Abstract
Objective
To evaluate the role of endoscopic cyst fenestration and endoscopic guided VP shunt insertion in multi-loculated hydrocephalus in children.
Method
A retrospective analysis was performed on 20 patients with multi-loculated hydrocephalus who underwent endoscopic cyst fenestration (ECF) alone or in combination with VP shunt revision or insertion between August 2014 and December 2016 with the extended follow-up period to December 2017.
Results
Thirty-one ECFs were performed: ECF alone, 10 operations in 8 cases, and 21 ECFs with shunt insertion in 12 cases. Eighteen of 20 patients required a VP shunt, 7 cases required multiple shunts. All patients with a previous shunt remained shunt dependent; and 6 cases with no prior shunt underwent endoscopic guided ventricular catheter insertion after ECF; only 2 cases did not require a shunt after ECF. The rate of repeated ECFs was 0.25 operations/year and the shunt revision rate was 0.11 operations/year. VP shunt or cystoperitoneal shunt without repeat ECF was used in 7 cases (35%). Mean duration between operations was 71 days in repeated ECF and 16 days in added-on shunt. The most common cause of re-operations was new formation of intraventricular fibrosis or compartmentalization causing ventricular catheter blockage.
Conclusion
Endoscopic cyst fenestration and endoscopic assisted VP shunt insertion minimize shunt complications in multi-loculated hydrocephalus. Shunt independence is unusual.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Multi-loculated hydrocephalus is a difficult problem in pediatric neurosurgery. It occurs because of intraventricular septations that are usually secondary to intraventricular hemorrhage (IVH), bacterial meningitis, or postoperative gliosis after a previous shunt operation. Multi-loculated hydrocephalus has been treated with a variety of operations, including open surgery, multiple or complex shunts, and insertion of multi-perforated ventricular catheters, with variable results, and there is no widely accepted surgical treatment.
Since the introduction of neuroendoscopes in the 1980s, endoscopic cyst fenestration (ECF) has become a common surgical option to treat intraventricular cysts, either alone or in combination with endoscopically assisted ventriculoperitoneal shunt (VPS) insertion.
In our center, multi-loculated hydrocephalus is common and is the most common disorder requiring neuroendoscopy. The purpose of this article is to evaluate the role of ECF and endoscopic assisted VPS insertion or revision in children with multi-loculated hydrocephalus.
Patients and methods
Study population
After approval was granted from the hospital ethics board, we reviewed the medical records of 20 patients with a diagnosis of complex hydrocephalus who had undergone ECF alone or ECF in combination with either shunt insertion or shunt revision during the period of August 2014–December 2016. The diagnosis of complex hydrocephalus was obtained mainly from the pre-operative radiological appearance (CT/MRI) that demonstrated loculated or multi-loculated hydrocephalus with septations in the ventricles and cisterns. Follow-up data were collected from outpatient clinic visits and with the extended follow-up period of each case to the end of December 2017.
Surgical treatment
All patients received intravenous antibiotic prophylaxis (fosfomycin or cefazolin) during anesthetic induction and continued for at least 24 h after surgery. Endoscopy was performed using rigid neuroendoscope (Minop system, Aesculap). Endoscope was inserted into lateral ventricles or ventricular compartments through variable approaches tailored to each patient’s CT/MRI findings. Continuous irrigation was obtained in all cases using warm Acetar solutionFootnote 1. Fenestration of as many compartments as possible was performed with a Bugbee wire, monopolar cautery, micro-scissors, and balloon Catheter (0.7 mm, Karl Storz). In most cases, an external ventricular drainage system was left in for 1–3 days to drain blood-stained CSF.
Postoperative follow-up
After discharge from the hospital, patients were scheduled to return to outpatient clinics within the first month, then at 3 or 6 months later for post-operative clinical and radiological (CT/MRI) surveillance according to the surgeons’ preference. At least 8 months follow-up was obtained in all cases with the mean duration of 26.3 months.
Statistical analysis
Statistical analysis was performed using SPSS software (standard version 20; SPSS, Inc.). Continuous variables were reported as the mean ± SD or median. Categorical variables were recorded using numbers and percentages. Categorical variables were compared using Fisher’s exact tests. A probability value of 0.05 was considered to be statistically significant.
Results
Twenty pediatric patients with multi-loculated hydrocephalus were identified; 13 were female and 7 were male ranging in age from 2 months to 11 years (mean 21.1 months). The most frequent clinical presentations were head enlargement in 7 (35%), signs of increased intracranial pressure in 4 (20%), shunt malfunction in 4 (20%), shunt infection in 3 (15%), incidental finding from surveillance imaging in 1 (5%), and seizure in 1 (5%) (Table 1). The duration of follow-up ranged from 8 to 41 months (mean 26.3 months). The repeat ECF rate was 0.25 operations/year, shunt revision rate without repeat fenestration was 0.11 operations/year, and the overall re-operations rate was 0.36 operations/year. Mean duration between operations was 71 days in repeated ECF and 16 days in added-on shunt (Table 2).
Complications of endoscopic approaches included two cases of transient subdural hematoma which were managed conservatively. One patient who had multiple ECF procedures died from severe brainstem dysfunction due to infratentorial compartmentalization.
Patients were divided into 2 groups according to whether or not a VP shunt was inserted prior to the ECF operation.
No pre-existing shunt group
In this group of 8 patients, post-infectious hydrocephalus was the most common etiology (4 patients), followed by intrauterine intraventricular hemorrhage in 2 patients, post-tumor resection, and post-encephalocele repair in 1 patient each. The mean follow-up duration in this group was 23.1 months (range 8–33 months, Table 3). Ten endoscopic fenestrations were performed in this group. Two children were treated with ECF only and required no VPS (Fig. 1), four were treated with ECF and a VPS but required no subsequent shunt operation, and two were treated with ECF and a VPS but required one subsequent shunt operation. Thus, six of the eight patients were shunt independent or had only one shunt with the ECF operation while two patient required repeated ECFs (25%) (Table 3). The rate of repeat ECFs was 0.13 operations/year as same as the rate of shunt revisions.
A 3-month-old girl with the history of antenatal hydrocephalus that required cesarean section due to macrocephaly presented with progressive macrocephaly and optic nerve atrophy. a, b, c Pre-operative MRI. c, d, e Two weeks post-ECF scan. Patient had remained well with no VP shunt required months after procedure. However, patient deceased from pneumonia and RDS 8 months after ECF procedure
VP shunt present prior ECF procedure
Twelve patients had 1–2 shunts before ECF. Their hydrocephalus was post-infectious in 7, post-IVH in 3, associated with a congenital brain anomaly in 3, and post-tumor resection in 1. In this group, 8 patients had multi-loculated hydrocephalus and 4 had shunt occlusion. Twenty-one cysts were fenestrated. Mean follow-up duration was 28.4 months (range 11–41 months, Table 4). At the end of the follow-up period, none of patients were shunt independent. Seven patients remained with a single shunt (Fig. 2) and five required additional shunts. (Table 4) Five patients (41%) required repeated endoscopic operations: three required one re-operation and two required three re-operations (Fig. 3). The rate of repeat ECFs with shunt revisions was 0.21 revisions/year and the rate of shunt revisions was 0.1 operations/year so the overall revisions rate was 0.31 revisions/year.
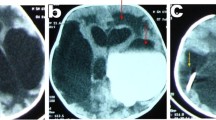
A 2-year-old girl with the history of maternal syphilis presented with progressive macrocephaly after VP shunt insertion and developmental delay. a, b Pre-ECF scan. c Six months post-ECF and endoscopic VP shunt scan. The ventricular catheter was placed under endoscopic guidance through all the compartments aiming to act as a stent. Patient does not require any procedure after this and remain well for the last 18 months
A 6-month-old girl with the history of GMIVH with hydrocephalus presented with VP shunt infection. a, b, c Pre-3rd ECF scan. d, e, f Immediate post-ECF and endoscopic rt. VP shunt insertion CT scan. The ventricular catheter was placed under endoscopic guidance aiming to act as stent and drain all compartments along also left the tip in quadrigeminal cyst. Patient required another ECF and VP shunt revision 6 months after this and the intra-operative view during the last endoscopic procedure showing in figure labels g, h, and i. Then she had remained well for the last 24 months. j, k, and l The most recent CT scan in March 2017 showing good functioning rt. VP shunt.
Discussion
Intraventricular septations develop secondarily from meningitis or ventriculitis, germinal matrix intraventricular hemorrhage, congenital brain anomalies and post-operative gliosis [1,2,3,4,5]. Predisposing factors include low birth weight, premature birth, perinatal complications, and congenital central nervous system malformations [4, 6]. However, post-infectious multi-loculated hydrocephalus may be the most difficult to treat [7]. El-Ghandour et al. reported 24 pediatric patients who were treated with multi-loculated hydrocephalus [8]. The etiologies of their cases were the same as for ours. Eshra reported 14 patients with septated/multi-loculated hydrocephalus who were treated with ECF and found that 11 patients required re-operations because of residual compartments that were not opened and drained by the existing shunts. Of those 11 patients with two ECF operations, only 3 needed an additional intra-cyst catheter insertion [9]. The higher rate of repeat ECFs was detected in our pre-existing shunt group; however, there is no statistically significant difference (41% vs. 25%, p = 0.642). This higher rate of repeat ECFs may be explained from postoperative gliosis or inadequate endoscopic fenestration on the previous attempt [10].
Multi-loculated hydrocephalus can be very difficult to manage. Apart from open surgery, insertion of additional shunt catheters was widely accepted as mainstay treatment prior to the increased use of endoscopy [3, 11, 12]. The goals of surgery in this disorder include control of hydrocephalus, simplification of complex shunts, reduction of shunt revisions, and decreased operative morbidity [5, 13]. The idea of insertion of multi-perforated ventricular catheters together with puncture of the membranes has been suggested, but has yielded inconsistent results [14]. In the 1980s, a 54% mortality rate was reported, with the remaining patients severely impaired [14]. Nida et al. and Lewis et al. reported a mean of 2.75 and 2.77 shunt revisions per year in their series respectively [11, 15]. The introduction of the neuroendoscope allowed fenestration of loculations with minimal invasion. The endoscope is an ideal instrument for exploration of intraventricular compartments. It is less invasive, has greater operative simplicity than microsurgery, and its use has become widely established in the treatment of multi-loculated hydrocephalus [16]. The three largest published series of patients treated for multi-loculated hydrocephalus using endoscopic techniques reported a notable reduction in the frequency of shunt revisions compared with that before surgery or compared with control patients treated without endoscopic fenestration [15,16,17,18]. In the most recent series, the shunt revision rate was 2.07 revisions per year before endoscopy and 0.35 revisions per year afterwards in the group with existing VPS [17] which is similar to our overall shunt revisions rate in the same group. From multiple series published previously, the overall success rate in control of hydrocephalus with a single shunt or no shunt ranged between 61 and 100% [17] similar to our 65% success. The wide range of success among centers might be explained by multiple factors including the complexity of cases, variety of endoscopic techniques, quality of visualization, and lack of advanced equipment such as stereotactic neuronavigation. Good results of craniotomy and microsurgical fenestration were reported in two series. [11, 13, 19] However, in the series of 33 patients, Sandberg et al. reported 47 repeat fenestration procedures (endoscopically or with craniotomy) were required in 19 patients that ranged from 1 to 6 each in the average follow-up duration of 3.7 years [19]. It has emphasized the fact that re-operations are not uncommon even when treated with craniotomy and microsurgical fenestration. In our opinion, the benefits of open surgery do not outweigh its well-known risks especially for young children less than 1 year old [13]. We found that multi-loculated hydrocephalus is a dynamic disorder. Opening of some loculations, often, is leading to discovery of more hidden loculations down the tract from hydrodynamic changes or new membrane formation. Thus the repeat ECFs are not always avoidable and it is considered to be the safest way possible to treat these patients [20]. Furthermore, Schulz et al. reported that Neuronavigator helps making every attempt more productive and precise, although re-operations or revisions are required often [21].
Finally, we have observed that those with multi-loculated hydrocephalus and multiple shunts frequently have complex cysts in posterior fossa or the tip of a pre-existing catheter is located in a difficult place such that revision might cause serious complications. From our experience, few posterior fossa cysts can be successfully treated with fenestration alone. Spontaneous closure is commonly detected soon after ECF, especially for those in the cerebellopontine angle. The most useful way to treat this condition may be with an endoscopic guided multi-perforated catheter which acts as a stent to drain multiple compartments. Caution should be exercised as the catheter may migrate into the brainstem later after insertion so clinical and imaging surveillance should be done cautiously and regularly. For cases with difficult location of a pre-existing catheter, such that a second catheter is needed, the use of a Neuronavigator and or intra-operative MRI may decrease the need of multiple shunts [21, 22].
Conclusion
Treatment of multi-loculated hydrocephalus is difficult. Endoscopic fenestration and endoscopic assisted VP shunt insertion are useful in reducing shunt complications and should be considered as a therapeutic option, although shunt independence is rare.
Notes
Acetar solution is an isotonic solution that contains Na 130 mEq/L, K 4 mEq/L, Cl 108.7 mEq/L, acetate 28 mEq/L, and osmolarity 273.4 mOsm/L. Acetate in this solution will be changed to bicarbonate in the muscle so it is widely used in patients with liver impairment.
References
Schultz P & Leeds NE (1973). Intraventricular septations complicating neonatal meningitis. J Neurosurg, 38, 5, (May 1973), pp. 620–626, ISSN 0022-3085
Eller TW & Pasternak JF (1985). Isolated ventricles following intraventricular hemorrhage. J Neurosurg, 62, 3, ( 1985), pp. 357–362, ISSN 0022-3085
Ling JM, Tiruchelvarayan R (2013) A review of endoscopic treatment of hydrocephalus in Paediatric and adult patients. Proceedings of Singapore Healthcare 22:203–212
Christian EA, Melamed EF, Peck E, Krieger MD, McComb JG (2016) Surgical management of hydrocephalus secondary to intraventricular hemorrhage in the preterm infant. J Neurosurg Pediatr 17:278–284
Spennato, Pietro & Cinalli, Giuseppe & Carannante, Giuseppe & Ruggiero, Claudio & Del Basso de Caro ML, . (2004). Multiloculated hydrocephalus chapter, pediatric hydrocephalus. Cinalli G, Maixner WJ, Sainte-Rose C (Ed.), https://doi.org/10.1007/978-88-470-2121-1_16
Albanese V, Tomasello F & Sampaolo S (1981). Multiloculated hydrocephalus in infants. Neurosurgery, 8, 6, (1981), pp. 641–646, ISSN 0148-396x
EL-Ghandour N (2013) Endoscopic cyst fenestration in the treatment of uniloculated hydrocephalus in children. J Neurosurg Pediatrics 11:402–409
EL-Ghandour N (2008) Endoscopic cyst fenestration in the treatment of multiloculated hydrocephalus in children. J Neurosurg Pediatrics 1:217–222
Eshra MA (2014) Endoscopic management of septated, multiloculated hydrocephalus. Alexandria Journal of Medicine 50:123–126
Cinalli G, Spennato P, Ruggiero C, Aliberti F, Trischitta V, Buonocore MC, Cianciulli E, Maggi G (2007) Complications following endoscopic intracranial procedures in children. Childs Nerv Syst 23:633–644
Nida TY, Haines SJ (1993) Multiloculated hydrocephalus: craniotomy and fenestration of intraventricular septations. J Neurosurg 78:70–76
David I (2008) Sandberg, endoscopic management of hydrocephalus in pediatric patients: a review of indications, techniques, and outcomes. J Child Neurol 23(5):550–560
El-Ghandour NMF (2012) Complex hydrocephalus, hydrocephalus. In: Pant S (ed). InTech. Available from: http://www.intechopen.com/books/hydrocephalus/complex-hydrocephalus. Accessed 28 Nov 2017
Kalsbeck JE, DeSousa AL, Kleiman MB, Goodman JM, Franken EA (1980) Compartmentalization of cerebral ventricles as a sequela of neonatal meningitis. J Neurosurg 52:547–552
Lewis AI, Keiper GL Jr, Crone KR (1995) Endoscopic treatment of loculated hydrocephalus. J Neurosurg 82:780–785
Tamburrini G, D’Angelo L, Paternoster G, Massimi L, Caldarelli M, Di Rocco C (2007) Endoscopic management of intra and paraventricular CSF cysts. Childs Nerv Syst 23:645–665
Spennato P, Cinalli G, Ruggiero C, Aliberti F, Trischitta V, Cianciulli E, Maggi G (2007) Neuroendoscopic treatment of multiloculated hydrocephalus in children. J Neurosurg (1 Suppl Pediatrics) 106:29–35
Nowoslawska E, Polis L, Kaniewska D, Mikolajczyk W, Krawczyk J, Szymanski W, Zakrzewski K, Podciechowska J (2003) Effectiveness of neuroendoscopic procedures in the treatment of complex compartmentalized hydrocephalus in children. Childs Nerv Syst 19(9):659–665
Sandberg DI, McComb G, Kreiger MD (2005) Craniotomy for fenestration of multiloculated hydrocephalus in pediatric patients. Neurosurgery 57(1 Suppl):100–106
Sikorski CW, Yamini B, Frim DM (2004) Endoscopic cyst fenestration outcomes in children one year of age or less. Pediatr Neurosurg 40:59–63
Schulz M, Bohner G, Knaus H, Haberl H, Thomale UW (2010) Navigated endoscopic surgery for multiloculated hydrocephalus in children. J Neurosurg Pediatrics 5:434–442
Paraskevopoulos D, Biyani N, Constantini S, Beni-Adani L (2011) Combined intraoperative magnetic resonance imaging and navigated neuroendoscopy in children with multicompartmental hydrocephalus and complex cysts: a feasibility study. J Neurosurg Pediatrics 8:279–288
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Piyachon, S., Wittayanakorn, N., Kittisangvara, L. et al. Treatment of multi-loculated hydrocephalus using endoscopic cyst fenestration and endoscopic guided VP shunt insertion. Childs Nerv Syst 35, 493–499 (2019). https://doi.org/10.1007/s00381-019-04047-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-019-04047-w