Abstract
After surgical correction of a craniosynostotic deformity, clinical follow-up and evaluation of the surgical result are mandatory like in any other surgical procedure. Both functional as well as cosmetic aspects lead to the indication for surgery and need to be addressed during follow-up assessments. In the past, cosmetic outcome was determined mainly by subjective evaluation. Parents, involved doctors, and sometimes patients themselves judged upon the surgical results without reproducible and objective tools.Single suture craniosynostosis Single suture craniosynostosis is mainly considered to be a cosmetic problem. Only in the recent past, functional aspects are getting into the focus in this patient group and respective clinical studies are gaining significance.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Introduction
After surgical correction of a craniosynostotic deformity, clinical follow-up and evaluation of the surgical result are mandatory like in any other surgical procedure. Both functional as well as cosmetic aspects lead to the indication for surgery and need to be addressed during follow-up assessments. In the past, cosmetic outcome was determined mainly by subjective evaluation. Parents, involved doctors, and sometimes patients themselves judged upon the surgical results without reproducible and objective tools. Single suture craniosynostosis is mainly considered to be a cosmetic problem. Only in the recent past, functional aspects are getting into the focus in this patient group and respective clinical studies are gaining significance. Syndromic craniosynostosis is causing a variety of functional problems due to microcephaly, micro-ophthalmic conditions, and consequences of the often associated midfacial hypoplasia. Functional assessment seems to be more objective compared to cosmetic evaluation, but both play an important role and are necessary for any therapeutic improvement in the future.
The cosmetic aspect gained increasing importance during recent years and accordingly there are a rising number of surgical indications in simple cases.
It is important to evaluate the cosmetic effect and the long-term development of morphometric head parameters of different surgical techniques in order to compare them with each other and to improve operative or adjuvant strategies. Since the introduction of minimal invasive endoscopic craniectomy and helmet therapy for the treatment of nonsyndromic craniosynostosis, the comparison of different techniques is of growing importance, not only in respect of the cosmetic results but also for the evaluation if the age of the affected child at time of intervention influences outcome and long-term results. In recent years also, developmental aspects attracted more attention.
Treatment Outcome and Prognosis
In principal, the direct influence of any surgical correction on the following skull development needs to be evaluated apart from the psychomotor development. So far no clear correlation could be found between surgical correction of a simple craniosynostosis and the child’s motoric and cognitive development. Syndromic conditions need to be evaluated separately due to the fact that in most cases relevant intracranial pressure elevations may occur early and some syndromes go along with cognitive dysfunctions due to primary brain defects (Kapp-Simon et al. 2007, 2012; Raybaud and Di Rocco 2007). Regarding long-term outcome after deformity correction, numerous publications can be found, partially basing on subjective criteria, partially on morphometric parameters. Different techniques or age at time of surgery are not always looked at specifically. Accordingly, no overall outcome evidence is available.
In order to evaluate outcome after correction of a sagittal or bicoronal synostosis, the assessment of the cephalic index (CI) is the standard outcome criterion. It is generally accepted to classify long-term correction of dolichocephalus in sagittal synostosis and of brachycephalus in bicoronal synostosis as successful, although brachycephalus in those cases, that most probably have a syndromic background, rarely completely resolves. Today in sagittal synostosis, normalization of dolichocephalus can be reached in 80–90%. The same results are seen in open and minimal invasive surgery series (Shah et al. 2011). Excellent and stable long-term results are found after fronto-orbital advancement with bifrontal cranioplasty in metopic synostosis. Careful outcome analysis in the past could demonstrate that such results are possible only after primary overcorrection of the bandeau advancement in order to compensate later growth inhibition in this area.
In asymmetric lesions such as anterior plagiocephaly, due to unilateral coronal synostosis, much less satisfactory results are observed, mainly, because part of the problem is the unaddressed facial scoliosis. Also the rare lambdoid synostosis has not a very favorable outcome since the affected skull base area cannot be corrected surgically in a direct way.
Reproducible morphometric parameters for the evaluation of symmetry that also includes the facial structures do not exist so far. The recent development of 3D stereoscopic measurement and visualization techniques have improved objective follow-up significantly (Martini et al. 2015). Although any cranioplastic correction is a significant surgical procedure with a relatively high blood loss, the related complication rate is very low, as soon as adequate blood transfusion is initiated in time and no intradural lesions occur. The only exceptions are monobloc distraction techniques (Dunaway et al. 2012). Complications with long-term follow-up relevance are therefore rare.
Regarding the psychomotor development of affected children, only few publications exist. Up to 10% of children with single suture craniosynostosis will show a more or less significant developmental delay. These data are mainly derived from scaphocephaly and trigonocephaly series. It is assumed that this is not necessarily related to the skull deformity itself but possibly caused by independent factors. In many cases, only minimal brain dysfunctions still in the range of normal intelligence are described. Trigonocephaly can be associated with syndromic conditions and other developmental pathologies influencing the overall intellectual, behavioral, and motoric development (Arnaud et al. 1995; Kapp-Simon et al. 1992, 2007, 2012; Mendonca et al. 2009).
In syndromic craniosynostoses, major psychomotor retardation can be found depending on the underlying subtype. Up to one-third of all untreated patients with craniosynostosis have an elevated intracranial pressure, which correlates in most cases with presence of a papilledema. After surgical correction of the skull deformity, papilledema and raised intracranial pressure still can be found, mostly after a latency of months up to years. The incidence varies depending on series and techniques. After single suture correction, the highest ratio of secondary papilledema up to 6% is found in patients with sagittal synostosis, even in cases with normalization of skull shape and volume. This compares with untreated series. In some syndromic cases, pre- as well as postoperative ICP increases are found even more frequently. In general, it is recommended to perform regular fundoscopy independent of prior surgery to rule out papilledema, which can be found in up to 20%, after the 6th month. An untreated papilledema can lead to irreversible visual decline. In single suture craniosynostoses, papilledema is much less frequent compared to syndromic cases (Dufier et al. 1986). Secondary papilledema can also be found even in cases with sufficient augmentation of the skull volume probably due to changes of the venous outflow, which can be primarily or secondary after bony changes caused by cranioplastic surgery (Martini et al. 2014). Additionally, an associated hydrocephalus or secondary Chiari malformation type 1 may contribute to elevated intracranial pressure levels and should be ruled out, whenever signs of raised ICP are found during follow-up. Papilledema can be observed in asymptomatic patients, and on the other hand, raised ICP can be present without papilledema. In these cases, headache is the predominant symptom and intracranial pressure monitoring, with open or telemetric techniques, must be discussed. Around 7–33% of all untreated patients with single suture craniosynostosis may develop an increased ICP (Gault et al. 1992; Hayward et al. 2015; Thompson et al. 1995).
The orbital structures can also be impaired in consequence of the bony anomalies which are part of the craniosynostotic deformities with involvement of the fronto-orbital region. Visual and refraction disorders, and, in severe cases exophthalmos, are resulting. Children with trigonocephaly and hypotelorism have a higher incidence to develop astigmatism (Macintosh et al. 2007, 2011).
Follow-up Criteria
Beside morphometric assessments like head circumference, head height, cephalic index (CI), and skull volume, subjective evaluation by parents, pediatricians, and later in the course by the patient him- or herself are used as well as photographic documentation. Further follow-up criteria are the overall shape of the skull, residual calvarian defects, and functional disorders of the naso-pharyngeal region, the inner ear, and the gnathic apparatus. Residual bony defects can be followed conservatively when they are very small and without round edges, indicating sclerosis with minor chance for spontaneous closure. Remaining defects can be covered using calvarian split graft or bone cement in small gaps. It is mandatory to fixate them sufficiently.
A major problem is the objective follow-up assessment of the overall skull shape.
Children with single suture craniosynostosis should be monitored at least once a year until the 10th birthday independently from prior cranioplastic surgery. The most important screening parameters are listed in Table 1.
In general, it is recommended to include children with single suture craniosynostosis into a craniofacial follow-up program until the age of 10 years, in complicated cases also for a longer period of time. Concomitant ophthalmological assessments with fundoscopy and visual or refraction tests are also necessary (Macintosh et al. 2007, 2011).
In syndromic cases, a minimal follow-up time until early adulthood must be recommended. The facial development will not be completed before the end of adolescence and functional disorders related to a deficient midfacial development may occur late. A staged treatment of gnathic and dentation problems throughout childhood and adolescence by orthodontist and maxilla-facial surgeon is often required.
Lower brainstem structures are at risk in patients with a major disproportion of skull and brain volume. Secondary Chiari malformation type 1 with downward displacement of cerebellar structures and a chronic elevated ICP can cause severe central apnea. Associated venous anomalies may also contribute to this condition. Additionally, concomitant upper airway restrictions can cause obstructive apnea leading to mostly combined severe sleep apnea pattern. Assisted breathing devices or even tracheostomy can be indicated. Regular polysomnography studies are indicated in syndromic cases with proven sleep apnea.
Additional functional ear and hearing tests are important as well, due to the fact, that the bony development of the inner ear structures may also be involved (see Table 2).
All children with a more or less significant craniosynostosis should be under developmental surveillance because of the fact that psychomotor and neurocognitive deficits may occur (Arnaud et al. 1995; Kapp-Simon et al. 1992, 2007, 2012; Raybaud and Di Rocco 2007).
It is important, that outcome assessment and follow-up, in particular in syndromic patients, is performed by an experienced team consisting of neurosurgeons, maxillo-facial surgeons, and neuropediatricians, as well as ENT and orthodontic experts.
Morphometric Assessment
In the past, morphological assessment during craniosynostosis follow-up was done by subjective evaluations or non-morphometric imaging (Arnaud et al. 1995; Haberl et al. 2004; Renier et al. 2000; Schaller et al. 2012). Whitaker et al. (1987) used the indication of a necessary second surgery as evaluation parameter (Whitaker et al. 1987). Also other authors used this criterion (Aryan et al. 2005; Breugem and van R. Zeeman 1999; Engel et al. 2012; Esparza et al. 2008; McCarthy et al. 1995a, b; Selber et al. 2008; Vinchon et al. 2012).
It was generally accepted to record skull growth and morphological features with photographs of the head taken from standardized perspectives (Haberl et al. 2004; Hilling et al. 2006a, b; van der Meulen 2012) and to perform classical anthropometric measurement by using measuring loops and tape measures (Farkas and Posnick 1992; Kolar and Salter 1997). Additionally, anthropometric methods in two- or three-dimensional radiographic images were also used (Frühwald et al. 2008; Marcus et al. 2008). All these techniques were not able to adequately depict the complex three-dimensional growth dynamics of the human viscero- and neurocranium.
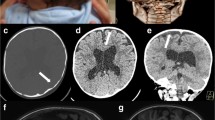
Recently, 3D-scan methods, 3D-photogrammetry, and stereo-photogrammetry gained importance for the assessment of skull volume and shape. Multiple photographic perspectives are fused and a virtual 3D image of the skull is formed (David et al. 2010). These techniques provide metric information and the excellent clinical applicability could have been shown. The calculated skull volumes basing on CT and photogrammetry images have been compared and a high correlation between the two methods has been found (McKay et al. 2010). Other authors could confirm these results (Schaaf et al. 2010a, b; Wong et al. 2008). Wilbrand et al. were the first who have been able to demonstrate three-dimensional changes of craniosynostotic deformities in children with the help of stereo-photogrammetry (Wilbrand et al. 2012). An example of a stereo-photogrammetry setting is given in (Fig. 1). A 3D surface scanner basing on laser technology is less time consuming and ideal in non-compliant children (Fig. 2).
Beside these new techniques, still the major morphological follow-up criterion is the development of the head circumference and the classification of the general head shape, in brachycephalic, normocephalic, and dolichocephalic skulls. This classification is based on the two-dimensional head shape which is derived from the cephalic index (CI). The CI is the ratio of the maximum width of the head multiplied by 100 divided by its maximum length in the horizontal plane (measured front to back). This measure is not only used in anthropology and human medicine but also for the categorization of animals. The CI has been defined by the Swedish anatomist Anders Retzius (1796–1860). The normal range is depending on the ethnical group the underlying values are derived from and significant variations exist across the globe. Differences also exist between male and female skulls. The overall accepted classification values are listed in Table 3.
A two-dimensional evaluation of the skull development during follow-up is not sufficient for the detection of additional deformities. Specific changes related to the height development and related to calvarian and facial symmetry in craniosynostoses are described by the morphological appearance. Typical features are oxycephalic, turricephalic, anterior or posterior plagiocephalic or using other descriptive terms, such as Kleeblattschädel (clover leaf skull). No objective measures, standard scales, or indices exist for three-dimensional deformities. Therefore, comparative surface scan models have been developed, demonstrating regional changes in shape of an individual postoperative course (Fig. 3).
Recently, a scan-basing 3D-model with new morphometric angle parameters has been established for clinical follow-up and assessment of form stability after fronto-orbital advancement (Martini et al. 2015) (Fig. 4).
Studies on asymmetric deformities in particular caused by unilateral coronal craniosynostosis can also be performed with modern scan techniques. Since metric measures can be obtained, objective data regarding changes during follow-up can be documented (Martini et al. 2015). Software programs help to calculate a variety of planes, angles, and other morphometric measures, like CI, head height, and skull volume, etc. by using predefined or newly established landmarks (Fig. 5).
Conclusion
The evaluation of outcome after craniosynostosis surgery remains complex and reproducible parameters are not well defined. On one side, this is related to the different pathologies and the interindividual clinical courses which are presented. In some of these patients, a specific genetic background or a different time of onset may be responsible for this phenomenon. On the other side, not many objective parameter and comparable data exist for the outcome assessment. It is important to follow children with craniosynostosis, independent from the kind of treatment, as long as possible to prevent them from possible late complications and to ensure an acceptable cosmetic outcome. An experienced maxillo-facial team and in syndromic cases, all additional disciplines, like sleep and ENT specialists, etc., are needed to guarantee adequate follow-up.
References
Arnaud E, Renier D, Marchac D (1995) Prognosis for mental function in scaphocephaly. J Neurosurg 83(3):476–479
Aryan HE, Jandial R, Ozgur BM, Hughes SA, Meltzer HS et al (2005) Surgical correction of metopic synostosis. Childs Nerv Syst 21(5):392–398
Breugem CC, van R. Zeeman BJ (1999) Retrospective study of nonsyndromic craniosynostosis treated over a 10-year period. J Craniofac Surg 10(2):140–143
David LR, Plikaitis CM, Couture D, Glazier SS, Argenta LC (2010) Outcome analysis of our first 75 spring-assisted surgeries for scaphocephaly. J Craniofac Surg 21(1):3–9
Dufier JL, Vinurel MC, Renier D, Marchac D (1986) Ophthalmologic complications of craniofacial stenoses. Apropos of 244 cases. J Fr Ophtalmologie 9(4):273–280
Dunaway DJ, Britto JA, Abela C, Evans RD, Jeelani NU (2012) Complications of frontofacial advancement. Childs Nerv Syst 28(9):1571–1576
Engel M, Thiele OC, Muhling J, Hoffmann J, Freier K et al (2012) Trigonocephaly: results after surgical correction of nonsyndromatic isolated metopic suture synostosis in 54 cases. J Craniomaxillofac Surg 40(4):347–353
Esparza J, Hinojosa J, Garcia-Recuero I, Romance A, Pascual B, Martinez de AA (2008) Surgical treatment of isolated and syndromic craniosynostosis. Results and complications in 283 consecutive cases. Neurocirugia (Astur) 19(6):509–529
Farkas LG, Posnick JC (1992) Growth and development of regional units in the head and face based on anthropometric measurements. Cleft Palate Craniofac J 29(4):301–302
Frühwald J, Schicho KA, Figl M, Benesch T, Watzinger F, Kainberger F (2008) Accuracy of craniofacial measurements: computed tomography and three-dimensional computed tomography compared with stereolithographic models. J Craniofac Surg 19(1):22–26
Gault DT, Renier D, Marchac D, Jones BM (1992) Intracranial pressure and intracranial volume in children with craniosynostosis. Plast Reconstr Surg 90(3):377–381
Haberl H, Hell B, Zockler MJ, Zachow S, Lamecker H et al (2004) Technical aspects and results of surgery for craniosynostosis. Zentralbl Neurochir 65(2):65–74
Hayward R, Britto JA, Dunaway D, Evans R, Jeelani N, Thompson D (2015) Raised intracranial pressure and nonsyndromic sagittal craniosynostosis. J Neurosurg Pediatr 16(3):346–348
Hilling DE, Mathijssen IM, Mulder PG, Vaandrager JM (2006a) Long-term aesthetic results of frontoorbital correction for frontal plagiocephaly. J Neurosurg 105(1 Suppl):21–25
Hilling DE, Mathijssen IM, Vaandrager JM (2006b) Aesthetic results of fronto-orbital correction in trigonocephaly. J Craniofac Surg 17(6):1167–1174
Kapp-Simon KA, Simon DJ, Kristovich S (1992) Self-perception, social skills, adjustment, and inhibition in young adolescents with craniofacial anomalies. Cleft Palate Craniofac J 29(4):352–356
Kapp-Simon KA, Speltz ML, Cunningham ML, Patel PK, Tomita T (2007) Neurodevelopment of children with single suture craniosynostosis: a review. Childs Nerv Syst 23(3):269–281
Kapp-Simon KA, Collett BR, Barr-Schinzel MA, Cradock MM, Buono LA et al (2012) Behavioral adjustment of toddler and preschool-aged children with single-suture craniosynostosis. Plast Reconstr Surg 130(3):635–647
Kolar JC, Salter EM (1997) Preoperative anthropometric dysmorphology in metopic synostosis. Am J Phys Anthropol 103(3):341–351
Macintosh C, Wall S, Leach C (2007) Strabismus in unicoronal synostosis: ipsilateral or contralateral? J Craniofac Surg 18(3):465–469
Macintosh C, Wells R, Johnson D, Wall S (2011) What are the effects of metopic synostosis on visual function? J Craniofac Surg 22(4):1280–1283
Marcus JR, Domeshek LF, Das R, Marshall S, Nightingale R et al (2008) Objective three-dimensional analysis of cranial morphology. Eplasty 8:e20
Martini M, Rohrig A, Wenghoefer M, Schindler E, Messing-Junger AM (2014) Cerebral oxygenation and hemodynamic measurements during craniosynostosis surgery with near-infrared spectroscopy. Childs Nerv Syst 30(8):1367–1374
Martini M, Schulz M, Rohrig A, Nadal J, Messing-Junger M (2015) A 3D morphometric follow-up analysis after frontoorbital advancement in non-syndromic craniosynostosis. J Craniomaxillofac Surg 43(8):1428–1437
McCarthy JG, Glasberg SB, Cutting CB, Epstein FJ, Grayson BH et al (1995a) Twenty-year experience with early surgery for craniosynostosis: I. Isolated craniofacial synostosis–results and unsolved problems. Plast Reconstr Surg 96(2):272–283
McCarthy JG, Glasberg SB, Cutting CB, Epstein FJ, Grayson BH et al (1995b) Twenty-year experience with early surgery for craniosynostosis: II. The craniofacial synostosis syndromes and pansynostosis–results and unsolved problems. Plast Reconstr Surg 96(2):284–295
McKay DR, Davidge KM, Williams SK, Ellis LA, Chong DK et al (2010) Measuring cranial vault volume with three-dimensional photography: a method of measurement comparable to the gold standard. J Craniofac Surg 21(5):1419–1422
Mendonca DA, White N, West E, Dover S, Solanki G, Nishikawa H (2009) Is there a relationship between the severity of metopic synostosis and speech and language impairments? J Craniofac Surg 20(1):85–88
Raybaud C, Di Rocco C (2007) Brain malformation in syndromic craniosynostoses, a primary disorder of white matter: a review. Childs Nerv Syst 23(12):1379–1388
Renier D, Lajeunie E, Arnaud E, Marchac D (2000) Management of craniosynostoses. Childs Nerv Syst 16(10–11):645–658
Schaaf H, Malik CY, Streckbein P, Pons-Kuehnemann J, Howaldt HP, Wilbrand JF (2010a) Three-dimensional photographic analysis of outcome after helmet treatment of a nonsynostotic cranial deformity. J Craniofac Surg 21(6):1677–1682
Schaaf H, Pons-Kuehnemann J, Malik CY, Streckbein P, Preuss M et al (2010b) Accuracy of three-dimensional photogrammetric images in non-synostotic cranial deformities. Neuropediatrics 41(1):24–29
Schaller BJ, Filis A, Merten HA, Buchfelder M (2012) Premature craniosynostosis–the role of skull base surgery in its correction. A surgical and radiological experience of 172 operated infants/children. J Craniomaxillofac Surg 40(3):195–200
Selber JC, Brooks C, Kurichi JE, Temmen T, Sonnad SS, Whitaker LA (2008) Long-term results following fronto-orbital reconstruction in nonsyndromic unicoronal synostosis. Plast Reconstr Surg 121(5):251e–260e
Shah MN, Kane AA, Petersen JD, Woo AS, Naidoo SD, Smyth MD (2011) Endoscopically assisted versus open repair of sagittal craniosynostosis: the St. Louis Children’s Hospital experience. J Neurosurg Pediatr 8(2):165–170
Thompson DN, Malcolm GP, Jones BM, Harkness WJ, Hayward RD (1995) Intracranial pressure in single-suture craniosynostosis. Pediatr Neurosurg 22(5):235–240
van der Meulen J (2012) Metopic synostosis. Childs Nerv Syst 28(9):1359–1367
Vinchon M, Pellerin P, Guerreschi P, Baroncini M, Dhellemmes P (2012) Atypical scaphocephaly: a review. Childs Nerv Syst 28(9):1319–1325
Whitaker LA, Bartlett SP, Schut L, Bruce D (1987) Craniosynostosis: an analysis of the timing, treatment, and complications in 164 consecutive patients. Plast Reconstr Surg 80(2):195–212
Wilbrand JF, Szczukowski A, Blecher JC, Pons-Kuehnemann J, Christophis P et al (2012) Objectification of cranial vault correction for craniosynostosis by three-dimensional photography. J Craniomaxillofac Surg 40(8):726–730
Wong JY, Oh AK, Ohta E, Hunt AT, Rogers GF et al (2008) Validity and reliability of craniofacial anthropometric measurement of 3D digital photogrammetric images. Cleft Palate Craniofac J 45(3):232–239
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Section Editor information
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this entry
Cite this entry
Messing-Jünger, M. (2020). Management of Craniosynostosis: Evaluation of Results. In: Di Rocco, C., Pang, D., Rutka, J. (eds) Textbook of Pediatric Neurosurgery. Springer, Cham. https://doi.org/10.1007/978-3-319-72168-2_69
Download citation
DOI: https://doi.org/10.1007/978-3-319-72168-2_69
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-72167-5
Online ISBN: 978-3-319-72168-2
eBook Packages: MedicineReference Module Medicine