Abstract
Purpose
In our series of endoscopic third ventriculostomy (ETV), we sought to establish the relationship between the preoperative prediction using the Endoscopic Third Ventriculostomy Success Score (ETVSS) and the postsurgical success rate.
Materials and methods
This descriptive analytical study comprised 50 pediatric patients who underwent 58 ETV procedures between 2003 and 2011. Data regarding clinical, surgical, and radiological findings were obtained from a continuously updated database. For each patient, we calculated the ETVSS, based on the patient’s age, hydrocephalus etiology, and presence of a previous shunt. We considered success to be an established or improved clinical state and at least one of the following radiological criteria: (a) reduction in ventricular size or stable ventricles with disappearance of periventricular edema and increased subarachnoid space over cerebral convexities, (b) flow artifact in sagittal T2FSE MR, or (c) bidirectional flow signal in 2D-CPC MR. Statistical significance was set at p < 0.05. Six months was the minimum postoperative follow-up required.
Results
The ETV was successful in 29 patients (58 %). Patients aged over 1 year achieved the best results (p < 0.019). For those who underwent successful ETV, the mean ETVSS was 71.03 (95 % CI, 66.23–75.84). In those for whom the ETV was not successful, the mean ETVSS was 60 (95 % CI, 53.09–66.90); (p < 0.007).
Conclusions
The success of ETV in our series could have been predicted by ETVSS. Predictability could help establish stricter surgical selection criteria, thereby obtaining higher success rates, as well as preparing the patients and their families for expected outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Endoscopic third ventriculostomy (ETV) is an established treatment for hydrocephalus and is currently the procedure of choice for treatment of non-communicating hydrocephalus [9, 11, 13, 36]. However, controversy exists over which patients are appropriate candidates for the procedure [20, 23], and the selection of candidates for ETV affects its overall success rate [5, 11, 26].
Different systems for predicting results have been developed, among which is the Endoscopic Third Ventriculostomy Success Score (ETVSS), which is based on age, etiology of the hydrocephalus, and the presence of a previous shunt [24]. The varying results for neuroendoscopy may also be explained by the different postoperative criteria used to evaluate success [5, 26]. We recently proposed a system for classifying success grades for neuroendoscopic procedures to assess the type of success depending on clinical and radiological data [35]. The purpose of this study was to determine whether there existed a relation between the preoperative ETVSS prediction and the postsurgical success rate in our series of ETV.
Materials and methods
Between July 2003 and July 2011, 50 pediatric patients underwent 58 ETV procedures at the Pediatric Neurosurgery Service, Carlos Haya University Hospital, Málaga, Spain. All the surgical procedures were performed under general anesthesia by the same neurosurgical team. The ETVs were performed through a standard frontal burr hole with a rigid endoscope, inserting it into the lateral ventricle and entering the foramen of Monro. Mammillary bodies, the infundibular recess, the thalamostriate and septal veins, and the choroid plexus were identified in the floor of the third ventricle. The fenestration site was the floor of the third ventricle, halfway between the mammillary bodies and the infundibular recess, enlarged by using a 3- or 4-F Fogarty catheter. Fenestration of the Liliequist membrane, when present, was ensured with the aid of the Fogarty catheter.
Data regarding the age, sex, age at ETV, etiology of the hydrocephalus, previous shunt and shunt infection, admission symptoms, and surgical procedures performed were retrospectively reviewed. Table 1 shows the characteristics of the 50 patients.
The clinical symptoms were classified in two categories according to the time of development: acute and subacute symptoms (lasting less than 1 month), e.g., headache, nausea, and vomiting, and chronic symptoms (lasting more than 1 month), e.g., headache, progressive head enlargement, scoliosis, and gait or sphincter disturbances. Of the 50 patients, 25 had previously received a shunt, six of whom had a shunt infection. Table 2 shows the ETV procedure performed, either alone in 36 patients or plus another endoscopic maneuver in 14 patients. The seven surgical complications experienced were one pontine infarct followed by mild hemiparesis, two subdural hygromas, one unilateral third cranial nerve palsy, and three cerebrospinal fluid (CSF) fistula followed by meningitis. No mortality was seen following ETV.
For each patient in the cohort, we calculated the ETVSS [24] retrospectively, based on the patient’s age, etiology of the hydrocephalus, and the presence of a previous shunt. Success was considered to be the same or an improved clinical status as compared with the baseline preoperative status, plus at least one of the following radiological criteria [35]: (a) reduction in ventricular size or stable ventricles with disappearance of periventricular edema and increased subarachnoid space over cerebral convexities, (b) flow artifact in sagittal T2FSE MR, or (c) bidirectional flow signal in 2D-CPC MR. The minimum postoperative follow-up required was 6 months. Failure could be established immediately, with no requirement for any follow-up time.
The ETV success rate was related to age, sex, etiology, previous shunt, shunt infection, and number of maneuvers in each endoscopic procedure. We also examined whether the ETV success rate was predictable by the ETVSS. Lastly, we analyzed the relation between success and the learning curve, comparing the success rate in the first 4 years (2003–2007) with the success rate in the second 4 years (2007–2011).
In eight cases, a repeat ETV procedure was registered after a failure of the first ETV and the results were analyzed separately. No surgical complications were recorded in these eight repeat procedures.
The statistical analysis was performed using SPSS for Windows. The variables were subjected to a descriptive and comparative analysis through the Chi-square test for qualitative variables, the Student’s t test for quantitative and qualitative variables, and nonparametric Spearman’s rank correlation for quantitative variables. Statistical significance was set at p < 0.05.
Results
Endoscopic third ventriculostomy was successful in 29 of the 50 patients (58 %), with a mean follow-up of 33.92 months (range 6–92). Age was the only factor statistically related to a successful ETV. After distributing the patients in five ETVSS age groups (<1 month; 1 to <6 months; 6 months to <1 year; 1 to <10 years, and 10 or more years), we found that success was associated with an age of over 1 year (p < 0.019). No success was achieved in any of the five patients who were younger than 6 months (all failures).
The highest success rates were achieved in those cases of hydrocephalus caused by arachnoid cysts (85.7 %) or tumors (70 %) and the lowest in patients with slit ventricle syndrome (33 %). The success rate for nontumor aqueductal stenosis was 45.5 %. A previous shunt and shunt infection were not significantly correlated with success. The success rate for those with acute/subacute symptoms on admission was 60.0 %, and for those with chronic hydrocephalus, it was 53.3 % (p, not significant). The success rate of ETV when it was the sole surgical maneuver was 62.9 %, and that of ETV plus another maneuver was 46.7 % (p = 0.08); the lack of significance is probably because of the small sample, as the contingency table described a relation of success in >50 % of the ETV and in <50 % of the ETV plus another maneuver (Table 3).
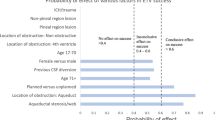
For the group that experienced success, the mean ETVSS prior to surgery was 71.03, variance (\( \overline \sigma \)) 12.63 (95 % CI, 66.23–75.84). The mean ETVSS in the group that did not experience success was 60, variance (\( \overline \sigma \)) 15.16 (95 % CI, 53.09–66.90). The confidence intervals hardly overlapped, and the result was a significant correlation (p < 0.007) (Fig. 2).
The ETVSS for the patients during the first period (2003–2007) was 62.8 (SD, 16.46) and that of the second period (2003–2007) was 70.0 (SD, 11.9), probably indicating a modification in stricter inclusion criteria with time. In the first period, the success rate for ETV was 12 patients (48 %), and in the second period (2007–2011), it rose to 17 patients (68 %), (p = 0.08).
A repeat ETV was performed after an initially unsuccessful procedure in eight patients. The follow-up period after endoscopy in these patients ranged between 13 and 62 months (mean 35.5 months). In these repeat procedures, ETV alone was performed in six patients, while in two, it was combined with another maneuver (ETV + septostomy + fourth ventricle opening in one patient, and in the other ETV + neuroendoscopic foraminal plasty of Monro). The mean ETVSS in these eight patients before the repeat ETV was 70. The repeat ETV was successful in seven of the eight. No complications were recorded in these eight repeat procedures. No statistical analysis could be performed in this group due to the small number of patients.
Discussion
Endoscopic third ventricle ventriculostomy is a minimally invasive procedure that has been used routinely in our department since 2003. It is an established treatment for hydrocephalus, especially since there is no need to place a foreign body such as a ventricular shunt, with its associated possibility of shunt malfunction and/or shunt overdrainage [29, 34]. Controversy persists over the selection of candidates for ETV, which affects the overall success rate of the procedure [9, 11, 23, 31]. Our success rate (58 %) was in line with overall success rates reported, such as about 56 % by Gangemi [17], 59 % by Kulkarni [25], and 78 % by Kadrian [20]. Nevertheless, low complication rates have also been described [13].
It is important to define the success of ETV from both the clinical and the radiological viewpoints [2, 6, 15, 18, 35]. A basic classification of degrees of success, such as that proposed in our previous work [35], has been suggested before [22], with the emergent need of a common classification to predict and evaluate success to improve neurosurgical practice.
Some efforts have been developed to predict success, and a predicting score has been proposed based on age, etiology, and a previous shunt [24]. Age seems to be the main factor influencing outcome in pediatric patients undergoing an ETV, with younger patients having a poorer success rate, though the minimum age to attempt ETV is still questioned. The age limitation in previous studies has become gradually lower, from 2 years [16] down to 6 months [14], given the effectiveness of this procedure and the importance of shunt independency. ETV had a significantly worse outcome as a function of age [18, 19, 23, 31], with younger, particularly neonate patients faring worse (Fig. 1) [11, 20, 30, 37].
These worse outcomes in younger patients have been associated with the physiology of CSF, along with the maturation of the subarachnoid space [21, 33], and with the developmental process of the major CSF pathway during infancy after the neonatal period [33]. Ventriculoperitoneal shunting is a favorable option in the age group under 6 months, rather than ETV [27], postponing ETV for older patients when success is more likely [10]. Nevertheless, ETV can still be considered as an alternative to shunt revision for cases previously shunted in the first year of life and that present malfunction [3, 7, 19]. Other authors have reported success rates of 34.8 % [32] or 67 % for ETV in neonates under 6 months of age [14], concluding that the factor influencing success was the specific etiology of the hydrocephalus [4, 6, 14]. According to our results, we cannot recommend ETV as a first choice for treatment under 1 year of age. As our figures show, no success was achieved in patients younger than 6 months (Fig. 1), with patients aged over 1 year achieving the best results (p < 0.019).
The etiology also influences ETV success; in fact, the highest success rates were achieved in cases of hydrocephalus caused by arachnoid cysts (85.7 %) or tumors (70 %) and the lowest in slit ventricle syndrome (33 %) [34]. The success rate for nontumor aqueductal stenosis in our series was 45.5 %, which is lower than the 60–94 % in other reports [20, 30], probably because 50 % of the children in our series were under 1 year of age. A previous shunt has been related with better outcomes after ETV [36], but not all authors agree [24]. We did not find that any particular etiology or the coexistence of a previous shunt worsened the prognosis significantly.
Although the ETVSS was initially designed to predict success rates in ETV procedures performed in acute hydrocephalus, we have applied this score in both acute/subacute and chronic hydrocephalus, due to nonsignificant differences regarding success. In addition, we were unable to demonstrate that a second maneuver, such as a tumor biopsy, worsens the probability of success in ETV (p > 0.05). However, there may be a bias here as our study had a limited number of patients, and the results could become significant by increasing the sample size. Nonetheless, a second maneuver would entail a more complex underlying pathology, which could also worsen the prognosis for the outcome in these patients (Fig. 2) [1, 8].
We found a significant correlation (p < 0.007) between the predicted success score and postoperative success, not just in acute/subacute hydrocephalus, but also in chronic hydrocephalus. Similar results were reported in recent validation studies for this success score, which suggest the ability of ETVSS to discriminate failure from success [12, 25, 28]. We also noted a significantly increased success with an increased ETVSS, with the scale showing most reliability above 66.23 (or in percentage terms, 73.58 %), a similar situation to that reported by others, who suggest that success prediction with ETVSS ≤70 is overestimated [28].
Our results have changed over time. In the first period (2003–2007), the success rate in ETVs was 48 %, and in the second period (2007–2011), it rose to 68 %. Though the difference was not significant (p = 0.08), it was nevertheless notable and probably related to the stricter inclusion criteria for these patients (e.g., not including any patient <6 months of age in the second period).
A success rate of 87 % was obtained in the patients who underwent a second ventriculostomy. No worthwhile statistical analysis could be done due to the limited sample size, and we recommend further studies related to the results in repeat ETV.
The low morbidity associated with ETV balanced against the lifetime risk of ventriculoperitoneal shunting remains a convincing argument in favor of a trial of ETV in pediatric patients over 1 year of age. Even so, the results to date offer rates of success and morbidity that could be introduced into the informed consent process [10].
Conclusion
We highlight the importance of the prediction of success. Better results are obtained performing ETV procedures in selected patients. In a significant percentage of cases (p < 0.007), ETV was successful in those patients with a higher ETVSS, with most reliability being found in those with an ETVSS of 66.23 or over, and in children older than 1 year of age (p < 0.019). These findings could also help prepare the patients and their families for expected outcomes.
References
Al-Tamimi Yahia Z, Bhargava D, Surash S, Ramirez RE, Novegno F, Crimmins D, Tyagi AK, Chumas PD (2008) Endoscopic biopsy during third ventriculostomy in paediatric pineal region tumors. Childs Nerv Syst 24:1323–1326
Bargalló N, Olondo L, Garcia AI, Capurro S, Caral L, Rumia J (2005) Functional analysis of third ventriculostomy patency by quantification of CSF stroke volume by using cine phase-contrast MR imaging. Am J Neuroradiol 26:2514–2521
Bilginer B, Oguz KK, Akalan N (2009) Endoscopic third ventriculostomy for malfunction in previously shunted infants. Childs Nerv Syst 25:683–688
Buxton N, Macarthur D, Mallucci C, Punt J, Vloeberghs M (1998) Neuroendoscopic third ventriculostomy in patients less than 1 year old. Pediatr Neurosurg 29:73–76
Cinalli G (2006) Impact of neuroendoscopy on the treatment of pediatric hydrocephalus. Neurosurg Rev, vol 1, no. 1. http://www.wfns.org/principal_reviews2-1c.html
Cinalli G, Sainte-Rose C, Chumas P, Zerah M, Brunelle F, Lot G, Pierre-Khan A, Renier D (1999) Failure of third ventriculostomy in the treatment of acueductal stenosis in children. J Neurosurg 90:448–454
Cinalli G, Salazar C, Mallucci C, Yada JZ, Zerah M, Sainte-Rose C (1998) The role of endoscopic third ventriculostomy in the management of shunt malfunction. Neurosurgery 43:1323–1329
Depreitere B, Dasi N, Rutka J, Dirks P, Drake J (2007) Endoscopic biopsy for intraventricular tumors in children. J Neurosurg 106(5 Suppl):340–346
Di Rocco C, Massimi L, Tamburrini G (2006) Shunts vs endoscopic third ventriculostomy in infants: are there different types and/or complications? A review. Childs Nerv Syst 22:1573–1589
Drake JM (2007) Endoscopic third ventriculostomy in pediatric patients: the Canadian experience. Neurosurgery 60:881–886
Drake JM, Kulkarni AV, Kestle J (2009) Endoscopic third ventriculostomy versus ventriculoperitoneal shunt in pediatric patients: a decision analysis. Childs Nerv Syst 25:467–472
Durnford AJ, Kirkham FJ, Mathad N, Sparrow OC (2011) Endoscopic third ventriculostomy in the treatment of childhood hydrocephalus: validation of a success score that predicts long-term outcome. J Neurosurg Pediatr 8:489–493
Ersahin Y, Arslan D (2008) Complications of third ventriculostomy. Childs Nerv Syst 24:943–948
Faggin R, Bernardo A, Stieg P, Perilongo G, D’Avella D (2009) Hydrocephalus in infants less than six months of age: effectiveness of endoscopic third ventriculostomy. Eur J Pediatr Surg 19:216–219
Fischbein NJ, Ciricillo SF, Barr RM, McDermott M, Edwards MS, Geary S, Barkovich AJ (1998) Endoscopic third ventriculocisternostomy: MR assessment of patency with 2-D cine phase-contrast versus T2-weighted fast spin echo technique. Pediatr Neurosurg 28:70–78
Gallo P, Szathmari A, De Biasi S, Mottolese C (2010) Endoscopic third ventriculostomy in obstructive infantile hydrocephalus: remarks about the so-called “unsuccessful cases”. Pediatr Neurosurg 46:435–441
Gangemi M, Maiuri F, Naddeo M, Godano U, Mascari C, Broggi G, Ferroli P (2008) Endoscopic third ventriculostomy in idiopathic normal pressure hydrocephalus: an Italian multicenter study. Neurosurgery 63:62–69
Goumnerova LC, Frim DM (1997) Treatment of hydrocephalus with third ventriculocisternostomy: outcome and CSF flow patterns. Pediatr Neurosurg 27:149–152
Janelli A, Reea G, Di Rocco C (2005) CSF shunt removal in children with hydrocephalus. Acta Neurochir 147:503–507
Kadrian D, van Gelder J, Florida D, Jones R, Vonau M, Teo C, Stening W, Kwok B (2005) Long-term reliability of endoscopic third ventriculostomy. Neurosurgery 56:1271–1278
Koch D, Wagner W (2004) Endoscopic third ventriculostomy in infants of less than 1 year of age: which factors influence the outcome? Childs Nerv Syst 20:405–411
Kulkarni A, Drake JM, Armstrong D, Dirks P (2000) Imaging correlates of successful endoscopic third ventriculostomy. J Neurosurg 92:915–919
Kulkarni AV, Drake JM, Kestle JRW, Mallucci CL, Sgouros S, Constantini S (2009) Endoscopic third ventriculostomy in the treatment of childhood hydrocephalus. J Pediatr 155:254–259
Kulkarni AV, Drake JM, Kestle JRW, Mallucci CL, Sgouros S, Constantini S (2010) Predicting who will benefit from endoscopic third ventriculostomy compared with shunt insertion in childhood hydrocephlalus using the ETV Success Score. J Neurosurg Pediatr 6:310–315
Kulkarni AV, Riva-Cambrin J, Browd SR (2011) Use of the ETV Success Score to explain the variation in reported endoscopic third ventriculostomy success rates among published case series of childhood hydrocephalus. J Neurosurg Pediatr 7:143–146
Meling TR, Tiller C, Due-Tønnessen BJ, Egge PK, Frøslie KF, Lundar T, Helseth E (2007) Audits can improve neurosurgical practice—illustrated by endoscopic third ventriculostomy. Pediatr Neurosurg 43:482–487
Mohanty A, Bisqas A, Satish S, Vollmer D (2008) Efficacy of endoscopic third ventriculostomy in fourth ventricular outlet obstruction. Neurosurgery 63:905–913
Naftel RP, Reed GT, Kulkarni AV, Wellons JC (2011) Evaluating the Children’s Hospital of Alabama endoscopic third ventriculostomy experience using the Endoscopic Third Ventriculostomy Success Score: an external validation study. J Neurosurg Pediatr 8:494–501
O’Brien D, Javadpour M, Collins D, Spennato P, Mallucci CL (2005) Endoscopic third ventriculostomy: an outcome analysis of primary cases and procedures performed after ventriculoperitoneal shunt malfunction. J Neurosurg 103(5 Suppl):393–400
O’Brien DF, Seghedoni A, Collins DR, Hayhurst C, Mallucci CL (2006) Is there an indication for ETV in young infants in aetiologies other than isolated aqueduct stenosis? Childs Nerv Syst 22:1565–1572
Oertel JM, Baldauf J, Schroeder HW, Gaab MR (2009) Endoscopic options in children: experience with 134 procedures. J Neurosurg Pediatr 3:81–89
Ogiwara H, Dipatri AJ Jr, Alden TD, Bowman RM, Tomita T (2010) Endoscopic third ventriculostomy for obstructive hydrocephalus in children younger than 6 months of age. Childs Nerv Syst 26:343–347
Oi S, Di Rocco C (2006) Proposal of “evolution theory in cerebrospinal fluid dynamics” and minor pathway hydrocephalus in developing inmature brain. Childs Nerv Syst 22:662–669
Ray P, Jallo GI, Kim RYH, Kim BS, Wilson S, Kothbauer K, Abbott R (2005) Endoscopic third ventriculostomy for tumor related hydrocephalus in pediatric population. Neurosurg Focus 19:E8
Ros B, Romero L, Ibañez G, Iglesias S, Rius F, Pérez S, Arráez MA (2012) Success criteria in pediatric neuroendoscopic procedures. Proposal for classification and results after 67 operations. Childs Nerv Syst 28:691–697
Teo C, Jones R (1996) Management of hydrocephalus by endoscopic third ventriculostomy in patients with myelomeningocele. Pediatr Neurosurg 25:57–63
Wagner W, Koch D (2005) Mechanisms of failure afer endoscopic third ventriculostomy in young infants. J Neurosurg 103:43–49
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
García, L.G., López, B.R., Botella, G.I. et al. Endoscopic Third Ventriculostomy Success Score (ETVSS) predicting success in a series of 50 pediatric patients. Are the outcomes of our patients predictable?. Childs Nerv Syst 28, 1157–1162 (2012). https://doi.org/10.1007/s00381-012-1836-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-012-1836-3