Abstract
Purpose
The clinical value of electroencephalography (EEG) in pediatric moyamoya disease has been underestimated, though the characteristic patterns are well known. We undertook this study to evaluate the clinical value of EEG as a diagnostic and postoperative follow-up modality in pediatric moyamoya disease.
Methods
We retrospectively reviewed the pre and postoperative EEG with effective hyperventilation in 127 pediatric moyamoya patients and compared their patterns with hemodynamic images.
Results
One hundred and two patients (80.3 %) among 127 showed abnormal EEG findings before revascularization surgery. The typical rebuild-up phenomenon was observed in 82 (64.6 %) and localized build-up in 32 (25.2 %) without any significant clinical ischemic events during and after hyperventilation. The rebuild-up was observed more frequently in younger age groups (less than 13 years) and Suzuki stages III. The location of the rebuild-up distribution and asymmetric build-up was consistent with the area showing hemodynamic abnormalities on single photon emission computed tomography and/or perfusion magnetic resonance imaging. Postoperative follow-up EEGs were performed in 41 patients. Six patients with remaining rebuild-up in postoperative follow-up EEG showed poorer postoperative clinical outcomes.
Conclusions
This study may reappraise EEG as an easy, safe, and adjunctive diagnostic and postoperative follow-up modality for evaluation of hemodynamic status and clinical outcome, especially in children with moyamoya disease.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Moyamoya disease is a vascular disorder showing progressive narrowing of the internal carotid artery at the level of its terminal bifurcation, with abnormalities involving the anterior and middle cerebral arteries [17, 23]. It is a common and important cerebrovascular disorder in children, especially in regions of East Asia [1, 12, 28]. Clinical and basic knowledge about moyamoya disease has increased considerably [11, 17, 20] since 1969 when Suzuki and Takaku [23] first described this disease.
The characteristic electroencephalogram (EEG) features of moyamoya disease were previously described by Kodama and colleagues [15] in 1979. These distinctive EEG findings, which are usually observed only in pediatric moyamoya patients, include the high amplitude slow waves called posterior or centrotemporal slowing and the rebuild-up phenomenon, which is indicated by the reappearance of high amplitude slow waves at 20–60 s after the cessation of hyperventilation during EEG recording. Although this characteristic EEG pattern in pediatric moyamoya disease is well known [15, 16, 18, 22], it has been thought that EEG in this disorder has little clinical value. The aim of this study was to analyze the pre and postoperative features of EEG and to evaluate the clinical value of EEG as a diagnosis and follow-up modality in pediatric moyamoya disease.
Methods
Patients
This study included 127 patients who underwent surgical interventions for the treatment of moyamoya disease at the Pediatric Clinical Neuroscience Center, Seoul National University Children’s Hospital from July 2003 to August 2009. During this period 286 children with moyamoya disease underwent indirect bypass surgery at our center. Among these 286 patients, 127 patients who satisfied the following criteria were enrolled from our cohort retrospectively: (1) patients with bilateral (N = 106) or unilateral (N = 21) moyamoya disease who underwent indirect bypass operation in the involved cerebral hemispheres; and (2) patients with effective preoperative hyperventilation digital waking EEGs. The study received ethics approval by the institutional review board.
Preoperative evaluations and operations
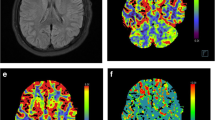
The diagnoses of all patients were confirmed by conventional angiography and their preoperative angiographic stage according to Suzuki’s classification [23] was evaluated. The clinical features of all 127 patients before surgical intervention were evaluated by review of medical records. Magnetic resonance imaging (MRI) performed with a 1.5-T unit (Sigma, GE Medical Systems, Milwaukee, WI, USA) was checked in all patients and the evidence of acute or chronic parenchymal lesions was evaluated. Perfusion MRI was performed (N = 125) using a gradient echo single-shot echo-planar image sequence, following an intravenous bolus injection of 0.1 mmol/kg of gadopentetate dimeglumine (Magnevist, Berlex Laboratories, Wayne, NJ, USA)[14]. The regional cerebral blood volume (rCBV) map and the time to peak (TTP) images were reviewed on the perfusion MRI. Basal and acetazolamide stress brain single photon emission computed tomography (SPECT) using a triple-headed SPECT system (Prism 3000 SPECT camera, Picker International Inc., Cleveland, OH, USA) with 99mTc-hexamethylpropyleneamin oxime (HMPAO; Amersham, Buckinghamshire, UK) was also performed [21] in most of the patients (N = 125). The SPECT image was assessed to determine whether it showed decreased regional cerebrovascular reserve (rCVR). Decreased rCVR was defined as cerebral perfusion of acetazolamide stress SPECT falling into a lower color range than basal SPECT over at least one-third of any brain lobe [21]. Of the 127 patients, 97 patients underwent encephaloduroarteriosynangiosis using bilateral superficial temporal artery with or without bifrontal encephalogaleoperiosteal synangiosis [9] in two stages, one side then the other side. Thirty patients including 17 unilateral moyamoya patients underwent unilateral operation only. The median duration between the first and second operation was 3.4 months (range 0.9–46.8 months).
Postoperative follow-up evaluations
Among 127 patients, we successfully analyzed postoperative follow-up EEGs in 41 patients. The limitations were due to irregular visits to our out-patient clinic after the operation and ineffective hyperventilation during EEG recordings. In our institution, we routinely perform follow-up EEGs at least 3 months after the revascularization operation since the average period needed for revascularization has known to be at least 3 months or longer. In 41 patients, the follow-up EEG recordings were available at least 3 months (median 16 months, range 3 months to 60.5 months) after the bilateral indirect bypass operation for the treatment of moyamoya disease was completed, or after the unilateral hemispheric operation in eight unilateral moyamoya patients.
The clinical outcomes of 41 patients were classified into four groups: [11, 13] (1) excellent: the preoperative symptoms such as transient ischemic attack (TIA) had totally disappeared without fixed neurological deficits; (2) good: the symptoms had totally disappeared but the neurological deficits remained; (3) fair: the symptoms persisted but their frequency had decreased; and (4) poor: the symptoms remained unchanged or worsened. Postoperative basal and acetazolamide stress brain SPECT was performed in all 41 patients. The follow-up SPECT findings were classified into two groups: [13] (1) favorable: SPECT scans demonstrated no hemodynamic abnormalities or a decrease in the size of hemodynamic abnormalities compared to preoperative images; and (2) unfavorable: SPECT scans demonstrated no change in the size of hemodynamic abnormalities or revealed new hemodynamic abnormalities. The hemodynamic abnormalities included perfusion defects, decreased perfusion, and/or decreased rCVR. Postoperative perfusion MRI was performed in 35 patients. The follow-up perfusion MRI findings were compared with the preoperative ones and also classified into two groups: [13] (1) favorable: patients whose perfusion MRI demonstrated no hemodynamic abnormalities or a decrease in the size of hemodynamic abnormalities; and (2) unfavorable: patients whose perfusion MRI demonstrated no change in the size of hemodynamic abnormalities or showed new hemodynamic abnormalities. The hemodynamic abnormalities included increased or decreased rCBV and/or delayed TTP.
EEG analyses
Routine 19-channel digital EEGs were performed according to the international 10–20 system, with a Grass-Telefactor, Twin EEG system (Grass Technologies, West Warwick, RI, USA). We applied longitudinal bipolar and referential montage (Pz reference) for EEG analysis. The patients were encouraged to breathe deep sustained breaths during EEG recording and examiners carefully monitored adverse events such as TIA or headache. EEGs were recorded continuously for more than 20 min, of which at least 5 min recorded after cessation of the hyperventilation was included in each record. The optimal hyperventilation activation conditions were determined to be a respiratory rate of 30/minute, threefold increase in resting expiratory volume, and duration over 3 min. Three different pediatric neurologists interpreted the EEG recordings after being blinded with patients’ clinical information. The following characteristics of the EEG records were evaluated: (1) background activity abnormalities; (2) changes with hyperventilation; and (3) spike or sharp wave discharges. Background abnormalities included localized or generalized slow waves and abnormal changes of amplitude [3]. Changes with hyperventilation included build-up and rebuild-up phenomenon. The normal build-up response consisted of generalized slow waves that began soon after the onset of hyperventilation and ended within 1 min after the patient stopped hyperventilation [3]. Normal slow waves of hyperventilation were not consistently localized or lateralized in distribution even though they might have a maximum in the anterior or posterior head regions. Rebuild-up was defined as continuous slow waves appearing within 20–60 s and lasting for 30 s or more after the termination of hyperventilation without temporary subsidence [15]. Delta frequency waves (under 4 Hz) with the high amplitude over 100 μV that persisted for at least 30 s were considered as a significant rebuild-up phenomenon. Localized build-up and rebuild-up consisted of slow waves that appeared mainly at one or a few electrodes and lateralized build-up and rebuild-up consisted of slow wave appeared only or mostly on one side of the hemisphere. The cerebral region showing a localized rebuild-up pattern was compared with the region showing hemodynamic abnormalities in SPECT and perfusion MRI.
Statistical analyses
The t test was used in the comparison of age between the patients showing rebuild-up and those not showing rebuild-up. The kappa value was used to evaluate the concordance between build-up and rebuild-up phenomena in each patient. The Fisher Exact test was used to compare postoperative clinical outcomes with the appearance of remaining rebuild-up phenomena after surgical revascularization. We used SPSS 17.0 for statistical analysis. For all tests, a p value less than 0.05 was considered significant.
Results
Clinical characteristics
There were 44 male patients and 83 female patients. The median age of symptom onset was 7 years 2 months and the median duration between symptom onset and first surgical intervention was 13 months. The most common clinical symptom was TIA (N = 112, 88.2 %), which was often associated with hyperventilation in situations such as crying and eating hot spicy foods. Headache (N = 52, 40.9 %) was the second most common clinical presentation and ten patients (7.9 % of total included patients) complained of chronic headache as the single clinical symptom of moyamoya disease. The MRI showed the evidence of major cerebral infarction in 35 patients (27.6 %), of whom eight patients (6.3 %) showed an acute infarction at the point of diagnosis. One hundred and ten patients (86.6 %) showed bilateral disease involvement and only 17 patients (13.4 %) showed unilateral involvement, of which six were right hemispheric and 11 were left hemispheric moyamoya patients. Based on the more involved hemisphere, the numbers of patients in each stage of Suzuki’s classification were three (2.4 %), 21 (16.5 %), 79 (62.2 %), 18 (14.2 %), six (4.7 %), and zero (0 %) in ascending stage order. Perfusion MRI (N = 125) and SPECT (N = 125) revealed abnormal findings in 120 patients (96.0 %) and 117 patients (93.6 %), respectively.
Of the 41 patients who underwent postoperative follow-up EEGs, 25 (61.0 %) were classified into the excellent clinical outcome group, two (4.9 %) to the good outcome group, 11 (26.8 %) to the fair outcome group, and the remaining three patients (7.3 %) to the poor outcome group. Nine of 41 patients (22.0 %) revealed unfavorable outcomes in SPECT and six of 35 patients (17.1 %) in perfusion MRI.
Preoperative EEG
During the 127 preoperative EEG recordings with the hyperventilation activation procedure, no significant neurologic symptoms including motor TIA were reported. Two patients had complained of brief numbness of the unilateral hand, which completely recovered soon after the cessation of hyperventilation without any residual neurologic deficits. One hundred and two patients (80.3 %) showed abnormal EEG findings before revascularization surgery.
Background activity abnormalities in preoperative EEG
Forty-two patients (33.0 %) showed background activity abnormalities. Slow wave and asymmetric posterior alpha rhythm were the main background abnormalities. Localized or generalized slow waves appeared in 31 patients (24.4 %). Of the eight patients who had experienced acute major infarction at the point of diagnosis, six patients showed fixed localized slow waves. Asymmetry of posterior alpha rhythm during the waking EEG record appeared in 19 patients (15.0 %). Stage І and ІІ sleep EEG records were performed in 56 patients, of whom seven (12.5 %) showed asymmetric sleep parameters. Posterior slow waves (N = 16, 12.6 %), centro-temporal slow waves (N = 4, 3.1 %), and diffuse low voltage pattern (N = 2, 1.6 %), which Kodama and colleagues [8] had previously described as characteristic features in childhood moyamoya disease, were observed less frequently than in the previous report.
-
1.
EEG changes with hyperventilation
A build-up of slow waves during hyperventilation appeared in 88 (69.3 %) patients, and rebuild-up of high-amplitude slow waves within 20–60 s after termination of hyperventilation was observed in 82 (64.6 %) patients. Localized or lateralized build-up appeared in 32 patients (25.5 %). Statistical analysis using the kappa value between build-up and rebuild-up phenomenon revealed significant concordance of these EEG changes with hyperventilation (kappa value 0.681, p = 0.00).
Because the build-up is known to disappear with advanced age [30], we divided the subjects into five age groups (4–6, 7–9, 10–12, 13–15, and over 16 years) and compared the differences in EEG changes with hyperventilation (Fig. 1a). Both build-up and rebuild-up were rarer when the patients reached ages greater than 13 years old. Comparing the two groups of patients with (N = 82) and without rebuild-up (N = 45), the average age of the former group was significantly less (101.7 ± 30.0 months) than that of the latter group (124.8 ± 44.6 months; p = 0.03).
Fig. 1 The appearance of the rebuild-up phenomenon according to the Suzuki stages [23] of the more involved hemisphere (Fig. 1b). Thirty-two patients with significant differences in disease involvement of both hemispheres (Suzuki stage gap ≥ 2) were excluded from this analysis. The rebuild-up phenomenon appeared most frequently in patients of Suzuki stage 3 (N = 44, 74.6 %), which is known to be the period with the most prominent moyamoya vessels at the base of the brain. The EEG records of Suzuki stages 2 and 4 moyamoya patients also showed higher incidences of rebuild-up phenomenon with 10 patients (71.4 %) in each stage showing the phenomenon. However, in the earliest stage (Suzuki stage 1) and severely advanced stage (Suzuki stage 5), the rate of rebuild-up was significantly lower (33.4 % in stage 1 and 40 % in stage 5) than the average incidence (70.5 %) of all 95 patients. Table 1 shows the summary of data from EEG, clinical findings, angiography, SPECT, and perfusion MRI in 82 patients who showed the rebuild-up phenomenon. Localized or asymmetric rebuild-up was observed in 62 of the 82 patients. Comparing the SPECT, the location of the rebuild-up distribution of EEG was more consistent with the area showing hemodynamic abnormalities on perfusion MRI (kappa value 0.711, p < 0.01).
Table 1 The summary of data from EEG, clinical findings, angiography, SPECT, and perfusion MRI in 82 patients who showed rebuild-up -
2.
Spike or sharp wave discharge
Spike or sharp wave discharges appeared in four patients (3.1 %), but none of these had clinical seizure attacks. In three patients, the spike discharges were activated by sleep and localized over the rolandic area. The other patient with frequent left occipital spike discharges had an acute major infarction in the corresponding region on MRI.
Postoperative EEG and clinical outcome
Of the 41 patients who underwent postoperative follow-up EEG, four patients (9.8 %) showed abnormalities in background activity. Asymmetric posterior alpha rhythm was observed in two patients, localized slow waves were observed in one patient, and abnormal low amplitude pattern was observed in the other patient. Spike discharges were observed in two patients, but none of them had clinical seizures up to the last follow-up.
Rebuild-up remained postoperatively in only six (14.6 %) patients. Among the 41 patients, postoperative clinical outcomes of the 35 patients without the rebuild-up phenomenon were excellent in 23, good in two, fair in eight, and poor in two patients. The outcomes of the six patients with remaining rebuild-up were excellent in two patients, good in none, fair in three patients, and poor in one patient. Table 2 summarizes the clinical data in the six patients who showed remaining rebuild-up after revascularization surgery. Four of the six patients who had remaining rebuild-up on follow-up EEG records showed TIA or medically intractable severe headache postoperatively even though they showed fair revascularization in postoperative follow-up angiography.
The serial follow-up EEG records of case 1 are presented in Fig. 2 as an illustrative case. This nine-year-old girl with unilateral moyamoya disease in the left hemisphere had recurrent motor TIA after hyperventilation, which almost disappeared after the first indirect bypass surgery. However, she started to complain of morning headache 4 months after the first operation. Her follow-up EEG record at that time revealed remaining rebuild-up mainly in left posterior head region. At 6 months after the surgery, the headache had become worse with recurrent motor TIA. Acetazolamide stress SPECT showed preserved rCVR and postoperative MR angiography was equivocal but TTP delay was observed in the follow-up perfusion MRI. Moreover, the degree of rebuild-up in EEG had become more prominent than in the previous study. Then we decided to perform the additional posterior revascularization operation on the same hemisphere. After the second operation her symptoms completely disappeared.
Discussion
Moyamoya disease is the most common pediatric cerebrovascular disorder in East Asia, especially Korea and Japan [1, 12, 28]. Since the surgical revascularization was widely accepted as a successful treatment [4, 6, 7, 11, 13, 19], the prompt diagnosis and proper evaluation has become more important to improve the long-term clinical outcome of the patients with moyamoya disease. Although conventional angiography is still the gold standard for the diagnosis of moyamoya disease, it has relative limitations as a repeat and follow-up modality because of its invasive nature and possible complications, especially in pediatric moyamoya patients. Therefore, MRI, magnetic resonance angiography, perfusion MRI, and SPECT have been accepted as useful modalities for noninvasively diagnosing and evaluating the determination of clinical severity and hemodynamic status in pediatric moyamoya patients [5, 14, 21, 24, 25, 29].
Although EEG in pediatric moyamoya disease also has characteristic findings [15], there have been few recent reports of the EEG features of moyamoya disease because it is nowadays regarded as having little clinical value. Because this study provides a comprehensive review of the EEG characteristics of a large series of pediatric moyamoya patients, it can shed new light on the clinical value of EEG as a diagnostic and postoperative follow-up modality.
The typical rebuild-up phenomenon was observed in two-thirds of the patients in this study. This total incidence of rebuild-up is similar to the results of a previous study [15]. We observed a significant correlation between age and the changes with hyperventilation. The changes in degree of build-up with advancing age in normal children have been considered to be related to the age difference in the decrease of cerebral blood flow and the threshold for EEG slowing in response to changes of cerebral blood flow [30]. Considering the significant concordance between rebuild-up and build-up (kappa value 0.681, p < 0.01) in our study, we suggest that the rebuild-up phenomenon also has considerable correlation with the change in cerebral blood flow. Although the mechanism of rebuild-up is not yet completely understood, previous reports [8, 15, 18, 26] have suggested that rebuild-up results from the decreased cerebral perfusion reserve associated with disturbance of cerebrovascular reactivity and the regional cerebral hypoxia followed by disturbance of oxygen metabolism. Further studies are necessary to clarify this phenomenon.
According to our study, the appearance of rebuild-up also showed a close correlation with the degree of disease progression. Considering that the Suzuki stage has a close correlation with the development of collateral vessels, it is thought that the delayed response of vascular reactivity and relatively decreased cerebral blood flow in the collateral vessels generates the characteristic delayed EEG slowing after cessation of hyperventilation in children with moyamoya disease. This seems to be similar to the mechanism of acetazolamide stress brain SPECT. The comparable distribution of the area showing hemodynamic abnormalities between SPECT, perfusion MRI, and the localized rebuild-up in EEGs strongly supports our hypothesis. We have experienced some patients with long-standing motor TIA after using acetazolamide for stress SPECT. In this case, hyperventilation EEG can be used as an alternative tool to evaluate the cerebral vascular reserve without causing significant neurologic deficits because we can simply ask the patient to stop hyperventilation if neurological symptoms occur.
As for the background activity, several typical cases showing posterior slow waves or centro-temporal slow waves were uncovered by careful review of our 127 EEG records but the incidence was relatively low compared with the previous report [15]. In our study, nonspecific localized or generalized slow waves and asymmetric posterior alpha rhythms were more common features of abnormal background activity. Considering that the patients with evidence of acute infarction on MRI (N = 8) showed a relatively high incidence of fixed regional slow waves (N = 6, 75 %), it is thought that the slow waves and asymmetry of background activities in moyamoya disease reflect secondary cerebral parenchymal changes such as infarction or atrophy rather than the characteristics of the disease itself. Paroxysmal activities such as spike or sharp wave discharges were not common in moyamoya EEGs (N = 4, 3.1 %). Moreover, the spike discharges of three patients were rolandic spike discharges that were not thought to be related to moyamoya disease. None of the four patients who showed spike discharges on EEG had experienced clinical seizures before or after the revascularization surgery. Consequently, the spike and sharp wave discharges might not be characteristic of moyamoya disease as were the abnormalities of background activity.
As progressive vascular narrowing and recurrent ischemic insults occur in moyamoya disease, careful follow-up after revascularization surgery is very important for improving the long-term outcome [2]. However, in some clinical situations, it is not easy to evaluate accurately the improvement of cerebral perfusion and hemodynamic change after surgical intervention. Although SPECT and perfusion MRI are valuable follow-up modalities for assessing cerebral perfusion and the outcome after revascularization surgery [14, 21, 31], we have often encountered a discrepancy between the clinical outcome and image findings like previous illustrative case. Kim and colleagues [10] have previously suggested that the postoperative EEG records with effective hyperventilation can be a good clinical follow-up tool in pediatric moyamoya disease. Although our study is limited in analyzing less than 50 % of postoperative EEGs among 127 patients even without intention and having potential bias that patients with poor postoperative outcome tended to return to better clinical follow-up and further study, our results of 41 follow-up EEGs after surgical intervention demonstrated that the EEG can be used as a helpful follow-up modality for clinical evaluation in pediatric moyamoya patients. In some patients like the illustrative case 1, EEG changes can be a strong supportive evidence of decreased functional vascular reservoir, closely correlated with the clinical symptoms, even though it seemed to be preserved in SPECT, perfusion MRI, and angiography. Based on this EEG finding, neurosurgeons decided to perform posterior vascular surgery. Good surgical outcome with symptom relief was observed as well as improvements in EEG findings.
Four of the six patients who had remaining rebuild-up in postoperative follow-up EEG showed unfavorable clinical outcomes regardless of the findings in SPECT and perfusion MRI (Table 2), though the correlation between remained EEG rebuild up and clinical outcomes were not statistically significant (p = 0.069) due to small sample size. We plan to continue further prospective study to verify these results.
Recently, an interesting study was published by Vendrame et al. [27], where they described their expereince with intraoperative EEG monitoring in moyamoya surgery and a technically feasible method to monitor ischemic changes during the operation. Althogh their results could not reveal EEG as a predictive value for intraoperative ischemic changes, they also suggested the potential clinical utility of bedside intraoperative EEG monitoring as an adjunctive tool in moyamoya disease.
In our study, significant complications including motor TIA were not observed during and after hyperventilation EEG recording before surgical revascularization. Although some authors regard moyamoya disease as a contraindication for hyperventilation during routine EEG recording [3], we carefully suggest that the EEG recording with hyperventilation in a moyamoya patient is a relatively safe and valuable test. However, the hyperventilation should be induced under close and careful supervision of an experienced examiner and should be stopped immediately when the patient experiences any clinical symptoms.
In summary, our study showed that prolonged build-up and rebuild-up with the hyperventilation are characteristic EEG changes in moyamoya disease especially in children, which is well correlated with the previously proven image modality to evaluate the vascular reserve. Although comparing MR perfusion, SPECT and angiography are the standard diagnostic modalities in moyamoya disease and most centers do not advocate hyperventilation, hyperventilation EEG can be used as an excellent supportive proof in some clinical situations since it is well correlated with the clinical symptoms in moyamoya disease patients. Additional experiences in hyperventilation EEG may be useful if done with appropriate precautions.
Conclusively, we reappraise noninvasive EEG as a relatively easy, safe, and valuable adjunctive modality for the diagnosis and postoperative evaluation of hemodynamic and clinical outcomes in pediatric moyamoya disease.
References
Baba T, Houkin K, Kuroda S (2008) Novel epidemiological features of moyamoya disease. J Neurol Neurosurg Psychiatry 79(8):900–904
Caldarelli M, Di Rocco C, Gaglini P (2001) Surgical treatment of moyamoya disease in pediatric age. J Neurosurg Sci 45(2):83
Fisch BJ (1999) Fisch and Spehlmann's EEG primer: basic principles of digital and analog EEG. Elsevier, New York
Goda M, Isono M, Ishii K, Kamida T, Abe T, Kobayashi H (2004) Long-term effects of indirect bypass surgery on collateral vessel formation in pediatric moyamoya disease. Journal of Neurosurgery: Pediatrics 100(2):156–162
Houkin K, Aoki T, Takahashi A, Abe H (1994) Diagnosis of moyamoya disease with magnetic resonance angiography. Stroke 25(11):2159–2164
Houkin K, Kuroda S, Nakayama N (2001) Cerebral revascularization for moyamoya disease in children. Neurosurgery Clinics of North America 12(3):575
Ishikawa T, Houkin K, Kamiyama H, Abe H (1997) Effects of surgical revascularization on outcome of patients with pediatric moyamoya disease. Stroke 28(6):1170–1173
Kameyama M, Shirane R, Tsurumi Y, Takahashi A, Fujiwara S, Suzuki J, Ito M, Ido T (1986) Evaluation of cerebral blood flow and metabolism in childhood moyamoya disease: an investigation into “re-build-up” on EEG by positron CT. Child's Nervous System 2(3):130–133
Kim CY, Wang KC, Kim SK, Chung YN, Kim HS, Cho BK (2003) Encephaloduroarteriosynangiosis with bifrontal encephalogaleo (periosteal) synangiosis in the pediatric moyamoya disease: the surgical technique and its outcomes. Child's Nervous System 19(5):316–324
Kim DS, Ko TS, Ra YS, Choi CG (2006) Postoperative electroencephalogram for follow up of pediatric moyamoya disease. J Korean Med Sci 21(3):495–499
Kim SK, Seol HJ, Cho BK, Hwang YS, Lee DS, Wang KC (2004) Moyamoya disease among young patients: its aggressive clinical course and the role of active surgical treatment. Neurosurgery 54(4):840
Kim SK, Wang KC, Kim DG, Paek SH, Chung HT, Hee M, Ahn Y, Cho BK (2000) Clinical feature and outcome of pediatric cerebrovascular disease: a neurosurgical series. Childs Nerv Syst 16(7):421–428
Kim SK, Wang KC, Kim IO, Lee DS, Cho BK (2002) Combined encephaloduroarteriosynangiosis and bifrontal encephalogaleo (periosteal) synangiosis in pediatric moyamoya disease. Neurosurgery 50(1):88–96
Kim SK, Wang KC, Oh CW, Kim IO, Lee DS, Song IC, Cho BK (2003) Evaluation of cerebral hemodynamics with perfusion MRI in childhood moyamoya disease. Pediatr Neurosurg 38(2):68–75
Kodama N, Aoki Y, Hiraga H, Wada T, Suzuki J (1979) Electroencephalographic findings in children with moyamoya disease. Arch Neurol 36(1):16
Kurlemann G, Fahrendorf G, Krings W, Sciuk J, Palm D (1992) Characteristic EEG findings in childhood moyamoya syndrome. Neurosurg Rev 15(1):57–60
Kuroda S, Houkin K (2008) Moyamoya disease: current concepts and future perspectives. Lancet Neurol 7(11):1056–1066
Kuroda S, Kamiyama H, Isobe M, Houkin K, Abe H, Mitsumori K (1995) Cerebral hemodynamics and “re-build-up” phenomenon on electroencephalogram in children with moyamoya disease. Child's Nervous System 11(4):214–219
Mesiwala AH, Sviri G, Fatemi N, Britz GW, Newell DW (2008) Long-term outcome of superficial temporal artery–middle cerebral artery bypass for patients with moyamoya disease in the US. Neurosurg Focus 24(2):E15
Scott RM, Smith ER (2009) Moyamoya disease and moyamoya syndrome. N Engl J Med 360(12):1226–1237
So Y, Lee HY, Kim SK, Lee JS, Wang KC, Cho BK, Kang E, Lee DS (2005) Prediction of the clinical outcome of pediatric moyamoya disease with postoperative basal/acetazolamide stress brain perfusion SPECT after revascularization surgery. Stroke 36(7):1485–1489
Sunder T, Erwin C, Dubois P (1980) Hyperventilation induced abnormalities in the electroencephalogram of children with moyamoya disease. Electroencephalogr Clin Neurophysiol 49(3):414–420
Suzuki J, Takaku A (1969) Cerebrovascular "moyamoya" disease: disease showing abnormal net-like vessels in base of brain. Arch Neurol 20(3):288
Togao O, Mihara F, Yoshiura T, Tanaka A, Noguchi T, Kuwabara Y, Kaneko K, Matsushima T, Honda H (2006) Cerebral hemodynamics in moyamoya disease: correlation between perfusion-weighted MR imaging and cerebral angiography. Am J Neuroradiol 27(2):391–397
Touho H, Karasawa J, Ohnishi H (1996) Preoperative and postoperative evaluation of cerebral perfusion and vasodilatory capacity with 99mTc-HMPAO SPECT and acetazolamide in childhood moyamoya disease. Stroke 27(2):282–289
Touho H, Karasawa J, Shishido H, Morisako T, Yamada K, Nagai S, Shibamoto K (1990) Mechanism of the re-buildup phenomenon in moyamoya disease—analysis of local cerebral hemodynamics with intra-arterial digital subtraction angiography. Neurol Med Chir 30(10):721
Vendrame M, Kalelyias J, Loddenkemper T, Smith E, Rockoff M, Manganaro S, McKenzie B, Gao L, Scott M, Bourgeois B, Kothare S (2011) Encephalogram monitoring during intracranial surgery for moyamoya disease. Pediatr Neurol 44:427–432
Wakai K, Tamakoshi A, Ikezaki K, Fukui M, Kawamura T, Aoki R, Kojima M, Lin Y, Ohno Y (1997) Epidemiological features of moyamoya disease in Japan: findings from a nationwide survey. Clin Neurol Neurosurg 99:S1–S5
Yamada I, Suzuki S, Matsushima Y (1995) Moyamoya disease: diagnostic accuracy of MRI. Neuroradiology 37(5):356–361
Yamatani M, Konishi T, Murakami M, Okuda T (1994) Hyperventilation activation on EEG recording in childhood. Epilepsia 35(6):1199–1203
Yun TJ, Cheon JE, Na DG, Kim WS, Kim IO, Chang KH, Yeon KM, Song IC, Wang KC (2009) Childhood moyamoya disease: quantitative evaluation of perfusion MR imaging—correlation with clinical outcome after revascularization surgery1. Radiology 251(1):216–223
Acknowledgments
This study was supported by a grant of the Korean Health Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (A120099).
We would like to thank Jae So Cho for English revision of this article.
Conflict of interest
The authors declared no potential conflicts of interests with respect to the authorship and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Jong-Hee Chae: Equally contributed and first author of the study.
Rights and permissions
About this article
Cite this article
Cho, A., Chae, JH., Kim, H.M. et al. Electroencephalography in pediatric moyamoya disease: reappraisal of clinical value. Childs Nerv Syst 30, 449–459 (2014). https://doi.org/10.1007/s00381-013-2215-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-013-2215-4