of 0.05 ms duration pulses delivered transcranially between leads placed at C3 and C4 (standard international 10–20 system). The anode at C3 or C4 was contralateral to the stimulated extremities. Train length and stimulus intensity was adjusted to provide stable MEPs that were clearly above threshold but below supramaximal response.
MEPs were typically recorded from the thenar eminence of each hand, the iliopsoas, vastus medialis, extensor hallucis longus and abductor hallucis of each lower extremity, and the anal sphincter. In the extremities, needle electrodes were placed over the belly of each muscle about 2 cm apart. In this paper, we report amplitudes and durations of MEPs from the thenar eminence and abductor hallucis. Amplitudes of the response were measured as maximal peak to peak amplitude. All measurements were from the same side for each patient. Response duration was measured as the time from the initial deflection to the return of the trace to baseline zero voltage. Turns or number of peaks were not noted.
MEP mean data for the desflurane and propofol groups was obtained over a 150-min period, beginning at 60 min after induction. The number of observations per patient varied from 5 to 15 with the majority more than 10. Because MEPs were not taken at set times during the procedures, the MEP data were binned in 30-min increments starting at 60 min after the induction of anesthesia. If multiple values occurred within any 30-min bin, an average was taken to form the representative value for that bin. Anesthetic fade was examined as the relative number of cases showing an amplitude decrease ≥10 % compared to those with no change or an increase in amplitude. The percent change in each 30-min bin for each patient was obtained relative to the first available MEP data, beginning a minimum of 60 min after induction. The coefficient of variation (standard deviation/mean) was calculated for all values taken regardless of time after induction. t tests were used to test for significant mean differences between the desflurane and propofol groups. A Bonferroni correction was used for these multiple mean comparisons.
Results
Suprathreshold MEP responses with good amplitudes were obtained from both the desflurane and propofol groups (Table 2). Thenar MEPs had mean peak to peak amplitudes of 419 μV (range 69–1,114 μV) with desflurane and 608 μV (range 22–1,928 μV) with propofol. Abductor hallucis MEPs had mean amplitudes of 386 μV (range 74–1,099 μV) with desflurane and 343 μV (68–1,320 μV) with propofol. Although mean amplitudes were not significantly different between the desflurane and propofol groups, their large variability and the small number of patients in each group made mean comparisons underpowered for detecting modest amplitude differences (Fig. 2).
The durations of thenar MEPs were also similar between the two groups, averaging 22.9 ms (range 11.5–35.9 ms) and 22.5 ms (range 12.7–36.6 ms) for desflurane and propofol, respectively. In contrast, the abductor hallucis mean duration of 33.5 ms (range 20.6–46.1 ms) under desflurane was significantly greater than that seen under propofol anesthesia (24.9 ms, range 13.8–43.4 ms, p < 0.0005).
Greater voltage and current with longer trains were required for suprathreshold MEP responses in the desflurane as compared to the propofol group (Table 2). Stimulus voltage averaged 339 V for the desflurane group and 297 V for the propofol group. Measured current was 798 and 662 mA, respectively. Mean train length was 7.9 for the desflurane group and 6.5 for the propofol group. All of these mean differences were statistically significant at p < 0.003 or better, and the total familywise error including all mean comparisons was p < 0.05. In summary, stimulation was greater by 42 V (16–68, 95 % CI) and 136 mA (40.8–230.9, 95 % CI), and trains were slightly longer by 1.3 pulses (0.6–2.1, 95 % CI) in the desflurane compared to the propofol group (Fig. 2).
Time dependency
Anesthetic fade with desflurane or propofol anesthesia was examined for 150 min beginning 60 min after induction. For each patient, percent changes in MEP amplitudes were calculated relative to the first period a MEP was obtained (Fig. 3). MEPs were not available for all 30-min bins in many cases, resulting in bin counts less than 25. With the exception of thenar MEP amplitudes at 60 min under desflurane and propofol, the number of cases with decreased amplitudes in each bin was less than those with no change or increased amplitudes. There was no trend for amplitudes to decrease with time, which would be seen as an increasing relative size of the black segments with each successive 30-min bin. For those cases where MEPs were obtained 150 min after the first, amplitudes under desflurane and propofol were more likely to remain the same or increase (71 % of cases) than decrease (29 %).
MEP amplitudes from the thenar eminence and abductor hallucis (AH) were obtained for successive 30-min time periods beginning at least 60-min post-induction. Times after the first MEP for the desflurane and propofol groups are shown. Segment heights within each bar show the number of patients with decreased (black) or no change/increased amplitudes (white). MEPs were not available for every 30-min epoch, as shown in the unequal number of cases for each epoch
The coefficient of variation, which measured the variability of responses across time, also was similar for both groups. Thenar MEPs showed coefficients of variation of 0.75 and 0.66 for desflurane and propofol, respectively, and for abductor hallucis, coefficients of variation were 0.50 and 0.60. For desflurane, the change in voltage from baseline to final runs averaged to a decrease of 1 % with 16 of 25 changing less than 10 %. If anything, for propofol, there was a slight increase in voltage from baseline to final runs, with the average an increase of 19 %, but 13 of 25 changing less than 10 %.
Discussion
These findings are a modest comparison of the effects of desflurane and propofol anesthesia on MEPs in the pediatric population and to our knowledge is the first to be reported. The results of an initial pilot study suggested that desflurane in combination with propofol at substantial dosages for both severely reduced or abolished the amplitudes of MEPs recorded at the upper and lower extremities. The present study compared MEPs in two matched cohorts. Desflurane used alone without propofol was compared to propofol alone without desflurane.
Many studies have identified problems when volatile anesthetics are used with MEPs. Volatile anesthetics, either alone [16] or in combination with nitrous oxide [3, 14] decrease the likelihood of obtaining MEP baseline responses. They may also increase the probability of false positives [16, 20], due to the relatively small amplitudes under volatile anesthesia as compared to propofol alone.
MEP amplitudes averaged several hundred microvolts in both the propofol and desflurane groups. Although not significant, modest differences in amplitudes between the groups would have been difficult to detect with the size of the cohorts in this study. MEP response durations, which reflect one aspect of their complexity, for the hands were also similar under desflurane and propofol, but were significantly longer for the abductor hallucis under desflurane anesthesia. Comparable amplitudes and variability, as shown by the coefficients of variation, demonstrate that MEPs under desflurane have a satisfactory signal to noise, and may be used without increasing the risk of false positive or unobtainable responses.
The results of this study are consistent with previous studies showing the relative equivalence of desflurane and propofol [8, 9]. One difference in this study was the use of desflurane or propofol as the sole anesthetic agent without an adjunct anesthetic such as nitrous oxide. This difference in anesthetic, and different MEP stimulation techniques, may explain the generally greater amplitudes observed for the abductor halluces responses in our study as compared to these other studies. In these previous studies, constant current stimulation was used, and amplitudes were adjusted to 10 % above threshold responses. In this study, stimulation intensity was increased until suprathreshold responses of typically several hundred microvolts were obtained. Another difference between this and previous studies was the focus on children and, thus, expanding the beneficial findings of desflurane to that group of patients.
The concept of anesthetic fade of MEPs over time has been reported for desflurane in combination with nitrous oxide or propofol [10]. That study measured anesthetic fade as the increase in threshold for MEPs over the course of surgery. MEP amplitudes were examined over a shorter time period (150 min) in the present study. No trend of decreased amplitudes with time was observed. For most subjects, stimulus voltages were held to less than 10 % increase or decrease. Liu et al. [7] found no changes in MEP amplitudes over 120 min in patients undergoing spine surgery with propofol anesthesia.
The patients in the present study were induced on combinations of inhalational agents and propofol and then converted to desflurane or propofol. The time until data collection started (60 min after conversion) may not have been sufficient for complete washout of the induction agent, and increased amplitudes over time are possible. Even so, the lack of any fade may relate to the use of only the one anesthetic agent without any adjunct agents. It is also possible that fade would have been observed at times longer than the 150 min used in the present study.
A strength of this study is the matching of cohorts which was blinded to the neuromonitoring data to reduce the risk of confounding variables and bias. The relatively few exclusion criteria increase the external validity of this study, where results may be generalized to surgeries where variables (e.g., mean arterial pressures) in some cases may, unavoidably, be poorly controlled. Pediatric patients undergoing surgery for spinal deformities were used in this study, and results may not extend to those with significant myelopathy or morbidity.
The limitations of this study are its sample size, its retrospective approach, and the use of different agents for induction. The small sample size is mitigated by the use of matched subjects to minimize between group subject variability. For example, the ages ranged from 2 to 17 years of age, which may have introduced age-related effects on our findings [6]. However, the use of age matched cohorts should have minimized this potential confounding variable. The disadvantage of a retrospective approach was that it did not allow for control of variables such as the type and dosage of induction agents, and changes over time in anesthetic or neuromonitoring technique. While the induction regimens were not uniform throughout, there was no consistent difference between the two groups, so any variability should have been evenly applied.
In summary, MEPs showed good quality amplitudes under desflurane only anesthesia that were comparable to propofol only anesthesia. The combination of the two anesthetics had a deleterious effect on MEP amplitudes, rendering them nearly unusable. When used by itself, desflurane can be considered a viable alternative to propofol anesthesia.
References
Chen Z (2004) The effects of isoflurane and propofol on intraoperative neurophysiological monitoring during spinal surgery. J Clin Monit Comput 18:303–308
Clapcich AJ, Emerson RG, Roye DP et al (2004) The effects of propofol, small-dose isoflurane, and nitrous oxide on cortical somatosensory evoked potential and bispectral index monitoring in adolescents undergoing spinal fusion. Anesth Analg 99:1334–1340
Deiner SG, Kwatra SG, Lin H, Weisz DJ (2010) Patient characteristics and anesthetic technique are additive but not synergistic predictors of successful motor evoked potential monitoring. Anesth Analg 111:421–426
Jellinek D, Platt M, Jewkes D, Symon L (1991) Effects of nitrous oxide on motor evoked potentials recorded from skeletal muscle in patients under total anesthesia with intravenously administered propofol. Neurosurgery 29:558–562
Kunisawa T, Nagata O, Nomura M, Iwasaki H, Ozaki M (2004) A comparison of the absolute amplitude of motor evoked potentials among groups of patients with various concentrations of nitrous oxide. J Anesth 18:181–184
Lieberman JA, Lyon R, Feiner J, Diab M, Gregory GA (2006) The effect of age on motor evoked potentials in children under propofol/isoflurane anesthesia. Anesth Analg 103:316–321
Liu HY, Zeng HY, Cheng H, Wang MR, Qiao H, Han RQ (2012) Comparison of the effects of etomidate and propofol combined with remifentanil and guided by comparable BIS on transcranial electrical motor-evoked potentials during spinal surgery. J Neurosurg Anesthesiol 24:133–138
Lo YL, Dan YF, Tan YE, Nurjannah S, Tan SB, Tan CT, Raman S (2004) Intra-operative monitoring in scoliosis surgery with multi-pulse cortical stimuli and desflurane anesthesia. Spinal Cord 42:342–345
Lo YL, Dan YF, Tan YE, Nurjannah S, Tan SB, Tan CT, Raman S (2006) Intraoperative motor-evoked potential monitoring in scoliosis surgery: comparison of desflurane/nitrous oxide with propofol total intravenous anesthetic regimens. J Neurosurg Anesthesiol 18:211–214
Lyon R, Feiner J, Lieberman JA (2005) Progressive suppression of motor evoked potentials during general anesthesia: the phenomenon of "anesthetic fade". J Neurosurg Anesthesiol 17:13–19
Macdonald DB, Skinner S, Shils J, Yingling C (2013) Intraoperative motor evoked potential monitoring—a position statement by the American Society of Neurophysiological Monitoring. Clin Neurophysiol 124:2291–2316
Nathan N, Tabaraud F, Lacroix F, Mouliès D, Viviand X, Lansade A, Terrier G, Feiss P (2003) Influence of propofol concentrations on multipulse transcranial motor evoked potentials. Br J Anaesth 91:493–497
Pechstein U, Cedzich C, Nadstawek J, Schramm J (1996) Transcranial high-frequency repetitive electrical stimulation for recording myogenic motor evoked potentials with the patient under general anesthesia. Neurosurgery 39:335–344
Pelosi L, Stevenson M, Hobbs GJ, Jardine A, Webb JK (2001) Intraoperative motor evoked potentials to transcranial electrical stimulation during two anaesthetic regimens. Clin Neurophysiol 112:1076–1087
Schindler E, Müller M, Zickmann B, Osmer C, Wozniak G, Hempelmann G (1998) Modulation of somatosensory evoked potentials under various concentrations of desflurane with and without nitrous oxide. J Neurosurg Anesthesiol 10:218–223
Shida Y, Shida C, Hiratsuka N, Kaji K, Ogata J (2012) High-frequency stimulation restored motor-evoked potentials to the baseline level in the upper extremities but not in the lower extremities under sevoflurane anesthesia in spine surgery. J Neurosurg Anesthesiol 24:113–120
Sloan TB, Janik D, Jameson L (2008) Multimodality monitoring of the central nervous system using motor-evoked potentials. Curr Opin Anaesthesiol 21:560–564
Sloan TB, Heyer EJ (2002) Anesthesia for intraoperative neurophysiologic monitoring of the spinal cord. J Clin Neurophysiol 19:430–443
Sloan T (2010) Anesthesia and intraoperative neurophysiological monitoring in children. Childs Nerv Syst 26:227–235
Tamkus AA, Rice K, Kim HL (2014) Differential rates of false-positive findings in transcranial electric motor evoked potential monitoring when using inhalational anesthesia versus total intravenous anesthesia during spine surgeries. Spine J. doi:10.1016/j.spinee.2013.08.037
Vaughan DJA (2001) Effects of different concentrations of sevoflurane and desflurane on subcortical somatosensory evoked responses in anaesthetized, non-stimulated patients. Br J Anaesth 86:59–62
Zhang JLW (2005) Effects of volatile anesthetics on cortical somatosensory evoked potential and bispectral index. Chung-Hua I Hsueh Tsa Chih 85:2700–2703
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Holdefer, R.N., Anderson, C., Furman, M. et al. A comparison of the effects of desflurane versus propofol on transcranial motor-evoked potentials in pediatric patients. Childs Nerv Syst 30, 2103–2108 (2014). https://doi.org/10.1007/s00381-014-2510-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-014-2510-8