Abstract
Introduction
Metopic suture synostosis leading to trigonocephaly is considered the second most frequent type of craniosynostosis. Besides esthetic results, we present 25 consecutive pediatric cases operated upon metopic suture synostosis with a focus on the child’s motor, speech, and neurocognitive development.
Methods
Twenty-five children (aged 6 to 33 months; median 9.2 months) with trigonocephaly were operated upon between 2002 and 2012 with fronto-orbital advancement including frontal bone cranioplasty and fronto-orbital bandeau remodeling. Neurodevelopmental deficits were evaluated by a standardized questionnaire including gross motor function, manual coordination, speech, and cognitive function performed by independent pediatric/developmental neurologists before surgery and at 6 and 12 months of time interval postoperatively.
Results
Twenty-one (84 %) boys and four (16 %) girls were included in this study. Mean follow-up period was 33 ± 28 months. Outcome analysis for esthetic results showed a high degree of satisfaction by the parents and treating physicians in 23 cases (92 %). Preoperative evaluation revealed neurodevelopmental deficits in 10 children (40 %; six mild, four moderate degree). Twelve children (48 %) were proven to have a normal preoperative neuropediatric development. Mild or moderate developmental restraints were no longer apparent in 6/13, improved but still apparent in 3/13, and stable in 4/13, 6 months after cranial vault reconstruction. At 12 months of follow-up, deficits were no longer present in 9/13 and improved in 4/13. Apart from this cohort, two children were diagnosed with a syndromic form, and one child had a fetal valproate syndrome. In these three children, neurodevelopmental deficits were more pronounced. Neurocognitive progress was obvious, but was comparably slower, and major deficits were still apparent at last follow-up. All children with proven mild/moderate/severe deficits received intensive physiotherapy, logopedic, or neurobehavioral support.
Conclusions
As shown in a single-center observation, surgical correction of metopic suture synostosis not only refines esthetic appearance but also might improve neurodevelopmental outcome if deficits are apparent, even in syndromic forms of the deformity under additional physiotherapy, logopedic, or neurobehavioral support.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The patency of open cranial sutures allows the skull to mold during delivery and enables the developing brain to expand and to grow. Premature closure of the cranial sutures is called craniostenosis and provokes characteristic skull deformities depending on the suture involved. A premature closure of the metopic suture between both frontal bones consequently leads to trigonocephaly with narrowing of the orbits and the forehead. Apart from the esthetic aspect with shallow temples and hypotelorism, impaired skull growth in the frontal region can lead to increased intracranial pressure and thereby impaired normal development. The main purpose of craniostenosis repair is to prevent developmental delay and severe deformities in an esthetic relevant area.
The range of incidence of metopic synostosis has been reported to be rather wide with an increasing rate over the recent decades to 25.5 % [1]. Kweldam et al. reported on a current incidence of 1:5,200 newborns [2].
Metopic suture synostosis leading to trigonocephaly was considered the third most frequent single-suture craniostenosis/-synostosis after scaphocephaly and plagiocephaly. However, according to increasing incidence over the last few decades, trigonocephaly is now the second most frequently seen type of craniosynostosis [1, 3–5]. The normal growth in the sutures is perpendicular to the orientation of the suture. A premature closure of a single suture is accompanied by compensatory growth in other sutures and by appositional growth in other parts of the skull [6, 7]. In trigonocephaly, the skull becomes prominent in the parieto-occipital region, while it remains very short and narrow in the forehead with ridging of the metopic suture. In addition, development of the midface is impaired with narrow orbits and a small midface. Apart from the esthetic aspects of a metopic synostosis, normal intellectual development of a child depends significantly on the ability of the growing brain to expand. Pressure on the developing cerebral cortex may have a detrimental effect on the child’s intelligence, although unequivocally raised intracranial pressure is found only in about 50 % of the patients, even with multiple suture fusions [8].
We present the clinical and esthetic results in 25 consecutive pediatric cases operated upon metopic suture synostosis at the Pediatric Neurosurgical Unit of the Ludwig-Maximilians-University, Munich, with special focus on the child’s neurocognitive, motor, and speech development.
Material and methods
Patient selection
All pediatric patients presenting with the clinical and radiological signs for a premature closure of the metopic suture and who had craniostenosis repair between August 2002 and May 2012 were included in the present study. Informed consent about the developmental evaluation was obtained for all patients.
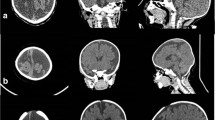
The typical clinical appearance included a narrow forehead with ridging of the metopic suture, hypotelorism, fleeing eyebrow region, and shallow temples. This was confirmed on a low-dose spiral CT scan with 3D reconstruction or more recently on MR reconstructions. Fundoscopy was performed routinely to rule out increased intracranial pressure. In addition, patients underwent thorough neurodevelopmental exams by pediatricians or pediatric neurologists and, in suspected cases, a genetic work-up for a syndromic form of trigonocephaly.
The surgical correction of this complex three-dimensional growth restriction caused by metopic synostosis was performed by a team consisting of a pediatric neurosurgeon (AP, MK, LA), pediatric surgeon (ML, AH), and a cranio-maxillo-facial surgeon (GM). The operative techniques as well as the postoperative clinical course and complications are described.
Patient evaluation
Clinical and esthetic follow-up examination was performed 3, 6, and 12 months after surgery, followed by yearly intervals up to 5 years. Date of last follow-up was October 2012. Apart from standard measurements of the skull circumference, esthetic results were evaluated by AP, GM, MK, and ML within the follow-up period to determine whether the metopic ridging and width of the forehead were satisfactorily corrected. Esthetic results have been photo documented by AP, GM, and ML from three different positions (anterior, lateral, and superior view) and compared to the preoperative shape and extension of the forehead. In addition, at the time of follow-up investigations, parents were interviewed about their subjective satisfaction with esthetic results as well as the postoperative developmental achievements of their children.
Due to the fact that the neurodevelopmental assessment of children at the age of 12 months or younger is difficult, a standardized questionnaire including gross motor function (e.g., trunk control, head elevation, standing, walking), manual coordination (grasping), speech (e.g., intentional crying, vocalization), and cognitive function (e.g., observation, hand–mouth–eyes exploration) was applied and conducted by independent pediatric/developmental neurologists before surgery and at 6 and 12 months of time intervals postoperatively [9, 10]. Neuropediatric development was evaluated according to the achievement of motor, speech, and cognitive milestones that have been reached/not reached at the corresponding age. The applied standardized questionnaire is shown in Table 1.
Preoperative developmental deficits were regarded as mild, moderate, or severe, if the corresponding motor, speech, and cognitive milestones achieved by each child was comparable/equivalent to children of 3 (mild), 6 (moderate), or more than 6 (severe) months younger in age. At time intervals of 6 and 12 months postoperatively, any functionally relevant changes in neurological development as compared to the preoperative status was classified as improvement if deficits changed from mild to no longer apparent (n.a.), from moderate to mild/n.a., and from severe to moderate/mild/n.a., or as deterioration in case of worsening or new appearance of deficits. In all other cases, the postoperative status was evaluated to be stable.
Results
Between 2002 and 2012, 25 consecutive cases of trigonocephaly were treated with fronto-orbital advancement including frontal bone cranioplasty and fronto-orbital bandeau remodeling. There were 21 (84 %) boys and four (16 %) girls. Median age at the time of surgery was 9.2 months (range, 6–33 months). Mean follow-up period was 33 ± 28 months. Two children (8 %) were diagnosed later on with a syndromic form of metopic suture synostosis. In one syndromic child, a mutation in the TWIST1 gene could be identified. Despite intensive investigation, a definitive mutation in the other syndromic child could not be detected, but clinically, a syndrome had to be suspected due to severe retardation and typical stigmata such as low ear position, auricle abnormalities, and syndactyly.
On preoperative work-up, fundoscopy was normal in all patients. Preoperative CT or MR images showed premature fusion solely of the metopic suture even in the syndromic cases.
Surgical procedure is to some extent standardized, and we mention in the following only surgical aspects that have been modified at our institution.
After careful positioning and limited hair shaving, a bicoronal skin incision was tailored in multiple soft curves for optimal esthetic results. Using a monopolar needle, the layer between galea and periosteum was dissected down towards the supraorbital bar with preservation of the supraorbital nerve. Bifrontal craniotomy was performed, and the supraorbital bandeau was released with an oscillating mini-saw, remodeled by an open wedge osteotomy, internally fixed with absorbable plates and screws. To smoothen the bony edges and to improve the contour of the temples, the periosteum and the temporal muscles were reattached to the bandeau. The bifrontal bone flap was rotated and incised in order to model a symmetrical and anatomical well-contoured forehead. Fixation was accomplished with absorbable plates and screws as well as sutures. At the level of the bandeau, the plates and screws were placed on the inner side to prevent visible degradation reactions in the facial area.
Perioperative complications
Although the surgical procedure was performed at a young age with a mean body weight of 8.8 ± 1.1 kg, patients tolerated surgery very well, and there was no 30-day morbidity. Due to the large area of exposed, well vascularized dura and bone (still participating in hematopoesis), the limited blood volume at this age and the length of the procedure of 3 to 4 h, the mean blood loss was 291 ± 137 ml [21–49 % of circulating blood volume]. Blood transfusion (a mean of 177 ± 126 ml) was necessary in all but two children, both of which were older than 1 year. Prophylactic antibiotics (third-generation cephalosporin) were given for the first 5 days. All children developed periocular swelling to a varying degree that resolved completely during the hospital stay. Mean hospital stay was 7 days.
Esthetic results
Esthetic results showed a high degree of parents’ satisfaction in 23 cases (92 %) at follow-up investigations. The parents of one boy had very high expectations and were not completely happy because they assumed the forehead still is too narrow despite his perfect developmental progress. Another patient had, in addition to his trigonocephaly, a positional plagiocephaly, and this was most likely the reason why the parents of this child were not absolutely satisfied despite the perfect shape of the forehead also on MR scans. Esthetic results have been photo documented by AP, GM, and ML from three different positions (anterior, lateral, superior view) and compared to the preoperative shape and extension of the forehead.
No reoperation due to recurrent skull deformity of the forehead or temporal hollowing was necessary in any of the cases.
In three children, a transient swelling around the absorbable plates and screws was observed around 12 to 18 months after surgery. No revision was necessary, and the granulomatous reaction disappeared within the subsequent 6 months.
Neuropediatric development
Twelve children (48 %) were found to have a normal preoperative neurological development. In 10 children (40 %) standardized neuropediatric evaluation revealed neurodevelopmental deficit of a mild (n = 6) and moderate (n = 4) degree (Table 2). Deficits consisted of a mild or moderate impairment with regard to crawling or sitting due to hypotony/low tone of trunk muscles or deficits in manual coordination in six and two children, respectively; an additional delay in speech development in two and in cognitive development in one of these children. Two children presented with deficits in speech development in a mild and moderate degree in one child each without any other limitations.
Three children (12 %) showed more pronounced developmental delay with lack of head control, delayed motor function of the hands, and with additional restraints in speech and cognition. Two of the latter group had a syndromic form, and the other child had a known fetal valproate syndrome.
During the postoperative course, the 12 unaffected children continued to develop within the normal time and achieved all developmental milestones (Table 2). Children with a mild form of delay in motor function (n = 6) caught up with those of the same age under intensive physiotherapy in four cases and persisted in two cases at 6 months of follow-up. However, the respective delay was no longer apparent in all patients at 12 months of follow-up. Moderate delay in motor function was obvious in two children. At 6 months of follow-up, deficits improved to a mild degree in one child and moderately persisted in the other. At 12 months of follow-up, both children had improved with physiotherapy, but still exhibited a mild degree of motor delay. In eight children with proven mild and moderate delay in motor development, deficits were no longer apparent in four, improved, but were still apparent in one and were unchanged in three children at 6 months of follow-up. At 12 months of follow-up, motor deficits were no longer detectable in six and improved, but were still apparent in two children. Children with preoperative delay in speech development (n = 4), moderate deficits improved to a mild but still apparent deficit at 6 and 12 months of follow-up in one child, and mild deficits (n = 3) were no longer apparent in two cases at 6 months of follow-up and in all three cases at 12 months of follow-up. All of these children received logopedic therapy. Cognitive delay was evident to a moderate degree in one child and showed steady improvement under behavioral therapy at 6 and 12 months of follow-up.
Mild or moderate developmental restraints were no longer apparent in 6/13, improved, but were still apparent in 3/13 and were stable in 4/13 6 months after cranial vault reconstruction. At 12 months of follow-up, deficits were no longer apparent in 9/13 and improved, but were still apparent in 4/13 (Table 2).
The two syndromic children and the child with fetal valproate syndrome also improved with regard to their preexisting severe motor, speech, and cognitive deficits under intensive physiotherapy, logopedic, and neurobehavioral support, but neurocognitive progress was considerably slower. At 6 months of follow-up, severe deficits (n = 8) improved in only half of the deficits; at 12 months of follow-up, an improvement was obvious in six deficits, but were still apparent in a moderate degree.
In the patient cohort, no deterioration or appearance of new neurodevelopmental deficits occurred at 6 and 12 months of follow-up.
Discussion
Due to the increased incidence over the last few decades, metopic synostosis (trigonocephaly) has been shown to be the second most frequently seen type of craniosynostosis [1, 3–5].
Whether the marked increase in occurrence of trigonocephaly stated by several authors is due to a higher awareness of this disease among the medical community and public, due to improved diagnostic techniques or due to genetic or environmental or even mechanical or pharmacological factors, is still not resolved [12]. As was seen in our series, a male predominance in trigonocephaly is generally observed.
In the present study, esthetic results were very satisfactory in almost all children of our cohort evaluated by the parents and treating physicians at 3, 6, and 12 months of follow-up investigations and up to the age of 5 years. However, this evaluation may be biased from both sides and prospective three-dimensional digital measurement of the forehead pre- and postoperatively will be performed in the future.
Furthermore, no complications have been observed despite the extent of surgery in this very young age group with a relatively high rate of blood loss observed (mean blood loss 291 ± 137 ml; 21–49 % of circulating blood volume). Blood transfusion became necessary in all but two children. These results are in accordance to the literature with a median average amount of blood loss of less than 255 ml, ranging from 80 to 600 ml and blood transfusion in all cases [13].
No reoperations due to forehead deformities or temporal hollowing were necessary in all cases during follow-up. Reported complications in the literature are infection, hematoma, seroma, cerebrospinal fluid leakage, and recurrent bitemporal narrowing requiring repeated surgical interventions. In the series of Hormozi et al., eight revisions in 60 patients after trigonocephaly repair were reported [14]. In the literature, a reoperation rate of up to 15 % due to temporal hollowing is not unusual [15, 16].
While some authors report on mental impairment in children with craniostenosis [17], there is growing evidence that single-suture craniostenosis do affect normal neurological development [18–23]. Neurodevelopmental delays in metopic synostosis are reported in the literature ranging from 15 % to as high as 61 % [1, 24–26]. In comparison to sagittal suture stenosis, neurobehavioral studies on children affected by metopic synostosis are far less common and less precise. There is some evidence of learning and/or behavioral deficits. Shimoji et al. [27, 28] theorized that even mild forms of metopic ridging can be associated with significant developmental delay, language problems, and hyperactivity. Mendonca and coworkers reported about 6 out of 20 patients undergoing frontal orbital advancement and remodeling exhibit speech and language problems with no consistent trend observed linking the severity of frontal stenosis using the measured parameters with speech and language delays [11]. In a recent study, Da Costa and coworkers evaluated the neurodevelopmental functioning of infants with untreated single-suture craniosynostosis during early infancy [26]. They assumed that abnormal sutural fusion during the gestational and perinatal phase could compromise brain development and concomitant cognitive development. Boterro et al. evaluated 76 children with metopic synostosis: 32 % of the operated children showed developmental delay, while the incidence in nonoperated children with mostly milder forms of trigonocephaly was 23 % [18]. Their results support the theory that the developmental delay in metopic synostosis primarily derives from the brain and might not be a direct result of the craniosynostosis acting as a growth restrictor. The positive development in children treated for trigonocephaly at our institution reported by their parents was the reason to perform this study and to include the neurodevelopmental progress apart from the esthetic results. Despite parents even reporting a slight acceleration in the development of their children within the first weeks after operation, we had to face the problem that neurodevelopmental progress after surgery reported by the parents is not objective. Due to the fact that neurodevelopmental assessment and quantification of deficits in children at the age of 12 months or younger is difficult, a standardized questionnaire including gross motor function, manual coordination, speech, and cognitive development was applied (Table 1) [9, 10] and conducted by independent pediatric/developmental neurologists before surgery and at 6 and 12 months of time interval postoperatively. The intention of the present study was to analyze the early effects of metopic suture stenosis repair on the achievement of developmental milestones.
In the current study, 52 % of the children showed neurodevelopmental deficits: 40 % of the children exhibited a moderate (i.e., corresponding milestones achieved comparable to children of 6 months younger in age) or mild (comparable to children of 3 months younger in age) delay in mainly motor function (n = 8), but also in speech development (n = 4) and rarely in cognitive function (n = 1). Apart from this cohort, three children (12 %) suffered from a severe (comparable to children of >6 months younger in age) degree of neurodevelopmental delay. Of these, two children were syndromic, and one child was known to suffer from fetal valproate syndrome. The authors admit that these three children compose a completely different cohort and are not comparable to the other ten children due to other underlying causes.
Despite the fact that these children underwent a major surgical procedure at a very young age, an improvement was observed to some degree even at 6 months of follow-up. But at 12 months of follow-up, motor deficits were no longer apparent in 75 % and improved, but were still present in 25 %. Comparable results after 12 months were observed in children with deficits in speech development. Even in severe neurodevelopmental deficits in two syndromic children and in one child with fetal valproate syndrome, an improvement to a moderate degree could be achieved in half of the deficits at 6 months of follow-up. However, improvement was comparably slower despite intensive supportive therapy, but nevertheless promising results could be observed at 12 months of follow-up with an amelioration of initially severe to moderate deficits. Requirements for this relatively high improvement rate in all children were constant and intensive physiotherapy, logopedic, and neurobehavioral training irrespective of the degree of deficits. One major limitation in the present study is the relatively small number of patients treated at a single institution over a 10-year period. Furthermore, we have to admit that our series did not include children with mild forms of trigonocephaly and possible neurodevelopmental deficits that were surveyed without fronto-orbital advancement. In these cases, children might have improved under intensive training, too. Nevertheless, improvement rates at 6 months after cranial vault remodeling imply some evidence that these effects are somehow related to the decompression of the brain and not solely attributable to the natural course of child’s development under intensified physiotherapy and logopedic therapy. Among the pediatric subspecialties dealing with children suffering from craniostenosis, there is a growing awareness that standardized parameters of care for craniostenosis patients and their caregivers as well as the medical community are necessary. In this respect, Warren and coworkers have recently published a reasonable reporting system [29]. The individual number of cases treated per year even in a very active pediatric neurosurgical unit is limited due to the low incidence of this deformity. It would be therefore desirable to include all patients within a national or even international registry applying general preoperative parameters as well as postoperative outcome scales evaluating both esthetic results by three-dimensional digital measurements of the forehead and standardized neurodevelopmental status and progress in a prospective fashion.
References
van der Meulen J (2012) Metopic synostosis. Child’s Nerv Syst: ChNS 28:1359–1367, Official Journal of the International Society for Pediatric Neurosurgery
Kweldam CF, van der Vlugt JJ, van der Meulen JJ (2011) The incidence of craniosynostosis in the Netherlands, 1997–2007. J Plast Reconstr Aesthet Surg: JPRAS 64:583–588
Di Rocco F, Arnaud E, Meyer P, Sainte-Rose C, Renier D (2009) Focus session on the changing “epidemiology” of craniosynostosis (comparing two quinquennia: 1985–1989 and 2003–2007) and its impact on the daily clinical practice: a review from Necker Enfants Malades. Child’s Nerv Syst: ChNS 25:807–811, Official Journal of the International Society for Pediatric Neurosurgery
Di Rocco F, Arnaud E, Renier D (2009) Evolution in the frequency of nonsyndromic craniosynostosis. J Neurosurg Pediatr 4:21–25
van der Meulen J, van der Hulst R, van Adrichem L, Arnaud E, Chin-Shong D, Duncan C, Habets E, Hinojosa J, Mathijssen I, May P, Morritt D, Nishikawa H, Noons P, Richardson D, Wall S, van der Vlugt J, Renier D (2009) The increase of metopic synostosis: a pan-European observation. J Craniofac Surg 20:283–286
Bradley JP, Levine JP, Blewett C, Krummel T, McCarthy JG, Longaker MT (1996) Studies in cranial suture biology: in vitro cranial suture fusion. Cleft Palate-Craniofac J 33:150–156, Official Publication of the American Cleft Palate-Craniofacial Association
Bradley JP, Levine JP, Roth DA, McCarthy JG, Longaker MT (1996) Studies in cranial suture biology: IV. Temporal sequence of posterior frontal cranial suture fusion in the mouse. Plast Reconstr Surg 98:1039–1045
Tamburrini G, Caldarelli M, Massimi L, Santini P, Di Rocco C (2005) Intracranial pressure monitoring in children with single suture and complex craniosynostosis: a review. Child’s Nerv Syst: ChNS 21:913–921, Official Journal of the International Society for Pediatric Neurosurgery
Michaelis R, Niemann G (1999) Das Prinzip der essentiellen Grenzsteine. In: Niemann G, Krägeloh-Mann I, Mayerhofer-Kahle H (eds) Entwicklungsneurologie und Pädiatrie. Hippokrates, Stuttgart, pp 62–74
Michaelis Richard NG (2010) Entwicklungsneurologie und Neuropädiatrie: Grundlagen und diagnostische Strategien. Thieme, Stuttgart
Mendonca DA, White N, West E, Dover S, Solanki G, Nishikawa H (2009) Is there a relationship between the severity of metopic synostosis and speech and language impairments? J Craniofac Surg 20:85–88, discussion 89
Kolar JC (2011) An epidemiological study of nonsyndromal craniosynostoses. J Craniofac Surg 22:47–49
Engel M, Thiele OC, Muhling J, Hoffmann J, Freier K, Castrillon-Oberndorfer G, Seeberger R (2012) Trigonocephaly: results after surgical correction of nonsyndromatic isolated metopic suture synostosis in 54 cases. J Craniomaxillofac Surg 40:347–353, Official Publication of the European Association for Cranio-Maxillo-Facial Surgery
Hormozi AK, Shahverdiani R, Mohammadi HR, Zali A, Mofrad HR (2011) Surgical treatment of metopic synostosis. J Craniofac Surg 22:261–265
Greenberg BM, Schneider SJ (2006) Trigonocephaly: surgical considerations and long term evaluation. J Craniofac Surg 17:528–535
van der Meulen JJ, Nazir PR, Mathijssen IM, van Adrichem LN, Ongkosuwito E, Stolk-Liefferink SA, Vaandrager MJ (2008) Bitemporal depressions after cranioplasty for trigonocephaly: a long-term evaluation of (supra) orbital growth in 92 patients. J Craniofac Surg 19:72–79
Renier D, Lajeunie E, Arnaud E, Marchac D (2000) Management of craniosynostoses. Child’s Nerv Syst: ChNS 16:645–658, Official Journal of the International Society for Pediatric Neurosurgery
Bottero L, Lajeunie E, Arnaud E, Marchac D, Renier D (1998) Functional outcome after surgery for trigonocephaly. Plast Reconstr Surg 102:952–958, discussion 959-960
Hayward R, Jones B, Evans R (1999) Functional outcome after surgery for trigonocephaly. Plast Reconstr Surg 104:582–583
Kapp-Simon KA, Speltz ML, Cunningham ML, Patel PK, Tomita T (2007) Neurodevelopment of children with single suture craniosynostosis: a review. Child’s Nerv Syst: ChNS 23:269–281, Official Journal of the International Society for Pediatric Neurosurgery
Kelleher MO, Murray DJ, McGillivary A, Kamel MH, Allcutt D, Earley MJ (2006) Behavioral, developmental, and educational problems in children with nonsyndromic trigonocephaly. J Neurosurg 105:382–384
Kelleher MO, Murray DJ, McGillivary A, Kamel MH, Allcutt D, Earley MJ (2007) Non-syndromic trigonocephaly: surgical decision making and long-term cosmetic results. Child’s Nerv Syst: ChNS 23:1285–1289, Official Journal of the International Society for Pediatric Neurosurgery
Warschausky S, Angobaldo J, Kewman D, Buchman S, Muraszko KM, Azengart A (2005) Early development of infants with untreated metopic craniosynostosis. Plast Reconstr Surg 115:1518–1523
Aryan HE, Jandial R, Ozgur BM, Hughes SA, Meltzer HS, Park MS, Levy ML (2005) Surgical correction of metopic synostosis. Child’s Nerv Syst: ChNS 21:392–398, Official Journal of the International Society for Pediatric Neurosurgery
Collmann H, Sorensen N, Krauss J (2005) Hydrocephalus in craniosynostosis: a review. Child’s Nerv Syst: ChNS 21:902–912, Official Journal of the International Society for Pediatric Neurosurgery
Da Costa AC, Anderson VA, Savarirayan R, Wrennall JA, Chong DK, Holmes AD, Greensmith AL, Meara JG (2012) Neurodevelopmental functioning of infants with untreated single-suture craniosynostosis during early infancy. Child’s Nerv Syst: ChNS 28:869–877, Official Journal of the International Society for Pediatric Neurosurgery
Shimoji T, Shimabukuro S, Sugama S, Ochiai Y (2002) Mild trigonocephaly with clinical symptoms: analysis of surgical results in 65 patients. Child’s Nerv Syst: ChNS 18:215–224, Official Journal of the International Society for Pediatric Neurosurgery
Shimoji T, Tomiyama N (2004) Mild trigonocephaly and intracranial pressure: report of 56 patients. Child’s Nerv Syst: ChNS 20:749–756, Official Journal of the International Society for Pediatric Neurosurgery
Warren SM, Proctor MR, Bartlett SP, Blount JP, Buchman SR, Burnett W, Fearon JA, Keating R, Muraszko KM, Rogers GF, Rubin MS, McCarthy JG (2012) Parameters of care for craniosynostosis: craniofacial and neurologic surgery perspectives. Plast Reconstr Surg 129:731–737
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kunz, M., Lehner, M., Heger, A. et al. Neurodevelopmental and esthetic results in children after surgical correction of metopic suture synostosis: a single institutional experience. Childs Nerv Syst 30, 1075–1082 (2014). https://doi.org/10.1007/s00381-013-2340-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-013-2340-0