Abstract
Background
Torticollis, despite being well-known neurological manifestation, is often underestimated as a first symptom of the abnormalities of posterior cranial cavity and cervical spinal cord.
Objectives
The purpose of this study is to analyze the occurrence of acquired torticollis in children as a herald sign of the tumors of the cervical spinal cord or of the posterior fossa.
Methods
Clinical records of 54 cases treated for the tumor of the cervical spinal cord or posterior fossa (including congenital ones) were retrospectively reviewed. The following data were calculated: the occurrence of the torticollis as a first sign of tumors, the duration time from the onset of the symptoms to diagnosis, the concurrence of other pathological symptoms, and the diminishing of symptoms of the torticollis following treatment.
Results
In 12/54 (22.2 %) torticollis was first sign of central nervous system tumor and in all of them preceded other neurological symptoms. The time from the onset of torticollis to establishing diagnosis ranged from 2 to 52 weeks (9.6 weeks on average). Eleven of twelve patients were treated surgically—in 10 of them, torticollis disappeared in the postoperative course.
Conclusions
Torticollis may be a herald sign of the tumor of the cervical spinal cord or the posterior fossa. Those pathologies should be considered in the differential diagnosis of the torticollis, particularly if accompanied by other symptoms of the focal pathology of central nervous system. Awareness of this fact may shorten the time to establish the proper diagnosis. Torticollis necessitates exclusion of the posterior fossa and spinal cord tumor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term “torticollis” is derived from the Latin words tortus, meaning twisted, and collum—meaning neck. Torticollis is a pathological clinical sign that includes involuntary flexion of neck to the affected side and rotation to the opposite direction, resulting in the ear tilting toward shoulder and chin turning in the opposite direction. This deformation may be secondary to the wide spectrum of underlying, congenital as well as acquired pathologies. Congenital torticollis, most often of the muscular origin is caused by the fibrous scar formation in the sternocleidomastoideus muscle due to the abnormal intrauterine fetus position, birth trauma, or as a result of the resolution of preexisting cystic hygroma or else branchial cleft cyst. Another, less common causes of congenital torticollis include the congenital abnormalities of the cervical spine (failure of cervical spine formation, segmentation, Klippel–Feil syndrome) [1].
Acquired torticollis presenting in otherwise healthy patient is frequently the only or the first clinical sign of wide range of causative pathologies like syringomyelia, encephalitis, type II neurofibromatosis, musculoskeletal pathologies (cervical intervertebral disc herniation, cervical discitis, neck injury) and cervical spine tumors and tumor-like lesions. Apart from the pathologies of the central nervous system (CNS), ophthalmological problems (ocular abnormal head posture, AHP) [2] as well as laryngological conditions and contracting skin scars may lead to the torticollis. The aforementioned conditions usually necessitate multidisciplinary approach to establish proper diagnosis.
Torticollis is a also a term often used to describe pathologies referred to as cranial and cervical dystonia, manifesting by forced position of the head and neck determined by direction of motion disturbances [3].
The group of conditions that are obviously underestimated, rarely being taken into account in the first-line differential diagnosis in case of congenital or acquired sudden-onset or gradually developing non-dystonic torticollis in children are the lesions located in the posterior cranial cavity, particularly tumors of the posterior cranial fossa and/or tumors of the cervical spine cord. Unawareness of this may lead to delay diagnosis with life-threatening consequences. To the best of the authors' knowledge, there is paucity of data on this topic in English literature—we are aware of only a few reports of torticollis related to tumors and reporting only small series of cases [3–5].
Objective
Therefore the aim of present study was to analyze:
-
1.
The occurrence of non-dystonic torticollis in children as the first sign of cervical spine cord and/or posterior cranial cavity tumor and the duration from onset of the symptoms to the diagnosis of tumor
-
2.
The occurrence of concomitant symptoms of CNS tumor, preceding, coexisting with, or following the torticollis in this group of patients
-
3.
Frequency of the resolution of the torticollis after causative treatment of tumor
Material and methods
Fifty-four consecutive cases (24 girls, 30 boys, aged 5 months to 10 years; 3.9 years on average at the time of diagnosis of tumor) were treated for the posterior fossa or cervical spinal cord tumor (33 and 21 children, respectively) in our institution (Pediatric Neurosurgery Department) between 2005 and 2012.
All children on clinical examination at admission presented signs or symptoms of CNS pathology, suggestive of the process in the posterior cranial cavity and/or cervical spinal cord. Every patient after detailed neurological clinical examination underwent diagnostic imaging (MRI or CT scan of head and/or cervical spinal cord). All patients were qualified to surgical treatment and/or adjuvant chemotherapy/radiotherapy (if indicated) according to current standards (the details of the therapy exceed the scope of present study).
Complete clinical records of all patients were available and were reviewed retrospectively to calculate the occurrence of non-dystonic torticollis in children as a first sign of cervical spine cord and/or posterior cranial cavity tumor. This “torticollis-manifested” cohort was further analyzed. The following data were calculated: (1) the duration time of the torticollis from onset of symptoms to diagnosis of tumor (2) the occurrence of concomitant symptoms of CNS tumor following the torticollis. We also investigated the effect of tumor surgery on subsiding of the symptoms of torticollis.
Results
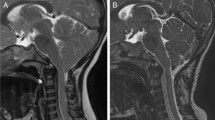
Torticollis as a first sign of CNS tumor was noted in 12/54 (22,2 %) patients of the analyzed group (five girls, seven boys, aged 4 months to 10 years; 3.3 years on average)—in eight cases on the right side, in four on the left. In 10/12 cases, tumor was located in the posterior cranial fossa (Fig. 1), whereas in further two in the cervical spinal cord (Fig. 2). Thus, the occurrence of non-dystonic torticollis as a symptom of tumor was almost one third in posterior cranial fossa tumors (10/33), versus 9.5 % in cervical spinal cord tumors (2/21).
MRI scans of 1.5-year-old boy. First alarming sign was left-side tilt of the head and limited range of motion of cervical spine. Patient was treated with rehabilitation without satisfactory results. 4 months later MRI examination revealed intraspinal tumor of C5–Th7: a sagittal section, b frontal cross-section
The time from the onset of the torticollis and/or its noting by the caretakers or the healthcare specialist to the diagnosis the CNS tumor ranged in the analyzed group from 2 to 52 weeks (mean 9.6 weeks).
In all cases, torticollis was followed by other clinical symptoms of CNS pathology, present at the time of diagnosis of tumor. Those signs are summarized in the Table 1, along with patients' demographic data and details concerning the location, histological type, and grading of the tumor (according to WHO classification of CNS tumors).
All 12 patients underwent surgical treatment. Radical excision of the tumor was carried out in 10 patients; in two, definitive surgical treatment was not possible: in one of them, due to a multifocal presentation (only partial excision of one tumor focus was performed). In another case, the brainstem location of the tumor precluded any efficient surgical intervention—only diagnostic biopsy was done to confirm the histological type of tumor.
In all 10 patients that had have tumor radically excised, torticollis disappeared totally in the postoperative course.
Two patients died: one due to recurrence of high-grade tumor (PNET) localized in IV ventricle; another due to progression of the multifocal low grade but inoperable lesion.
Table 2 shows details of the treatment and results of surgical treatment in study group.
Discussion
Torticollis in child may result from many etiological factors, including CNS tumors. Unfortunately, tumors of posterior cranial fossa and/or cervical spinal cord are rarely considered in primary differential diagnosis as a cause of forced head positioning. Thus, in clinical practice torticollis is still commonly treated symptomatically, without exclusion of serious underlined CNS lesions. This obviously makes conservative treatment and rehabilitation ineffective and, which is of more important, causes a delay of the proper diagnosis and implementation of adequate therapy [5–7].
Although the exact mechanism of the CNS tumor-associated torticollis remains obscure, the most commonly postulated explanations of this phenomenon include the accessory (XI) nerve pressure or the dura mater stretching, causing pain and involuntary position of the head [3]. It is also emphasized that motor neurons of external branch of accessory cranial nerve (supplying sternocleidomastoideus and rhomboideus muscles) are located in cervical spinal cord and in consequence intraspinal tumor can impair the function of the accessory nerve leading to torticollis or forced reflectory position of the head in extension (due to uni- or bilateral paresis of sternocleidomastoideus muscle) [8].
There are a few reports in the literature concerning the presence of the torticollis as a first clinical sign of cervical spine cord neoplasm [9–11]. Shy et al. found in his series that misdiagnosis of torticollis in children is associated with an “unacceptable delay ” in proper diagnosis and treatment of tumor in this location [7].
Intracranial tumors are the most common solid neoplasms in children, with reported incidence between 2.4 and 4.0/100,000/year [4]. Posterior cranial fossa tumors approximate 60–70 % of all brain tumors in children [12, 13]. Clinical symptoms include headache, nausea and vomiting, disorders of consciousness, ataxia, visual disturbances (nystagmus and diplopia), or cranial nerves deficits [4, 12, 13]. The presence of such alarming neurological symptoms usually tends to extend the diagnostic process by employing the imaging of posterior cranial fossa, brainstem and cervical spinal cord. In contrast, torticollis as a first sign of CNS pathology, despite the data pointing, its relatively high occurrence in this group of patients, seems to be ignored. The occurrence of torticollis in the present study in posterior cranial fossa tumor subgroup reached 30 %, which is in concordance with results presented by the other authors. Extremera et al. analyzed the group of 142 children with posterior cranial fossa tumor (aged 5 months to 16 years at presentation), and found that torticollis was present in 33 patients (23 %), predominantly in children aged 2 to 8 years (22 out of 74, 30 %) [13]. Torticollis was most often seen in astrocytomas (5/6) and ependymomas (6/19). Tumors were located at the cerebellum (57 %), the fourth ventricle (17 %), and the brainstem (13 %). The clinical symptoms included: vomiting (60 %), ataxia (51 %), headache (48 %), focal neurological signs (38 %), behavioral disturbances (irritability, decay) (29 %), torticollis (23 %), diplopia (12 %), nystagmus (11 %), seizures (4 %), and coma (4 %) [13].
Dorner et al. found torticollis to be the seventh most frequent symptom of posterior cranial fossa tumor in children, following: headache, vomiting, nausea, reduced level of consciousness, ataxia, and cranial nerve deficits [4]. Marmon et al. defined the triad of clinical symptoms characteristic for tumor in this location in children including photophobia, lacrimation and torticollis [14].
The time interval between onset of symptoms and establishing the definite diagnosis ranges from 5 to 535 days (142 days on average) according to literature, [3, 4, 7] which is similar to the data obtained from present analysis. Particularly those tumors of cervical spinal cord and posterior cranial fossa that initially manifest exclusively by torticollis may be diagnosed with significant delay, frequently no sooner than additional life-threatening symptoms (resulting from further course of the tumor growth) supervene. The reason for that is that despite those tumors are among the most common solid neoplasms in children, they are still relatively rare and tend to be misdiagnosed for more common pathologies [4, 6, 7, 9–11, 15]. Patients are treated for gastrointestinal problems, appendicitis, psychological and behavioral problems, cervical spine sprain, ocular AHP, etc. The awareness of brain tumors in children within the population is low; the knowledge among physicians is limited. Furthermore the presentation is often nonspecific, especially in infants and toddlers up to the age of 3 years [4]. Posterior cranial fossa tumors do not cause seizures as occasionally seen in supratentorial tumors.
Sudden-onset, nontraumatic torticollis should therefore always raise a suspicion of spinal cord tumor or posterior fossa tumor, especially if other symptoms of focal lesions of CNS or signs of intracranial hypertension coincide and as such should undergo detailed diagnosis to confirm or rule out underlying CNS pathology. Tumors that arise from the floor of the fourth ventricle are associated with torticollis and ataxia. Spinal cord lesions can be associated with back pain, sciatica, scoliosis, and extremities weakness [12]. Concomitant symptoms of focal CNS pathology and/or intracranial pressure was present at the time of definite diagnosis in all cases in the analyzed group (Table 1), such a coincidence was also reported by others [4, 12, 13].
Conclusions
Torticollis is a frequent herald sign of posterior cranial fossa and/or cervical spinal cord tumor. The delay between its occurrence and proper diagnosis of underlying CNS pathology is often unacceptably long. Torticollis concomitant symptoms are always present in those patients, indicating focal CNS pathology and/or intracranial pressure. After causative, radical treatment torticollis diminishes in the following course of the disease.
References
Marciniak W, Szulc A (2008) Brevicollis, Syndroma Klippel-Feil In: Wiktora Degi Ortopedia i Rehabilitacja, PZWL, Warszawa 2008, pp 55–56
Boricean ID, Bărar A (2011) Understanding ocular torticollis in children. Oftalmologia 55(1):10–26
Mutsaers P, Fick M, Plotz FB (2007) Acquired torticollis as the only initially presenting symptom in child with a brainstem glioma. Eur J Pediatr 166:1075–1076
Dorner L, Fritsch MJ, Stark AM, Mehdorn HM (2007) Posterior fossa tumors in children: how long does it take to establish the diagnosis? Childs Nerv Syst 23:887–890
Bussieres A, Cassidy JD, Dzus A (1994) Spinal cord astrocytoma presenting as torticollis and scoliosis. J Manip Physiol Ther 17(2):113–118
Drozyńska E, Połczyńska K, Bień E et al (2004) Solid tumours of the vertebral column and spinal cord in children. Reasons and consequences of diagnostic delay. Med Wieku Rozwoj 8:183–191
Shay V, Fattal-Valevski A, Beni-Adani L, Constantini S (2012) Diagnostic delay of pediatric brain tumors in Israel: a retrospective risk factor analysis. Childs Nerv Syst 28(1):93–100
Turgut M, Akalan N, Bertan V, Erbengi A, Eryilmaz M (1995) Acquired torticollis as the only presenting symptom in children with posterior fossa tumors. Childs Nerv Syst 11:86–88
Denaro L, Longo UG, Papalia R et al (2008) Eosinophilic granuloma of the pediatric cervical spine. Spine 33(24):936–941
Kiwak KJ, Deray MJ, Shields WD (1983) Torticollis in three children with syringomyelia and spinal cord tumor. Neurology 33(7):946–948
Visudhiphan P, Chiemchanya S, Somburanasin R, Dheandhanoo D (1982) Torticollis as the presenting sign in cervical spine infection and tumor. Clin Pediatr (Phila) 21(2):71–76
Kumandaş S, Per H, Gümüş H, Tucer B, Yikilmaz A, Kontaş O, Coşkun A, Kurtsoy A (2006) Torticollis secondary to posterior fossa and cervical spinal cord tumors: report of five cases and literature review. Neurosurg Rev 29:333–338
Extremera VC, Alvarez-Coca J, Rodriguez GA (2008) Torticollis is a usual symptom in posterior fossa tumors. Eur J Pediatr 167:249–250
Marmor MA, Beauchamp GR, Maddox SF (1990) Photophobia, epiphora, and torticollis: a masquerade syndrome. J Pediatr Ophthalmol Strabismus 27:202–204
Straussberg R, Harel L, Amir J (2002) Pseudotumor cerebri manifesting as stiff neck and torticollis. Pediatr Neurol 26:225–227
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fąfara-Leś, A., Kwiatkowski, S., Maryńczak, L. et al. Torticollis as a first sign of posterior fossa and cervical spinal cord tumors in children. Childs Nerv Syst 30, 425–430 (2014). https://doi.org/10.1007/s00381-013-2255-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-013-2255-9