Abstract
Introduction
The aim of this study was to evaluate the evolution in craniosynostosis in terms of incidence and management in the last 20 years and to discuss the clinical implications and future perspectives with regards to the practical organization of daily practice.
Methods
The relative incidence and management modalities of craniosynostosis hospitalized at the Craniofacial Unit of Necker, French National Referral Center for Faciocraniosynostosis, in two different quinquennia: 1985–1989 (group A) and 2003–2007 (group B) were reviewed.
Results
A total of 1,286 children were included in our study; group A 472, group B 814, that is an overall increase of 1.7-fold in the second period of the study. Sagittal synostosis remained the most frequent type (45% of cases in both groups). Conversely, the number of cases of Pfeiffer syndrome increased from seven patients to 20 (×2.8) and metopic synostosis cases increased from 49 to 193 (×3.9). Mean age at surgery in group A was 22.5 months and 13 months in group B.
Discussion
The comparison of the two quinquennia shows that there has been a change in the incidence of the different types of synostosis. The timing for surgery has also changed with the treatment of younger children in group B compared to group A. The principles of the surgical treatment of monosutural craniosynostosis have remained unmodified in our center. However, there has been an evolution in the techniques due to the introduction of new tools such as internal and external distractions, springs, and resorbable plates.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The aim of this study was to (1) evaluate the evolution which took place in the relative incidence of craniosynostosis and the changes that occurred in their management at the Craniofacial Unit of the Pediatric Neurosurgery Department of Necker Enfants Malades Hospital, in the last 20 years; (2) evaluate their impact on the current pediatric craniofacial practice; and (3) discuss the clinical implications and future perspectives with regards to the practical organization of daily clinical practice.
For this purpose, we compared the relative incidence and the management modalities of craniosynostosis in two different quinquennia: 1985–1989 and 2003–2007 in our institution which is a craniofacial referral center in France.
Patients and methods
The clinical documentation of the children hospitalized for craniosynostosis at the Craniofacial Unit of Necker Enfants Malades, French National Referral Center for Faciocraniosynostosis, during two 5-year periods, from 1985 to 1989 (group A) and from 2003 to 2007 (group B), was reviewed.
All patients selected for this study had a true synostosis confirmed by skull X-rays or computed tomography scanning. Nonsynostotic skull deformations such as positional plagiocephaly were excluded. Since early 1990s, all children with syndromic and familiar forms of craniosynostosis as well as unicoronal or bicoronal synostosis have been screened for genetic anomalies. Patients were subdivided according to their type of synostosis: sagittal, metopic, coronal (unicoronal or bicoronal), lambdoid, oxycephaly (sagittal and bicoronal), other nonsyndromic multisutural craniostenosis and syndromic cases. Demographic information such as date of birth, parental age at birth, birth weight, and age at presentation were also available.
Results
A total of 1,286 children were included in our study, 472 of them belonging to group A and 814 to group B.
Group A
The distribution according to the synostosis type of children in group A is summarized in Table 1. Among these children, 85.6% had a nonsyndromic craniosynostosis. Scaphocephaly was the most common synostosis (52.9%) followed by unicoronal synostosis (14.6%) and metopic synostosis (12.2%). Among scaphocephalic children in group A, 112 out of 214 (52%) were operated on. Crouzon syndrome was the most commonly found among the 68 syndromic cases of group A, affecting 30 children (mean of six cases per year, 45% of syndromic cases per year; 6.4% of the overall group A craniosynostosis). The mean age at surgery in this group was 22.5 months.
Group B
The distribution according to the synostosis type of children in group B is summarized in Table 1. Among the patients of this group, 87.4% had a nonsyndromic craniosynostosis. Scaphocephaly remained the most common type (51.9%) followed by metopic (27.1%) and unicoronal (11.4%) synostoses. Among the 369 children with sagittal synostosis in group B, 245 (66%) were operated on. Syndromic cases represented 103 children in group B. Crouzon syndrome was the most common (5.6 cases per year) as it occurred in group A but its relative incidence was reduced to 26.9% of syndromic cases per year and to 3.5% of the overall group B craniosynostosis.
Conversely, more children were affected by Pfeiffer syndrome in group B than in group A, seven of 68 and 20/103, respectively. The overall incidence of Pfeiffer syndrome changed from 1.5% in group A to 2.5% in group B. The mean age at surgery was 13 months in group B.
Discussion
-
Changing frequency of diseases
In these two quinquennia, more than 1,200 children presenting a craniofacial dysostosis were hospitalized at Necker Enfants Malades Hospital in Paris. The most obvious change observed between these periods was the increased admission for craniosynostosis in the second quinquennium as 92.6 patients per year was hospitalized in the period 1985–1989 versus 142.2 per year in the period 2003–2007 that is an overall increase of 1.7-fold. A better recognition of skull abnormalities by the pediatricians and care takers and/or an increased recruitment of patient in our center are the most likely causes of this changed figures. Indeed, an overall increase in the incidence of craniosynostosis in our country was in fact not documented in the same years.
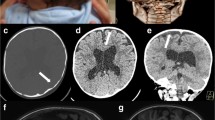
While the total number of patients hospitalized each year has increased, the ratio of syndromic and nonsyndromic synostosis children has remained stable, syndromic cases representing 14.4% of all the craniosynostosis hospitalized each year in group A and 12.6% in group B. However, some differences have been recorded concerning the relative incidence of the various types of complex synostosis (Fig. 1), probably depending on a more reliable type subdivision, at least in part. Indeed, an increase in frequency of Pfeiffer syndrome was found in our center in the second quinquennium. The number of cases increased from seven patients in group A to 20 in group B (×2.8-fold increase) whereas the total number of patients went from 472 to 814 (×1.7-fold increase). However, this relative increase of Pfeiffer syndrome was associated to a relative reduction in incidence of Crouzon syndrome suggesting a major awareness of morphological abnormalities, namely the great toe deviation and enlargement characteristic of Pfeiffer syndrome.
The analysis of the epidemiologic raw data shows also some significant changes in nonsyndromic synostosis (Fig. 1).
The most intriguing modification in nonsyndromic craniosynostosis regards metopic synostosis, the incidence of which increased in the second period of the study. Whereas the overall increase of cases between the two quinquennia was of 153%, metopic synostosis cases increased from 49 to 193, that is, a 3.9-fold increase. The relative proportion of cases with sagittal synostosis in groups A and B remained unchanged (45.3% in both groups), whereas trigonocephaly increased from 10.3% to 23.7% of the population here analyzed. The number of operated on trigonocephalic children also increased considerably (36 in group A, 132 in group B).
As a consequence, the rate of trigonocephaly to scaphocephaly that was only 1:5 20 years ago, changed to the current ratio of 50%.
According to our experience, as we have already reported [6–8], this increase seems to have started in the late 1980s and early 1990s and was confirmed by a recent analysis [5]. It is worth to note that similar changes in the relative incidence of trigonocephaly have also been noted by other centers in Western countries [16, 17]. Nevertheless, no clear factor to explain these modifications has been pointed out so far.
A significant and objective reduction in the number of oxycephalies was found when comparing the two groups, 33 and ten cases, respectively. More than a true epidemiologic change, this reduction is likely related to a reduction in the number of patients coming from north Africa countries where this particular type of craniosynostosis is common depending on the better management of the condition nowadays possible in their own hospitals.
-
Changing indications/timing/age
The comparison between the two periods here considered shows that patients' mean age at surgery has been dramatically reduced in our center, from 22.5 to 13 months, respectively. This reduction depends on several factors. Among them, the better knowledge of synostosis and an increased awareness of its possible late consequences by the pediatricians, obstetricians, and other caregivers are likely to have resulted in early diagnosis and referral of these patients, even though the erroneous belief that a spontaneous regression of the deformity is possible remains a common cause of delay in diagnosis and management.
In the same time, refinements in surgical treatment as compared to 20 years ago and the concomitant important improvements in pediatric intensive care and anesthesia have allowed the surgeons to adopt a policy of early surgical correction in the majority of cases. Consequently, to estimate heavy abrupt blood losses during operation, especially in low-weight infants and to precisely individuate subtle or dramatic preoperative hemodynamic abnormalities have become a major concern for the anesthetist faced with this type of surgical procedures. Control and limitation of homologous transfusions remain a further challenge for both the anesthetist during the surgical correction and for the intensivist in the early postoperative period. However, in the last years, more complex operations for cranial reconstruction and facial advancement have became possible, even in less than 8-kg-body-weight infants, without increasing anesthetic morbidity. Conversely, in group A, complex procedures were rarely performed in less than 8-kg body weight infants, and the need for homologous transfusion was somewhat overestimated, specifically in the postoperative period [11, 12]. Early complex surgical procedures, such as those carried out in the second period of this study, could not have been made possible without the progressive involvement of several specialists in the medical team and the acquisition of a multidisciplinary approach, which was not yet developed in the early period analyzed here.
Similarly, a major involvement of the neuropsychologists and the introduction of more refined tools for evaluation of the surgical outcome have emphasized the advantages of an early surgical correction [2, 4, 13, 14], consequently contributing at modifying the timing of the surgical management.
A similar improvement is also found in the recognition of those cases requiring an early surgical procedure. The dramatic difference in the management at operation between the two quinquennia analyzed demonstrates the impact of all the just-mentioned advancement unequivocally.
The increased knowledge of the possible negative impact of the craniosynostosis on the neuropsychological development may also have contributed to the overall increase in number of operated-on children in the more recent period especially in cases of simple synostoses as demonstrated, for example, by the statistically significant increase in the proportion of infants with sagittal synostosis operated on between the two periods, 52% and 66%, respectively (p < 0.01). To explain the absolute increase in number of cases treated in the two periods, a further explanation may be provided also by the current wider spectrum of indications for surgical correction in faciocraniosynostoses, with the improved understanding of the effects of the midface retrusion on the respiratory function which might occur already in early life [1, 10].
-
Impact of prenatal diagnosis and genetic analysis
The diagnosis of faciocraniostenosis might be obtained occasionally by ultrasound or intrauterine magnetic resonance imaging, based on anomalies of the brain or the extremities. However, prenatal diagnosis has had apparently a low influence on the epidemiology of craniosynostosis. The total number of children with Apert syndrome, for instance, a syndrome which can be diagnosed in utero due to the limb anomalies, augmented in the second quinquennium as compared to the first one, even though this relative increase (157%) remained inferior to that of the whole population with craniosynostosis admitted in our center 172% (Table 1). These figures, however, did not reach a statistical significance. On the other hand, the genetic analysis had a scarce impact on primary prevention.
The systematic screening of genetic anomalies in syndromic, familial, and coronal cases did have an obvious impact in our understanding of these diseases and resulted in the current better counseling of the families. The genetic analysis has provided some advantages in term of prognosis, too. For example, the presence of a mutation in FGFR3 gene in unicoronal or bicoronal synostosis has been found to be associated to worst functional and cosmetic results as compared to the nonmutated forms consequently allowing the surgeon to better predict the surgical outcome to the families [15]. Nevertheless, even though the improved genetic knowledge has not had a significant role in patients' recruitment at craniosynostosis prevention, it has certainly modified the relationship between the surgeon and the families in the two quinquennia. Currently, craniofacial surgeons have a better knowledge on the physiopathology of craniosynostosis and are more familiar with the genetic diagnosis; consequently, they are able to establish a more consensual relationship with the parents. Also, the parents are more informed (through the internet, blogs of other parents…). The more mature relationships between the surgeon and the parents is one of the most striking change observed to occur in the last years as compared with the first period when only the mechanical aspects of these malformations could be explained to the families.
-
Changing techniques (distractions/springs/resorbable plates)
The comparison of the two quinquennia shows that the principles of the surgical treatment of monosutural craniosynostosis have remained unchanged in our center.
Nonsyndromic synostoses are regarded as a whole distortion of the calvaria and not only the result of a single sutural dysfunction. That implies that no mere suturectomies were performed neither in group A nor group B patients. According to this principle, the endoscopic techniques were also not introduced in contrast with what is happening in several centers. Indeed most of the progresses done in the correction of these pathological conditions took place when simple suturectomies were substituted by more complex techniques of cranial remodeling. Currently, the revival of strip craniectomies, even though made possible by recently introduced less invasive techniques, does represent, in our opinion, a regression in the theoretical and practical management of craniosynostosis.
On the other hand, the management of faciocraniosynostosis has greatly changed between the two quinquennia. It was in fact greatly modified by the application of the distraction techniques to craniofacial surgery.
Traditionally, faciocraniosynostosis were managed by a two-stage strategy with a frontoorbital advancement in the first year and a delayed facial advancement (Lefort III) at, at least, 5 years of age [1]. But the morbidity of the classic approach of frontofacial monobloc advancement was high. In our center 20 years ago, the rate of frontal infections was evaluated close to 30% [1]. The use of internal distraction devices has allowed a simultaneous treatment in a single stage. The efficacy of the procedure has increased and, in the same time, its morbidity was reduced to an acceptable rate [1]. Indeed, the gradual advancement obtained by distraction reduces the retrofrontal dead space and allows a progressive anterior expansion of the dura and brain to occur. A significant improvement at the level of skull expansion, exorbitism correction, and breathing obstruction can thus be achieved even in the very young patients [1]. Similar results can be achieved with rigid external distraction system too [18].
Resorbable plates and screws have been utilized used craniofacial surgery routinely since 1999 [3]. They have been successfully used in trigonocephalies, plagiocephalies, brachycephalies, and in all other cases when an immediate rigid fixation is required. Their resorption in a few months allows bone reossification and consolidation to occur.
The development of springs has also changed current indication and techniques in craniosynostosis treatment [9]. In our center, they are used mainly in posterior vault remodeling. Springs can be applied through a patent suture or through an osteotomy to ensure a strain force. Their use is promising especially in parieto-occipital deformities.
Conclusions
The epidemiology of craniosynostosis has remained relatively stable in our center in the periods analyzed. Consequently, the workload related to this type of malformation did not change significantly. On the other hand, the management of these conditions has been mainly influenced by the progresses in basic research, which have resulted in a better understanding of the underlying psychopathogenetic mechanisms. These progresses require the neurosurgeon to be acquainted with an increasing amount of new information and to be more involved with other specialists and with the families. This multidisciplinary approach has had also an impact on the clinical practice, with an increasing number of infants and children with syndromic craniosynostoses being operated in an early age. The early treatment has been made possible also by the introduction of new material, more refined surgical tools, and more aggressive surgical techniques. The complexity of the theoretical and practical armamentarium nowadays necessary for treating craniosynostoses emphasizes the referral of patients to supraregional referral centers where multidisciplinary teams including genetecist, pediatric neurosurgeons, maxillofacial surgeons, ear, nose, and throat specialists, and ophthalmologic psychologists assure the child with craniosynostoses to the best available treatment.
References
Arnaud E, Marchac D, Renier D (2007) Reduction of morbidity of the frontofacial monobloc advancement in children by the use of internal distraction. Plast Reconstr Surg 15:120(4):1009–1026
Arnaud E, Renier D, Marchac D (1995) Prognosis for mental function in scaphocephaly. J Neurosurg 83(3):476–479
Ashammakhi N, Renier D, Arnaud E, Marchac D, Ninkovic M, Donaway D, Jones B, Serlo W, Laurikainen K, Törmälä P, Waris T (2004) Successful use of biosorb osteofixation devices in 165 cranial and maxillofacial cases: a multicenter report. J Craniofac Surg 15(4):692–701
Bottero L, Lajeunie E, Arnaud E, Marchac D, Renier D (1998) Functional outcome after surgery for trigonocephaly. Plast Reconstr Surg 102(4):952–958
Di Rocco F, Arnaud E, Renier D (2009) Evolution in the frequency of non syndromic craniosynostosis. J Neurosurg (in press)
Lajeunie E, Barcik U, Thorne JA, El Ghouzzi V, Bourgeois M, Renier D (2001) Craniosynostosis and fetal exposure to sodium valproate. J Neurosurg 95(5):778–782
Lajeunie E, Le Merrer M, Arnaud E, Marchac D, Renier D (1998) Trigonocephaly: isolated, associated and syndromic forms. Genetic study in a series of 278 patients. Arch Pediatr 5(8):873–879
Lajeunie E, Le Merrer M, Marchac D, Renier D (1998) Syndromal and nonsyndromal primary trigonocephaly: analysis of a series of 237 patients. Am J Med Genet 13;75(2):211–215
Lauritzen CG, Davis C, Ivarsson A, Sanger C, Hewitt TD (2008) The evolving role of springs in craniofacial surgery: the first 100 clinical cases. Plast Reconstr Surg 121(2):545–554
Mathijssen I, Arnaud E, Marchac D, Mireau E, Morisseau-Durand MP, Guérin P, Renier D (2006) Respiratory outcome of mid-face advancement with distraction: a comparison between Le Fort III and frontofacial monobloc. J Craniofac Surg 17(5):880–882
Meyer P, Renier D, Arnaud E, Jarreau MM, Charron B, Buy E, Buisson C, Barrier G (1993) Blood losses during repair of craniosynostosis. BJA 71:854–857
Orliaguet G, Bruyère M, Meyer P, Blanot S, Renier D, Carli P (2003) Comparison of perioperative blood salvage and postoperative reinfusion of drained blood during surgical correction of craniosynostosis in infants. Pediatr Anaesth 13:797–804
Renier D, Arnaud E, Cinalli G, Sebag G, Zerah M, Marchac D (1996) Prognosis for mental function in Apert's syndrome. J Neurosurg 85(1):66–72
Renier D, Arnaud E, Marchac D (2006) Functional retardation in craniosynostosis. Neurochirurgie 52(2–3 Pt 2):259–263
Renier D, Lajeunie E, Arnaud E, Marchac D (2000) Management of craniosynostoses. Childs Nerv Syst 16(10–11):645–658
Selber J, Reid RR, Chike-Obi CJ, Sutton LN, Zackai EH, McDonald-McGinn D, Sonnad SS, Whitaker LA, Bartlett SP (2008) The changing epidemiologic spectrum of single-suture synostoses. Plast Reconstr Surg 122(2):527–533
Van der Meulen J, van der Hulst R, van Adrichem L, Arnaud E, Chin-Shong D, Duncan C, Habets E, Hinojosa J, Mathijssen I, May P, Morritt D, Nishikawa H, Noons P, Richardson D, Wall S, van der Vlugt J, Renier D (2009) The increase of metopic synostosis; a pan-European observation. J Craniofac Surg (in press)
Yu JC, Fearon J, Havlik RJ, Buchman SR, Polley JW (2004) Distraction osteogenesis of the craniofacial skeleton. Plast Reconstr Surg 114(1):1E–20E
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Di Rocco, F., Arnaud, E., Meyer, P. et al. Focus session on the changing “epidemiology” of craniosynostosis (comparing two quinquennia: 1985–1989 and 2003–2007) and its impact on the daily clinical practice: a review from Necker Enfants Malades. Childs Nerv Syst 25, 807–811 (2009). https://doi.org/10.1007/s00381-009-0864-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-009-0864-0